Translate this page into:
Localized cutaneous leishmaniasis in South India: Successful treatment with ketoconazole
Correspondence Address:
M Kumaresan
Department of Skin and STD, Kasturba Medical College, Mangalore - 575 001, Karnataka
India
| How to cite this article: Kumaresan M, Kumar P. Localized cutaneous leishmaniasis in South India: Successful treatment with ketoconazole. Indian J Dermatol Venereol Leprol 2007;73:361-362 |
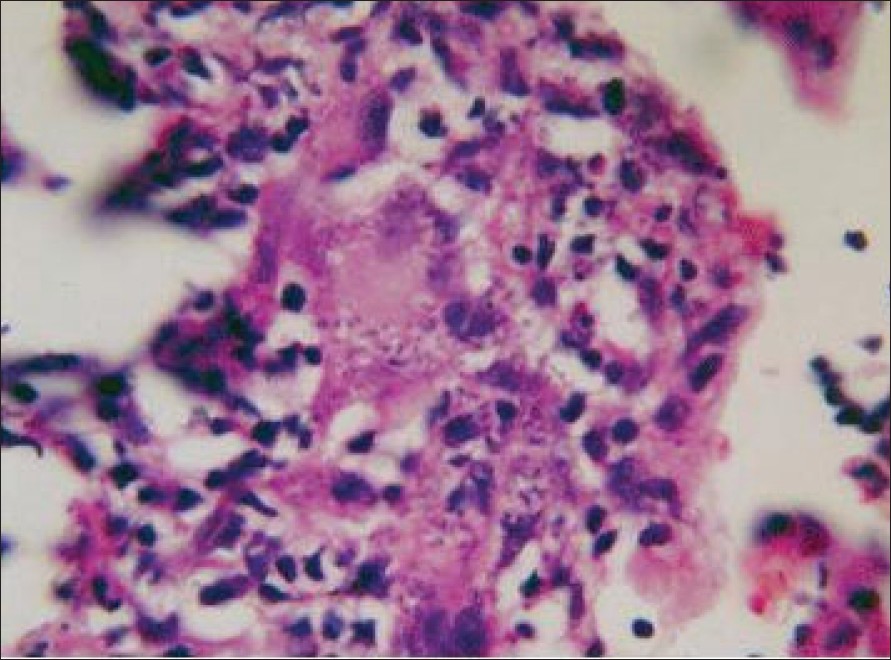 |
| Figure 3: Leishman Donovan bodies inside the macrophages (H and E, x400) |
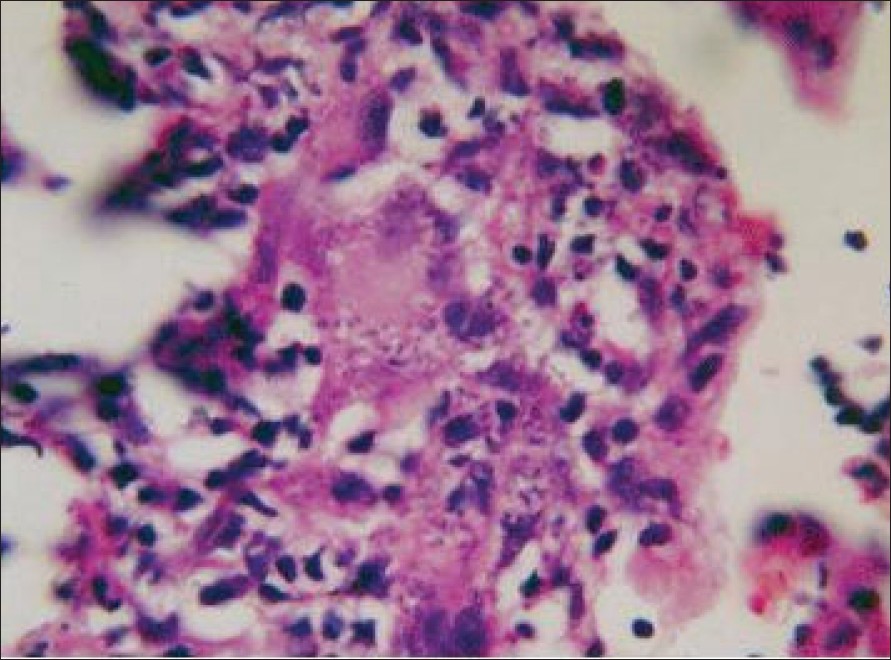 |
| Figure 3: Leishman Donovan bodies inside the macrophages (H and E, x400) |
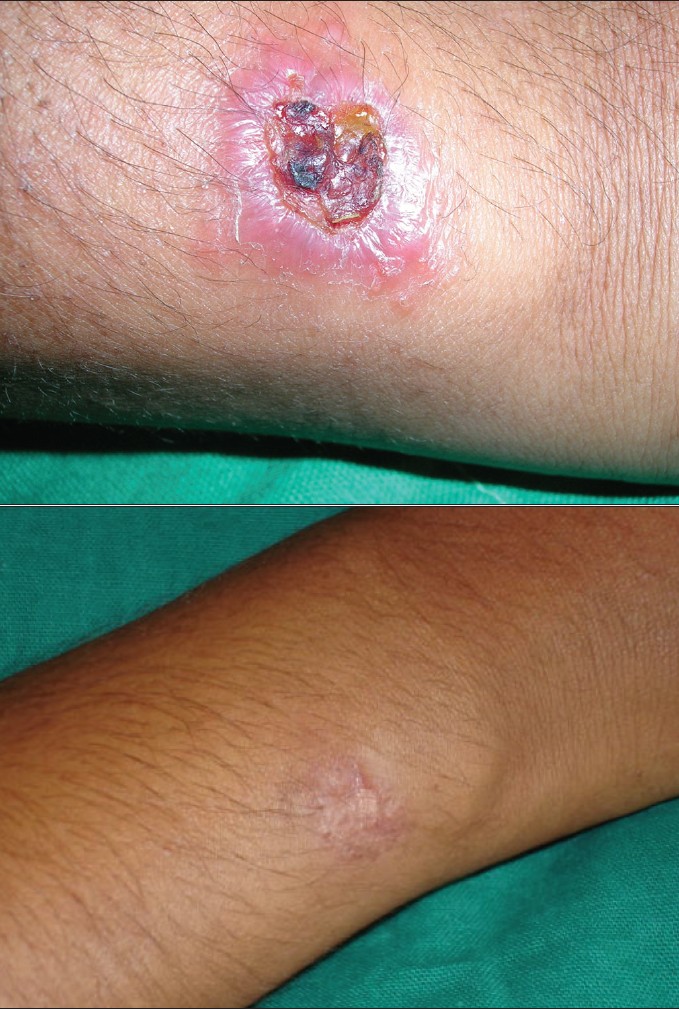 |
| Figure 2a: Case 3: Cutaneous leishamaniasis, before treatment Figure 2b: Case 3: Cutaneous leishamaniasis, after treatment |
 |
| Figure 2a: Case 3: Cutaneous leishamaniasis, before treatment Figure 2b: Case 3: Cutaneous leishamaniasis, after treatment |
 |
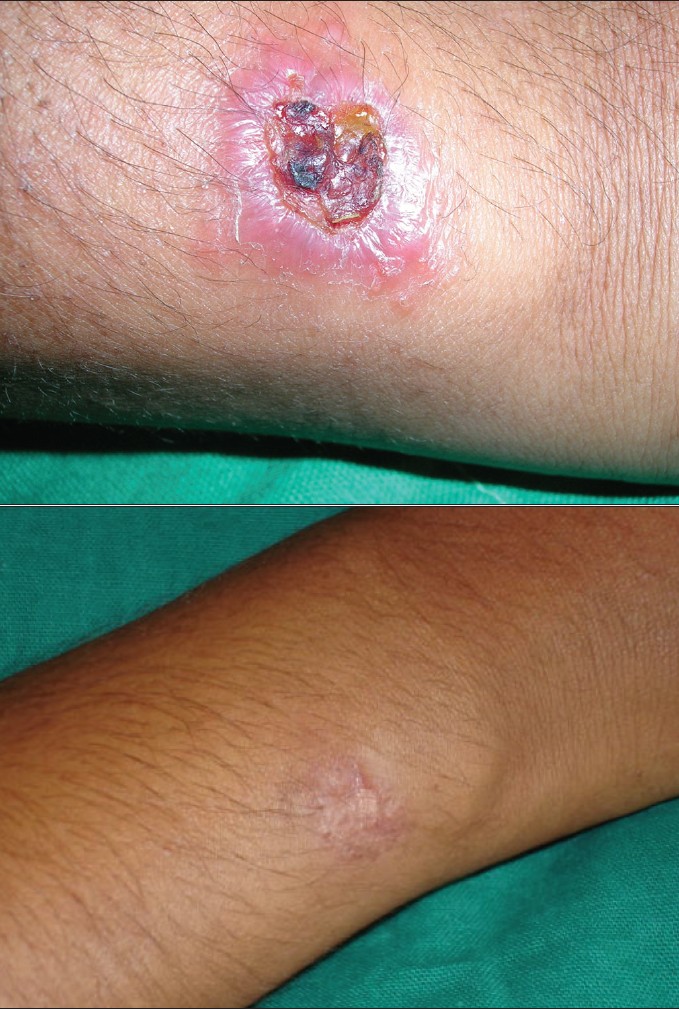
| Figure 1a: Case 2: Cutaneous leishamaniasis, before treatment Figure 1b: Case 2: Cutaneous leishamaniasis, after treatment |
 |
| Figure 1a: Case 2: Cutaneous leishamaniasis, before treatment Figure 1b: Case 2: Cutaneous leishamaniasis, after treatment |
Sir,
Leishmaniasis is a protozoal infestation caused by several species of the genus Leishmania . The disease, once restricted to certain geographical areas in India, is now showing a trend to spread to previously nonendemic areas. Hence, there are reports of new foci of infection from various parts of India. [1],[2],[3] There is no optimal treatment protocol for all forms of cutaneous leishmaniasis (CL). The therapeutic regimen for CL should be based on clinical experience and efficacy vs toxicity of the commonly used drugs in each endemic area. We report three cases of cutaneous leishmaniasis diagnosed histopathologically in a nonendemic area that are treated successfully with oral ketoconazole.
Our first case was a 39-year-old female who presented with an erythematous plaque that showed ulceration and crusting of the surface. The lesions were present over the right forearm since 2 months. The second case was a similar one: a 10-year-old boy presented with an erythematous ulcerated plaque of 3 months duration over the right cheek [Figure - 1]a . The third patient was a 20-year-old female who presented with an erythematous ulcerated plaque of 1 month duration over the right forearm [Figure - 2]a . All the three patients belonged to Kasargod district in the Western Ghats region of South India. None of them had traveled to the endemic areas for CL in the past. Cutaneous leishmaniasis was suspected in these cases on clinical grounds. In all the three patients, biopsy confirmed the diagnosis revealing LD bodies inside the macrophages [Figure - 3], although culture could not be performed. The patients were treated with oral ketoconazole (200mg twice daily for patients 1 and 3 and 100 mg once daily for patient 2) for a period of 3 months. Patients were followed up every 2 weeks. Complete hemogram, liver and renal function tests were performed for all the patients before commencing and after completion of the treatment.
At the end of 3 months of the treatment, clinical cure was observed in all the patients [Figure - 1]b, [Figure - 2]b. No adverse effect of the drug was noted at the end of the treatment period. The patients were followed up for a duration of 6 months and none of them showed recurrence. All the patients tolerated ketoconazole well.
Imidazole derivatives are potential therapeutic agents in cutaneous leishmaniasis. They act by interfering with the synthesis of ergosterol [4] that is present in large concentrations in the cell wall of Leishmania spp. The efficacy of ketoconazole in different doses for variable periods in both old and new world cutaneaous leishmaniasis has been documented in several studies. [5]
In Kerala, the cases of CL have been reported from Malappuram [1] and Trivandrum. [6] We diagnosed three cases of CL from the Kasargod district of Kerala for the first time. This is of considerable public health interest in view of a newly recognized reservoir area of CL in South India. Further investigations are required to identify the Leishmania species, reservoir and the vector in this area.
| 1. |
Bora D, Khera AK, Mittal Veena, Kaul SM, Sharma RS. New focus of cutaneaous leishmaniasis in India: Preliminary report. Indian J Dermatol Venereol Leprol 1996;62:19-21.
[Google Scholar]
|
| 2. |
Sharma RC, Mahajan VK, Sharma NL, Sharma A. A new focus of cutaneous leishmaniasis in Himachal Pradesh (India). Indian J Dermatol Venereol Leprol 2003;69:170-2.
[Google Scholar]
|
| 3. |
Kalla Gyaneshwar, Singhi MK Cutaneous Leishmaniasis in Jodhpur District. Indian J Dermatol Venereol Leprol 1996;62:149-51.
[Google Scholar]
|
| 4. |
Bergers M. Mechanism of antifungal drugs with special reference of Imidazole derivatives. Rev Infect Dis 1980;2:520-34.
[Google Scholar]
|
| 5. |
Urcuyo FG, Zaias N. Oral ketoconazole in treatment of leishmaniasis. Int J Dermatol 1982;21:414-6.
[Google Scholar]
|
| 6. |
Lohidakshan MU, Shanmugham Pillai SM, Vijayadharan M, Sarojini PA. Two cases of cutaneous leishmaniasis in Trivandrum. Indian J Dermatol Venereol Leprol 1988;54:161-2.
[Google Scholar]
|
Fulltext Views
3,676
PDF downloads
2,126





