Translate this page into:
Linear nodulo-ulcerative lesions on the leg in an elderly male
Corresponding author: Dr. Vishalakshi Viswanath, Department of Dermatology, Rajiv Gandhi Medical College and Chhatrapati Shivaji Maharaj Hospital, Thane Municipal Corporation, Thane, India. visha1967@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jethwa M, Viswanath V, Sakhadeo U, Kori S. Linear nodulo-ulcerative lesions on the leg in an elderly male. Indian J Dermatol Venereol Leprol. 2024;90:673-5. doi: 10.25259/IJDVL_729_2023
An 86-year-old man presented with multiple swelling on the left lower leg for the last 2 months, which began as small papular lesions and gradually increased in size and number. There was no history of weight loss or fever. His personal, past and family histories were unremarkable.
On cutaneous examination, there were seven, linear skin-coloured to erythematous, indurated nodules of 3 × 3 to 8 × 6 cm size with central ulceration and adherent black crusting on the medial aspect of the left leg with bilateral inguinal lymphadenopathy [Figure 1].

- Nodulo-ulcerative lesions of various sizes with adherent black crusting and pus discharge on the medial aspect of the leg.
Routine blood tests, peripheral smear, chest X-ray, electrocardiogram (ECG), 2D Echocardiogram (ECHO), ultrasonography (USG) of the abdomen and Computerised tomography (CT) scan of the chest and abdomen were normal. Other tests like lactate dehydrogenase, serum B12, folate, vitamin D3, iron/Total iron-binding capacity (TIBC) were within normal limits, and viral markers were non-reactive.
A wedge biopsy was done and sent for histopathological and immunohistochemical (IHC) examination [Figures 2–5].
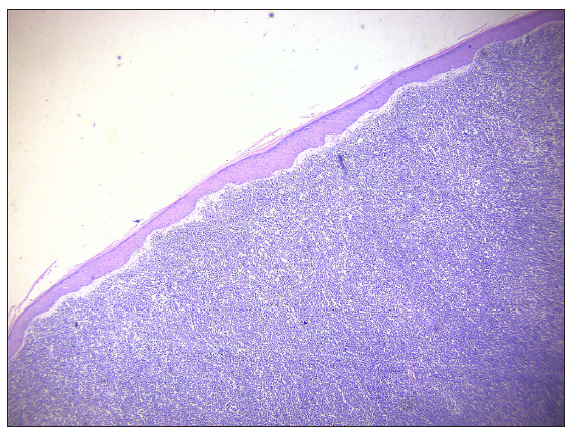
- Atrophic epidermis with distinct grenz zone and diffuse monotonous infiltrate of atypical lymphoid cells encompassing the entire dermis (Haematoxylin and Eosin, 100x).
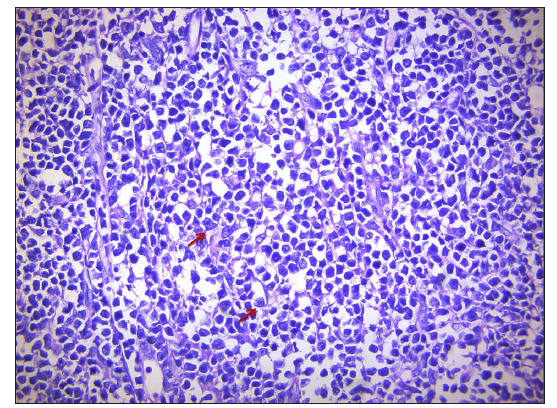
- Neoplastic lymphoid infiltrate composed of medium to large-sized cells in interstitial and perivascular area with round nuclear counter and distinct nucleoli (red arrows) and coarse chromatin (Haematoxylin and Eosin, 400x).
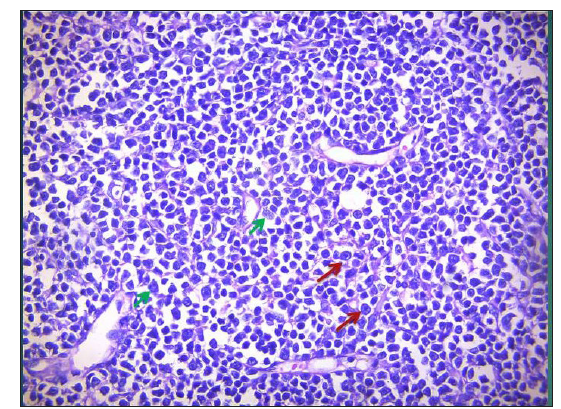
- Diffuse dermal infiltrate of distinct centroblasts (multiple nucleoli C-shaped, green arrows) and immunoblasts (single i-nucleoli with peripheral clear cytoplasm, red arrows) (Haematoxylin and Eosin, 400x).
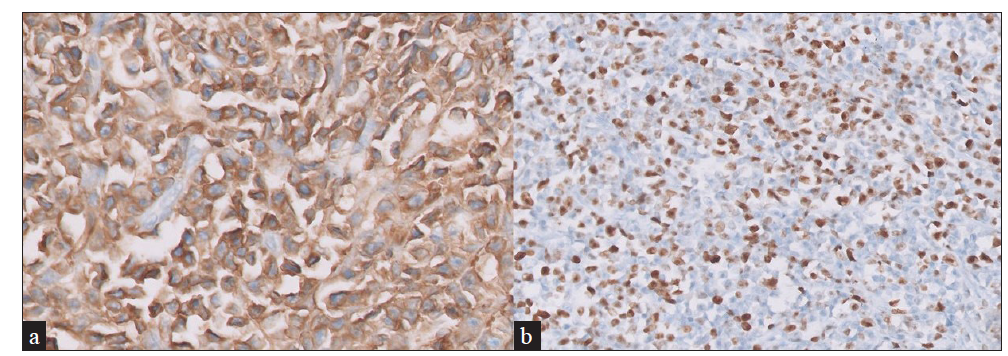
- Immunohistochemistry (IHC) showing (a) CD 20+ diffuse strong expression (IHC-CD20, 40x) (b) MIB1 positive (IHC-MIB1, 40x). MIB1: mindbomb E3 ubiquitin protein ligase 1.
Histopathology showed a distinct Grenz zone with diffuse dermal infiltrate of neoplastic lymphoid cells, centroblasts (C- shaped nucleoli) and immunoblasts (i-shaped nucleoli) [Figures 2, 3 and 4]. IHC showed diffusely positive CD20; BCL2, CD10 positivity, focal and weak positivity for MUM1, and MIB1 index 60–70% [Figure 5]. Positron emission tomography (PET) showed hypermetabolic ulcerative lesions up to intermuscular planes of the left distal leg and low-grade F-18 fluorodeoxyglucose (FDG)-avid left popliteal, inguinal and left pelvic nodes.
Question
What is your diagnosis?
Diagnosis
Primary Cutaneous diffuse large B-cell lymphoma, leg type [stage IIE (E-skin), limited to skin, NCCN IPI-4 (H-I Risk), CNS IPI-2 (IR)].
Treatment
The patient was referred to a higher centre, and started on R-CHOP regimen (single dose 500 mg IV Rituximab along with cyclophosphamide, doxorubicin, vincristine, prednisolone) for 6 cycles.
Discussion
Primary cutaneous lymphomas are a heterogenous group of extranodal non-Hodgkin lymphomas originating in the skin without evidence of extracutaneous disease. Primary cutaneous B-cell lymphomas (pcBCLs) account for 25% of all cases.1
The incidence of pcBCL has been increasing and is currently about 4 per million persons. It is common in males over 70 years of age.1,2
As per the 2016 revision of the World Health Organisation (WHO), classification of lymphoid neoplasms includes three main types of pcBCL: primary cutaneous marginal zone lymphoma (pcMZL), primary cutaneous follicle centre lymphoma (pcFCL) and primary cutaneous diffuse large B-cell lymphoma (pcDLBCL)-leg-type (LT), as well as intravascular large B-cell lymphoma (IVLBCL).3
Distinct key features of all clinical subtypes of pcBCLS are discussed in Table 1.1
| Marginal zone lymphoma | Follicle centre cell lymphoma | Diffuse large B-cell lymphoma, leg type | |
|---|---|---|---|
| Clinical features | Solitary or multiple papules,plaques, or nodules | Solitary, grouped, or multiple papules, plaques, or nodules | Solitary or multiple plaques and tumours |
| Site | Trunk and upper extremities | Head, neck, and trunk | Legs and rarely at other sites |
| Age group | Younger patients (median age, 55 years) | Elderly patients (median age, 60 years) | Elderly patients (median age, 76 years) |
| Relapse | Frequent cutaneous relapses (40%), rarely extracutaneous |
Cutaneous relapses in (20%), Extracutaneous in 5–10% |
Frequent relapses and extracutaneous dissemination |
| Histopathology | Patchy periadnexal or diffuse infiltrates of small B cells lymphoplasmacytoid cells and plasma cells |
Follicular, nodular, or diffuse infiltrates, Centrocytes and centroblast |
Diffuse infiltrates, Centroblasts and immunoblasts |
| IHC* | BCL2+, BCL6-, CD10- | BCL6+, CD20+, BCL2- | Ki-67, BCL-2+, MUM1+ |
| 5-year survival rate (%) | 99 | 95 | 50 |
pcDLBCL-LT affects elderly females and clinically presents as single-to-multiple erythematous to violaceous tumours or nodules on the leg, with 10 to 15% on non-leg locations like the head and trunk.
Other clinical differential diagnoses of leg type could be pseudolymphoma, lymphomatoid granulomatosis, Burkitt’s lymphoma, deep fungal infection, nodular sarcoid, and other types of B-cell lymphoma. Histopathology shows diffuse infiltrates with the presence of centroblasts and immunoblasts. On IHC, the presence of Multiple myeloma oncogene-1 (MUM1) indicates an aggressive course.
The first-line treatment for pcDLBCL-LT with extracutaneous spread is chemotherapy combined with intravenous or intralesional rituximab (R-CHOP), which shows a good response rate with a longer disease-free interval. Other options are lenalidomide and radiotherapy.4
Spontaneous regression of the pcDLBCL-LT tumour after biopsy has been rarely reported.5 The prognosis is unfavourable if multiple lesions are on the legs and the age is more than 75 years. There is a high chance of relapse and extracutaneous spread, and the 5-year survival rate is approximately 50%.1 Hence, early recognition and awareness regarding this subtype are needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cutaneous B-cell lymphoma. Hematol Oncol Clin North Am. 2019;33:149-61.
- [CrossRef] [PubMed] [Google Scholar]
- Changing incidence trends of cutaneous B-cell lymphoma. J Invest Dermatol. 2014;134:840-42.
- [CrossRef] [PubMed] [Google Scholar]
- The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375-90.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Innovative therapeutic approaches in primary cutaneous B cell lymphoma. Front Oncol. 2020;10:1163.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Spontaneous regression of primary cutaneous diffuse large B-cell lymphoma, leg type after biopsy. Indian J Dermatol Venereol Leprol. 2023;89:110-13.
- [CrossRef] [PubMed] [Google Scholar]






