Translate this page into:
Low-dose cyclosporine for rapid remission and maintenance in recurrent Kimura's disease
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Correspondence Address:
Rashmi Kumari
Department of Dermatology and STD, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605 006
India
| How to cite this article: Gupta D, Kumari R, Rajesh NG, Manobalan K, Thappa DM. Low-dose cyclosporine for rapid remission and maintenance in recurrent Kimura's disease. Indian J Dermatol Venereol Leprol 2017;83:262-264 |
Sir,
A 66-year-old man, on regular treatment for diabetes and hypertension, presented with an asymptomatic insidious growth on the left side of the face for 15 years. Thirteen years ago, the swelling had been excised and reported as inflammatory granuloma. However, this was followed by regrowth and a partial superficial parotidectomy was done 6 years ago which was reported as benign lymphoepithelial sialadenitis. Now, the patient had presented with another recurrence. On examination, a 12 cm × 10 cm firm, diffuse, mobile, non-tender, nodular swelling was present on the left parotid region extending from the preauricular area to the angle of the mouth, becoming pendulous anteriorly. Orbital involvement was seen superiorly [Figure 1a]. Satellite nodes were not palpable. Contrast-enhanced computerised tomography showed a well-defined, large, heterogeneous lesion in the subcutaneous and muscular plane [Figure 1b]. Histopathology revealed blood vessels surrounded by lobular infiltration of lymphocytes and numerous eosinophils forming microabscesses. An infiltrate of eosinophils was seen extending into the septa of subcutaneous tissue [Figure 1c]. Immunohistochemistry for IgE was strongly positive and peripheral blood eosinophilia of 27% was also noted. The baseline renal parameters were normal. Based on clinical features and histopathology, a diagnosis of Kimura's disease was made. He was started on prednisolone 1 mg/kg/day following which the swelling regressed almost completely in 2 months [Figure - 2]. However, it relapsed every time prednisolone was tapered to a low dose. After 8 months, prednisolone was discontinued and cyclosporine A 2 mg/kg/day was initiated, followed by rapid reduction in swelling within 10 days. Blood pressure, renal function, lipid levels and electrolytes were monitored closely during therapy. Though our patient was hypertensive, he did not develop any further rise in blood pressure after starting cyclosporine A. The drug was gradually tapered and stopped within 3 months. The patient continues to be in remission 3 months after stopping cyclosporine A [Figure - 3].
 |
| Figure 1a: A 12 cm × 10 cm firm, nodular, protuberant, swelling on the left side of the facegradually |
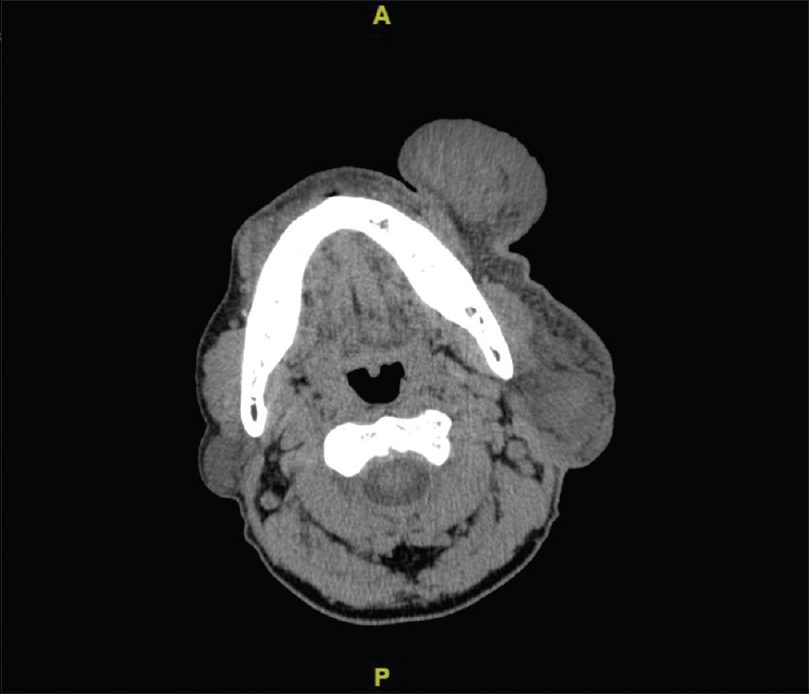 |
| Figure 1b: Contrast-enhanced computed tomography showing a well-defined lesion in subcutaneous and muscular plane near left preauricular region and body of left mandible (arrows) |
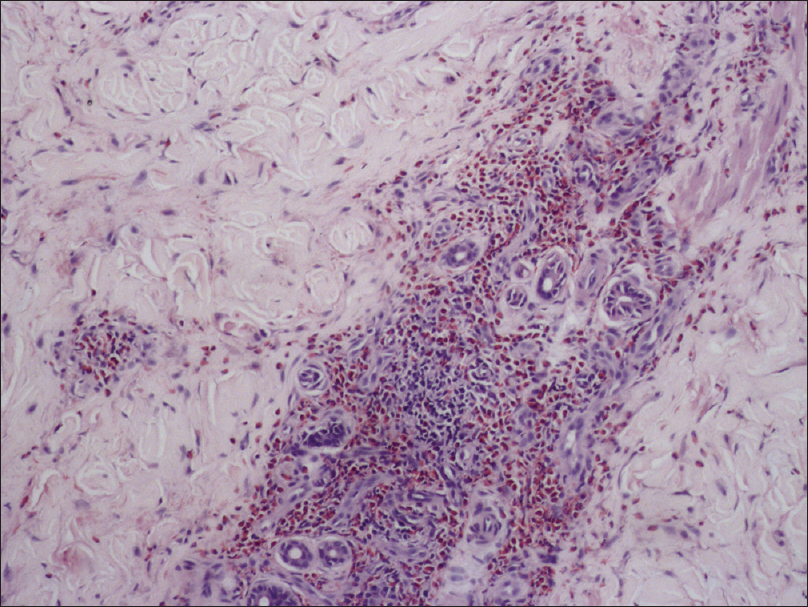 |
| Figure 1c: Blood vessels surrounded by lobular infiltration of lymphocytes and numerous eosinophils (H and E, ×200) |
 |
| Figure 2: Partial remission after treatment with oral prednisolone |
 |
| Figure 3: Near complete remission after 10 days of cyclosporine |
Kimura's disease is partly a T-helper cell 2 (Th2)-mediated disorder with overexpression of the Th2 cytokines, interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-13 (IL-13). Interleukin-5 stimulates the differentiation and activation of eosinophils and interleukin-4 and interleukin-13 initiate and enhance IgE synthesis.[1],[2] It is by targeting this interleukin pathway that cyclosporine is believed to work in Kimura's disease. It inhibits calcineurin, leading to decreased interleukin-2 production, which in turn inhibits T-cell proliferation and suppression of downstream cytokines such as interleukin-4, interleukin-5, interleukin-13 and eosinophil cationic protein in the lymph nodes and serum of Kimura's disease patients.[1],[2],[3],[4],[5] Sato et al. showed decreasing serum levels of soluble interleukin-2 receptor, interleukin-4 and interleukin-5 following treatment with cyclosporine A.[1] Cytokine levels and eosinophilia correlated with blood levels of cyclosporine and both are fully suppressed when the cyclosporine level is above 75 ng/L.2
A search of the PubMed database revealed 14 cases of Kimura's disease treated with cyclosporine A published to date, almost all of them in East Asian patients. It was noticed that most of the cases used cyclosporine A, along with steroids to induce remission, followed by cyclosporine A alone for maintenance. Furthermore, most authors have used a higher dose for treatment (3–5 mg/kg/day).
Although oral corticosteroids are the standard medical therapy of Kimura's disease, lesions often recur when steroid therapy is tapered or stopped. Moreover, doses exceeding physiologic levels for even 3–4 weeks produce clinically relevant hypothalamic–pituitary–adrenal axis suppression in addition to other side effects such as diabetes and hypertension which are irreversible. On the other hand, if cyclosporine is administered at a dose of 5 mg/kg/day or less for <2 years and serum creatinine levels are carefully monitored to ensure that they do not increase to more than 30% above baseline, renal side effects will be fully reversible after discontinuation of the drug. Intermittent therapy allows normalization of renal function between courses. Studies of short-course cyclosporine therapy show a low incidence of new-onset hypertension, ranging from 0% to 24% which is typically reversible on dose reduction or with the use of antihypertensive medications.[5]
This report is unique in that low dose (2 mg/kg/day) cyclosporine A was used as monotherapy for induction as well as maintenance for 3 months which was followed by remission of therapy for another 3 months, in which there was no relapse. We were unable to find any previous reports apart from Miki et al.[3] who used low-dose cyclosporine A for both induction and remission.
To conclude, cyclosporine is a promising nonsurgical, steroid-sparing therapeutic option for inducing rapid remission as well as maintenance for recurrent and refractory Kimura's disease. It may also serve as an alternative in patients in whom corticosteroids are otherwise contraindicated. Furthermore, low dose of cyclosporine A at 2 mg/kg/day may be without the side effects associated with long-term therapy of cyclosporine A.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sato S, Kawashima H, Kuboshima S, Watanabe K, Kashiwagi Y, Takekuma K, et al. Combined treatment of steroids and cyclosporine in Kimura disease. Pediatrics 2006;118:e921-3.
[Google Scholar]
|
| 2. |
Katagiri K, Itami S, Hatano Y, Yamaguchi T, Takayasu S.In vivo expression of IL-4, IL-5, IL-13 and IFN-gamma mRNAs in peripheral blood mononuclear cells and effect of cyclosporin A in a patient with Kimura's disease. Br J Dermatol 1997;137:972-7.
[Google Scholar]
|
| 3. |
Miki H, Tsuboi H, Kaneko S, Takahashi H, Yokosawa M, Asashima H, et al. A case of refractory Kimura disease with a buccal bulky mass successfully treated with low-dose cyclosporine A: Report and review of the literature. Allergol Int 2016;65:212-4.
[Google Scholar]
|
| 4. |
Kaneko K, Aoki M, Hattori S, Sato M, Kawana S. Successful treatment of Kimura's disease with cyclosporine. J Am Acad Dermatol 1999;41(5 Pt 2):893-4.
[Google Scholar]
|
| 5. |
Ryan C, Amor KT, Menter A. The use of cyclosporine in dermatology: Part II. J Am Acad Dermatol 2010;63:949-72.
[Google Scholar]
|
Fulltext Views
3,096
PDF downloads
1,692





