Translate this page into:
Linear perforating lesions in dystrophic epidermolysis bullosa: Is it Koebner's phenomenon?
Correspondence Address:
Devinder Mohan Thappa
Department of Dermatology and STD, JIPMER, Pondicherry - 605 006
India
| How to cite this article: Nath AK, Thappa DM, Varma SK. Linear perforating lesions in dystrophic epidermolysis bullosa: Is it Koebner's phenomenon?. Indian J Dermatol Venereol Leprol 2010;76:724 |
Sir,
Dystrophic epidermolysis bullosa (DEB) is a rare, inherited, blistering disease caused by mutations in a single gene, COL7A1, which encodes the anchoring fibril protein, type VII collagen. [1] DEB has two main subtypes: the more aggressive autosomal recessive type and much less severe dominant type. Besides the typical skin lesions, the dominant DEB may also have congenital absence of skin (Bart syndrome), atopic dermatitis, prurigo-like nodules, and albo-papuloid lesions. [2] The presence of perforating skin lesions in patients with DEB is unknown in the English literature. We hereby report a case of dominant DEB showing linearly disposed perforating lesions at various body sites and propose a plausible hypothesis for such occurrence.
A 4.5-year-old male child was brought with a history of spontaneous as well as trauma-induced blistering in both hands and feet since birth. Loss of nails due to blistering was also noted from early infancy. There was history of blistering in the oral mucosa and development of abnormal teeth, but no history of blistering elsewhere. Multiple, itchy, hyperpigmented, raised, linear lesions developed in the lower abdomen, inguinal region, groins, both axillae, popliteal fossae, wrists, ankles, dorsa of hands and feet from early infancy. His parents were second degree consanguineous. No one else in the family had similar problem. On examination, multiple bullae (some pus-filled) and crusted ulcers were seen in both palms and palmar aspects of the fingers [Figure - 1]a. Scarring and atrophy were also seen in the palms and fingers, being more prominent in the tips of the fingers. Well-defined areas of hyperkeratosis were present over both the heels and lateral aspects of the forefeet [Figure - 1]a. Fissures were seen on the medial aspect of left foot and toe clefts. An attenuated and dystrophic nail was seen in the right thumb. Remaining digits showed complete absence of the nail plate, with scarring and atrophy of the nail beds [Figure - 1]b. Mild contractures and resorption of the terminal phalanges of the fingers were also observed. Upper incisors were deformed and showed enamel defects. These features were consistent with dominant DEB. There were multiple, 2-5 mm sized, hyperkeratotic papules in the extensor aspects of bilateral elbows, knees, dorsa of hands, ankles, and dorsa of feet [Figure - 1]b. Some of the papules showed a central keratotic plug, removal of which revealed a crater. Linear hyperkeratotic streaks were present in the lower abdomen, inguinal region, groin [Figure - 2], bilateral popliteal fossae, axillae, ankles [Figure - 1]b, dorsa of hands and feet. Other cutaneous, hair and systemic examinations were within normal limits. Histopathology of the skin biopsy from the linear hyperkeratotic lesions showed acanthosis, transepidermal elimination of basophilic, degenerated collagen and elastic tissue materials admixed with inflammatory cell infiltrates [Figure - 3]. These findings were consistent with acquired perforating dermatosis. A final diagnosis of dominant DEB associated with perforating dermatosis was made. Topical tretinoin was prescribed for the perforating skin lesions, and care for epidermolysis bullosa was explained.
 |
| Figure 1 :(a) Multiple bullae, crusted ulcers, scarring, and atrophy on the palms and fingers, along with hyperkeratosis of both soles; (b) absence of finger and toe nails with scarring of the nail beds, linear hyperkeratotic streaks over the ankles and wrists, and hyperkeratotic papules with central keratotic plug over the dorsa of hands and feetd |
 |
| Figure 2 :Linear hyperkeratotic streaks in the lower abdomen, inguinal region, and groins |
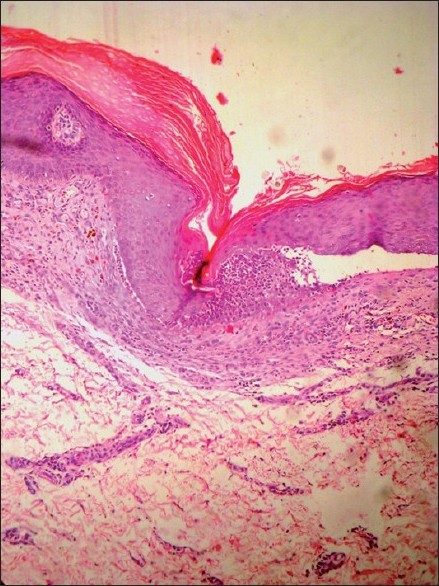 |
| Figure 3 :Photomicrograph shows acanthosis, with transepidermal elimination of basophilic, degenerated collagenous and elastic tissue materials admixed with inflammatory cell infiltrates (H and E, ×100) |
All forms of DEB are characterized by skin fragility, blistering, scarring, nail changes and milia formation. [3] The essential feature of dominant DEB is that the skin is generally less fragile than the recessive type, and blisters mostly develop over bony prominences (such as the knees and ankles, and dorsa of the hands or feet) following sharp blows. [2] The Cockayne-Touraine variety of dominant DEB is usually localized only to the extremities and is the milder expression of the blistering disease process, while the Pasini variant has more intense blistering and is more generalized. [3] The most consistent findings of DEB are localized scarring with milia formation and dystrophic nails. [2] Nail dystrophy is probably the most important diagnostic feature of the disease. [2]
Perforating disorders are a group of disorders characterized by extrusion of altered dermal components through a transepithelial channel. [4] There are four primary perforating disorders, i.e. Kyrle′s disease, perforating folliculitis, reactive perforating collagenosis, and perforating serpiginous elastosis. [5] However, many cases occur secondary to some underlying disease, such as granuloma annulare or PXE. Similar skin lesions noted in patients with diabetes and renal failure have been called acquired perforating dermatosis. [5] Occasionally, topically applied chemicals or intradermal injection can be eliminated by the transepidermal route to produce a perforating disorder. [5] Koebnerization is known to occur in almost all the perforating disorders with maximum prevalence in reactive perforating collagenosis. [4],[6] The perforating skin lesions in our case were like those of acquired perforating dermatosis. We considered elastosis perforans serpiginosa but ruled it out because lesions were not in typical serpiginous or arcuate in arrangement. [7]
The reason for occurrence of perforating lesions in DEB is at best hypothetical in our case. DEB could have been the underlying factor for abnormal alteration of dermal components followed by subsequent extrusion of the "altered" dermal elements through transepithelial channel. It was an interesting observation in our case that most of the skin areas affected by linear lesions never had blisters of DEB. It raises the possibility that alteration of upper dermal elastic tissue could have occurred in the apparently normal looking skin. The unique features in our patient were the linear arrangement of the perforating lesions, predominantly involving the flexural skin. The linear arrangement of perforating lesions could have been due to Koebnerization as the lesions were itchy. However, no atopic background was noted in our case.
| 1. |
Horn HM, Tidman MJ. The clinical spectrum of dystrophic epidermolysis bullosa. Br J Dermatol 2002;146:267-74.
[Google Scholar]
|
| 2. |
Eady RAJ, Fine JD, Burge SM. Genetic blistering diseases. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Science; 2004. p. 1-40.
th ed. Oxford: Blackwell Science; 2004. p. 1-40.'>[Google Scholar]
|
| 3. |
Burkhart CG, Ruppert ES. Dystrophic epidermolysis bullosa. Clin Pediatr (Phila) 1981;20:493-6.
[Google Scholar]
|
| 4. |
Rapini RP. Perforating Diseases. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. Spain: Mosby Elsevier; 2008. p. 1461-17.
[Google Scholar]
|
| 5. |
Burrows NP, Lovell CR. Disorders of Connective Tissue. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. Oxford: Blackwell Science; 2004. p. 64-7.
th ed. Oxford: Blackwell Science; 2004. p. 64-7.'>[Google Scholar]
|
| 6. |
Thappa DM. The isomorphic phenomenon of Koebner. Indian J Dermatol Venereol Leprol 2004;70:187-9.
[Google Scholar]
|
| 7. |
Mehta RK, Burrows NP, Payne CM, Mendelsohn SS, Pope FM, Rytina E. Elastosis perforans serpiginosa and associated disorders. Clin Exp Dermatol 2001;26:521-4.
[Google Scholar]
|
Fulltext Views
2,120
PDF downloads
3,348





