Translate this page into:
Localised urticarial eruption overlying thrombophlebitis
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Khan I, Sharma A, Khandpur S. Localised urticarial eruption overlying thrombophlebitis. Indian J Dermatol Venereol Leprol 2023;89:114-6.
Sir,
Chronic urticaria is classified into spontaneous and inducible forms. Spontaneous urticaria occurs largely in a generalised distribution, whereas inducible urticaria may be localised as per the responsible trigger. The pathophysiology of urticaria is centered around the release of histamine by mast cell degranulation, which in turn is associated with a multitude of immunologic and non-immunologic triggers. The activation of the coagulation system has also been proposed as an alternate mechanism in the pathophysiology of chronic urticaria.1 We describe an interesting case of chronic urticaria localised to the site of superficial thrombophlebitis, strengthening the above role in this condition.
A 44-year-old woman presented to our outpatient department with complaints of daily episodes of itchy urticarial wheals limited to the flexural aspect of the right upper limb for the last nine months [Figure 1a and b]. The wheals resolved within an hour of intake of tablet levocetirizine 5 mg without any residual pigmentation. There were no urticarial wheals at other sites concurrently or in the past. There was no history of angioedema, topical applications, localised pressure, cold, heat or sun exposure or contact with water. Dermographism could not be elicited.

- Subtle urticarial wheal seen over the medial aspect of the right upper limb at presentation

- Photograph shared by the patient, showing frank urticarial wheals over the same site
Two months prior to the onset of urticaria, there was a history of spontaneous development of a linear, tender and erythematous plaque over the proximal flexor aspect of the right forearm. Doppler ultrasonography revealed a hyperechoic thrombus in the underlying basilic vein, suggestive of superficial thrombophlebitis [Figure 2]. There was no history of recent intravenous cannulation, injury, surgery or prolonged immobility and no known hypercoagulability or other comorbidities. She was not on oral contraceptive pills or any other drugs. Obstetric history was significant for two consecutive embryonic losses at less than 10 weeks of gestation. Antiphospholipid antibodies revealed a positive β2-glycoprotein IgM antibody on one occasion, but negative when repeated at 12 weeks; while lupus anti-coagulant and anti-cardiolipin antibodies were negative. Thus, the modified Sapporo criteria for antiphospholipid antibody syndrome were not fulfilled in this case. She was treated with warfarin 6 mg with aspirin 75 mg daily, which led to the resolution of thrombophlebitis on doppler ultrasonography within one week. However, two months later, she began to develop urticarial wheals limited to the approximate distribution of the basilic vein, which have continued for the past nine months.
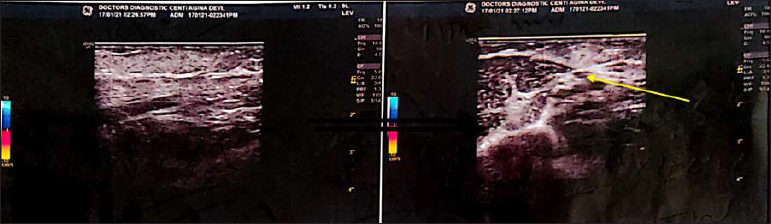
- Colour Doppler showing hyperechoic thrombus (yellow arrow) in a subcutaneous vessel on right upper arm and forearm without any colour flow
Chronic urticaria has been shown to have multi-faceted pathophysiology with mast cell degranulation being the central event in the pathogenesis. Among the immunological triggers, anti-IgE and anti-FcR1 autoantibodies and complement C5a are known to be important. However, only 50% of the patients have found to be positive for histamine-releasing autoantibodies (anti-IgE IgG) on enzyme immunoassay.2 Fagiolo et al. showed that serum from patients containing anti-FcRI autoantibodies lost the ability to release histamine from basophils in vitro, yet retained the ability to induce a wheal and flare reaction upon autologous serum injection even being heat-decomplemented/IgG depleted. Hence, there could be other non-immunoglobulin serum reactants that could lead to wheal and flare reactions in patients with chronic urticaria.3
It has been postulated that activation of the extrinsic coagulation pathway is one of the triggers for mast cell degranulation. Chronic urticaria patients show raised levels of prothrombin fragments 1+2 (PF1+2, a by-product of the conversion of prothrombin to thrombin), factor VIIa, fibrin degradation products and d-dimer, with their level having a positive correlation with urticaria severity.4 Thrombin has been found to facilitate mast cell adhesion to fibronectin and mast cell degranulation. It can also increase vascular permeability and hence can act as a trigger for urticaria.5 Thrombin injection for the treatment of pseudoaneurysm has been reported to induce a prolonged urticarial reaction6 and is also generated during attacks of hereditary angioedema.
The induction of tissue factors involved in the extrinsic coagulation pathway has also been associated with mast cell degranulation.7 Cugno et al. found eosinophils to be the main source of tissue factors, which are also the main inflammatory cells in urticaria.8 Tissue factor, along with factor VIIa, leads to activation of factor IIa and factor Xa, which, in turn, increases the vascular permeability via protease-activated receptor-1 and cause mast cell degranulation by activation of the C5 complement.9 There have been multiple reports and trials of successful use of heparin, warfarin and tranexamic acid in patients with chronic urticaria refractory to conventional treatment. A combination of low molecular weight heparin and tranexamic acid was successfully used by Asero et al. in patients with raised d-dimer levels, who also found that raised d-dimer levels correlated with non-responsiveness to anti-histamines.10
Our case demonstrates an interesting direct clinical association of thrombosis with localised urticaria; strengthening the existing laboratory and circumstantial evidence correlating urticaria and the coagulation pathway.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Inflammation and coagulation in urticaria and angioedema. Curr Vasc Pharmacol. 2012;10:653-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and functional role of anti-IgE autoantibodies in urticarial syndromes. J Invest Dermatol. 1988;90:213-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of complement inactivation and IgG depletion on skin reactivity to autologous serum in chronic idiopathic urticaria. J Allergy Clin Immunol. 2000;106:567-72.
- [CrossRef] [PubMed] [Google Scholar]
- Coagulation/fibrinolysis and inflammation markers are associated with disease activity in patients with chronic urticaria. Allergy. 2010;65:649-56.
- [CrossRef] [PubMed] [Google Scholar]
- Thrombin induces mast cell adhesion to fibronectin: Evidence for involvement of protease-activated receptor-1. J Immunol. 2002;169:4551-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prolonged generalized urticarial reaction after percutaneous thrombin injection for treatment of a femoral artery pseudoaneurysm. J Vasc Interv Radiol. 2000;11:759-61.
- [CrossRef] [PubMed] [Google Scholar]
- Activation of the tissue pathway of blood coagulation in patients with chronic urticaria. J Allergy Clin Immunol. 2007;119:705-10.
- [CrossRef] [PubMed] [Google Scholar]
- Expression of tissue factor by eosinophils in patients with chronic urticaria. Int Arch Allergy Immunol. 2009;148:170-4.
- [CrossRef] [PubMed] [Google Scholar]
- The role of coagulation and complement factors for mast cell activation in the pathogenesis of chronic spontaneous urticaria. Cells. 2021;10
- [CrossRef] [PubMed] [Google Scholar]
- Heparin and tranexamic Acid therapy may be effective in treatment-resistant chronic urticaria with elevated d-dimer: A pilot study. Int Arch Allergy Immunol. 2010;152:384-9.
- [CrossRef] [PubMed] [Google Scholar]





