Translate this page into:
Localized scleroderma unius lateri and Borrelia burgdoferi infection
2 Department of Neurology, "Maggiore della Carit�" Hospital, University of Eastern Piedmont "A. Avogadro". Corso Mazzini 18, Novara, Italy
3 Department of Medical Sciences, University of Trieste, Cattinara Hospital, Trieste, Italy
4 Department of Medical Sciences, "Maggiore della Carit�" Hospital, University of Eastern Piedmont "A. Avogadro". Corso Mazzini 18, Novara, Italy
Correspondence Address:
Benedetta Miglino
Clinica Dermatologica, AOU " Maggiore della Carit�", Corso Mazzini 18, 28100 Novara
Italy
| How to cite this article: Miglino B, Viana M, Zavattaro E, Bonin S, Valente G, Colombo E. Localized scleroderma unius lateri and Borrelia burgdoferi infection. Indian J Dermatol Venereol Leprol 2012;78:383-385 |
Sir,
Localized scleroderma (named also morphea) is an inflammatory autoimmune skin sclerosis of unknown etiology. A causative role of Borrelia burgdoferi infection has been proposed. [1] The B. burgdoferi infection can be assessed with serological test as well as polymerase chain reaction (PCR) on blood and skin sample. [2] Here we report the case of a Moroccan 27-year-old male, living in Italy since 10 years. In October 2010, he presented to the neurologist for progressive weakness and hypotrophy of his left limbs, which started 4 years before [Figure - 1]a. For the presence of scleroatrophic plaques on the affected areas and the left side of the trunk, he was referred to the dermatologist. Physical examination revealed multiple oval and round circumscribed areas of deep induration of the skin on the left upper and lower limbs, left half of the trunk and on the interscapular region. Sclerodermic plaques were painful, severely atrophic and hyperpigmented, adherent to the underneath tissues, with ill-defined borders, brownish color and no evidence of telangiectasia [Figure - 1]b and c. Neither erythema nor lilac ring was present. Since their appearance, they progressively increased in number and became more painful, mainly in the last 6 months. Hematochemical investigations including C3 and C4 complement factor levels, antidouble strand DNA antibodies, antibodies to extractable nuclear antigens (RNP, Sm, SS/A, SS/B), topoisomerase I (Scl/70), antisynthetasis (Jo1), IgG phospholipid units (GPL), IgM phospholipid units (MPL), C1q, antinuclear antibodies (ANAs), Weil-Felix test and B. burgdoferi serology (ELISA assay), were performed. The results were within the normal limits except for ANAs titer (4.7 index, normal values: 0.00 - 1.50 index; ANA-IIF: Positive for speckled/nucleolar type, medium positivity) and B. burgdoferi IgM (LYMEM 136.0 AU/ml; normal values: 0.0-22.0). The patient did not remember any bite in the previous months. A skin biopsy of a recent lesion on the distal third of the left thigh was performed. The histological evaluation confirmed the diagnosis of localized scleroderma [Figure - 2]. Direct immunofluorescence (DIF) analysis was negative. Nailfold capillaroscopy did not show microvascular abnormalities. PCR analyses for Borrelia detection, [2] performed on DNA obtained from peripheral blood and skin biopsy samples, were negative. The patient was then treated with benzathine penicillin intramuscular 12,000,000 IU per day for 20 days, and after 1 month, a 20 days cycle was repeated. No other medication was prescribed. After 4 months he showed a clear improvement of the symptoms and serological test for B. burgdoferi resulted negative. Physical examination showed that the plaques were softer and less adherent to the underneath tissues than before the benzathine penicillin treatment [Figure - 3].
 |
| Figure 1: (a) Clinical feature in the study patient showing striking hypotrophy of the left limbs; (b, c) Hyperpigmented atrophic plaques over the left part of the trunk and left lower limb (arrows) |
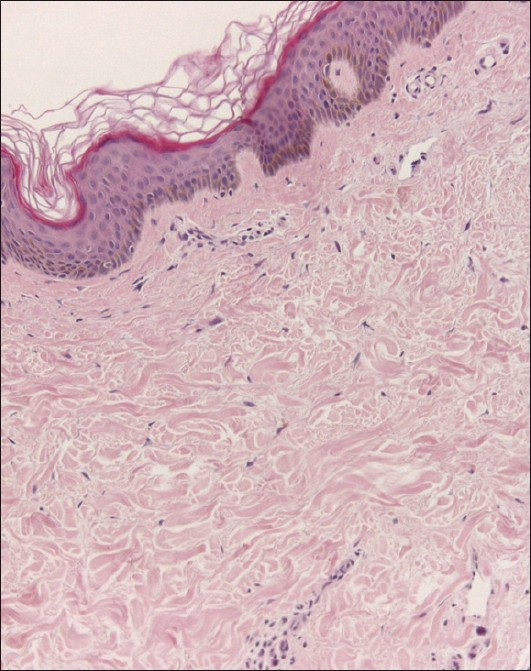 |
| Figure 2: H and E - stained section of the punch biopsy specimen showing marked sclerosis of the dermis with disordered arrangement and parallelement of collagen fibers, lack of skin appendageal structures and mild chronic inflammatory infiltration (×220 magnification) |
 |
| Figure 3: Clinical feature after benzathine - benzyl penicillin treatment: The plaques were softer, lighter in color and less adherent to the underneath tissues than before treatment |
Neurological examination showed a moderate hypotrophy of the proximal muscles of the left arm, a mild hypotrophy of the proximal muscles of the left leg and a mild diffuse strength reduction, 4 out 5 of the Medical Research Council scale (MRC scale) on the same limbs. Remaining examination was entirely normal. The neuroimaging workup (brain MRI with MRA, cervical MRI), and the neurophysiological tests (motor-evoked potential, sensory-evoked potentials, electroneurography and electromyography) were normal.
This is an interesting case of a patient with a localized scleroderma and serological signs of B. burgdoferi infection that sought medical care for neurological symptoms. Yet, he had no central or peripheral nervous system lesion. The muscle wasting and weakness were secondary to the dermatological lesions. [3] Nevertheless, B. burgdoferi detection by PCR was negative. This fact could be explained with the paucity of the bacteria, which did not reach the sensitivity of the analysis in this case. It is known, indeed that in the manifestation of long-standing infection of B. burgdoferi, the paucity of microorganisms could lead to a low detection rate by PCR, especially when the analysis is performed on archival biopsies. [4],[5] Negative results obtained by PCR did not prove the absence of the microorganism, for low sensitivity (45.2%) of the method. [4]
Nevertheless penicillin provided good results in line with previous reports on the efficacy of this treatment for localized scleroderma. [4],[5]
| 1. |
Valanciene G, Jasaitiene D, Valiukeviciene S. Pathogenesis and treatment modalities of localized scleroderma. Medicina (Kaunas) 2010;46:649-56.
[Google Scholar]
|
| 2. |
Pauluzzi P, Bonin S, Gonzalez Inchaurraga MA, Stanta G, Trevisan G. Detection of spirochaetal DNA simultaneously in skin biopsies, peripheral blood and urine from patients with erythema migrans. Acta Derm Venereol 2004;84:106-10.
[Google Scholar]
|
| 3. |
Chung L, Lin J, Furst DE, Fiorentino D. Systemic and localized scleroderma. Clin Dermatol 2006;24:374-92.
[Google Scholar]
|
| 4. |
Zollinger T, Mertz KD, Schmid M, Schmitt A, Pfaltz M, Kempf W. Borrelia in granuloma annulare, morphea and lichen sclerosus: A PCR-based study and review of the literature. J Cutan Pathol 2010;37:571-7.
[Google Scholar]
|
| 5. |
Breier FH, Aberer E, Stanek G, Khanakaha G, Schlick A, Tappeiner G. Isolation of Borrelia afzelii from circumscribed scleroderma. Br J Dermatol 1999;140:925-30.
[Google Scholar]
|
Fulltext Views
2,525
PDF downloads
1,727





