Translate this page into:
Lues maligna and HIV mimicking aggressive epidermotropic CD8+ cutaneous T-cell lymphoma
Corresponding author: Dr. Lyubomir A. Dourmishev, Department of Dermatology and Venereology, Medical University – Sofia, Bulgaria. l_dourmishev@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Petrova E, Mateeva V, Kafelova A, Saleva-Stateva M, Radeva I, Yancheva N, et al. Lues maligna and HIV mimicking aggressive epidermotropic CD8 cutaneous T-cell lymphoma. Indian J Dermatol Venereol Leprol. 2025;91:86-8. doi: 10.25259/IJDVL_203_2023
Dear Editor,
Both the human immunodeficiency virus (HIV) infection and syphilis are sexually transmitted infections (STIs) in which diagnostic challenges arise due to alterations in their natural progression when co-infecting a mutual host.1 Syphilis, a “great imitator” of skin disorders, has an extensively variable clinical appearance.2 Chancre facilitates the penetration of the viruses, while the treponemal infection activates the upregulation of transcription factors, leading to the enhancement of HIV-viral replication and the reduction of CD4 cells.3 The HIV infection impairs both humoral and cellular immunity thus modifying the defence against T. pallidum and increasing the risk of unfavourable progression.3 We observed a rare clinical manifestation of malignant syphilis in an HIV-positive patient mimicking aggressive epidermotropic CD8 cutaneous T-cell lymphoma (CTCL).
A 41-year-old Caucasian male presented with a 5-month-history of ulcerations over the face, the trunk and the upper limbs. The initial papules rapidly progressed to painless ulcers surrounded by an erythematous rim which subsequently developed haemorrhagic crusts at the periphery [Figures 1a and 1b]. The patient had fever up to 38.9°C, night sweats and arthralgia. In the last 10 days, a generalised papular rash corresponding to secondary syphilis with moderate pruritus appeared. The patient had reported promiscuity with unprotected sexual intercourse. This clinical picture was suggestive for pyoderma gangrenosum, necrotizing vasculitis, fungal and bacterial infections, or malignant cutaneous lymphoma.

- Lichenoid papular rash and ulcerative lesions with necrotic center and peripheral erythema upon admission.

- Ulcerative lesions on face.
Laboratory tests revealed mild anaemia with erythrocytes 3.9 × 109/L and haemoglobin 12.4 g/dL; and elevated fibrinogen at 4.8 g/dL; gamma-glutamyl transpeptidase 137 U/L and ESR 76 mm/h. Wound cultures revealed Staph. epidermidis. Serological findings showed strong positive rapid plasma reagin (RPR) test, RPR quantitative: 1:128 and TPHA tests. HIV 1+2 Ag/Ab ELISA was also positive and Western blot confirmed infection with HIV 1 virus. The histopathological examination from the border of an ulcerative lesion demonstrated necrosis, dense nested lymphocytic infiltrate with nuclear pleomorphism and epidermotropism consisting of the lining of small-sized lymphocytes along with the basal epidermal layer [Figures 2a and 2b]. Single plasma cells were present in the infiltrate [Figure 2c]. There were no signs of vasculitis. The immunohistochemical staining showed that the epidermotropic lymphocytes were CD3+CD8+ positive, as were the majority of cells in the dermal infiltrate [Figure 2d]. CD4 was positive in around 20% of the dermal lymphocytes, CD20 demonstrated focal positivity, CD30 was positive in single cells. This histological picture pointed to CD8+ CTCL. Upon clinicopathological correlation, given the sudden onset of ulcerative lesions and the B-symptoms, the diagnosis of CD8+ aggressive epidermotropic CTCL was considered.

- Almost complete disappearance of the lesions after treatment.
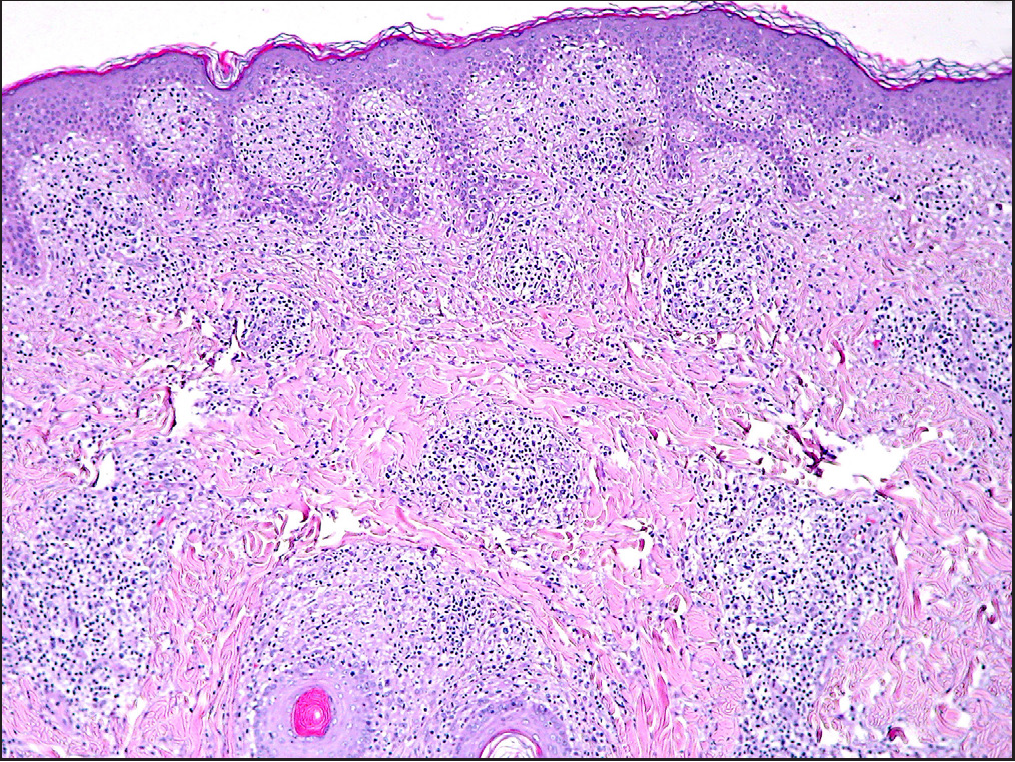
- Irregular acanthosis of the epidermis with epidermal lining of small-sized halo-lymphocytes and folliculotropism; in the dermis: dense nested lymphocytic infiltrate (Haematoxylin and eosin, 100 x).
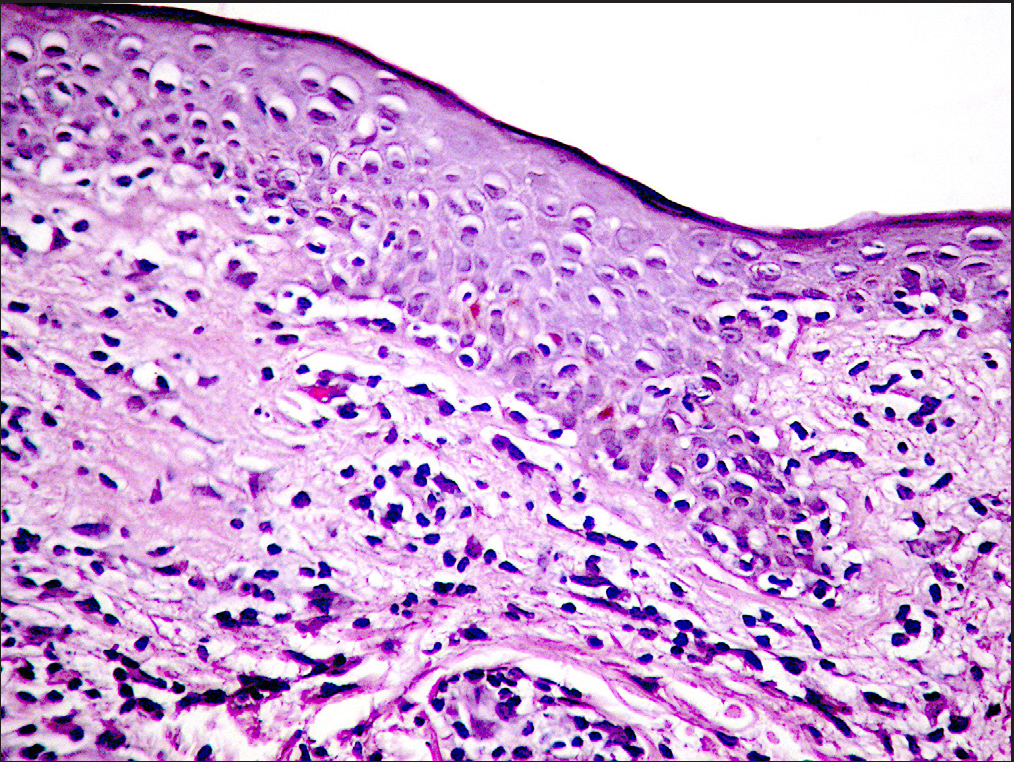
- Epidermis: epidermotropism consisting of lining of small-sized lymphocytes along the basal epidermal layer, suggestive of epidermotropic lymphoma (Haematoxylin and eosin, 400 x).
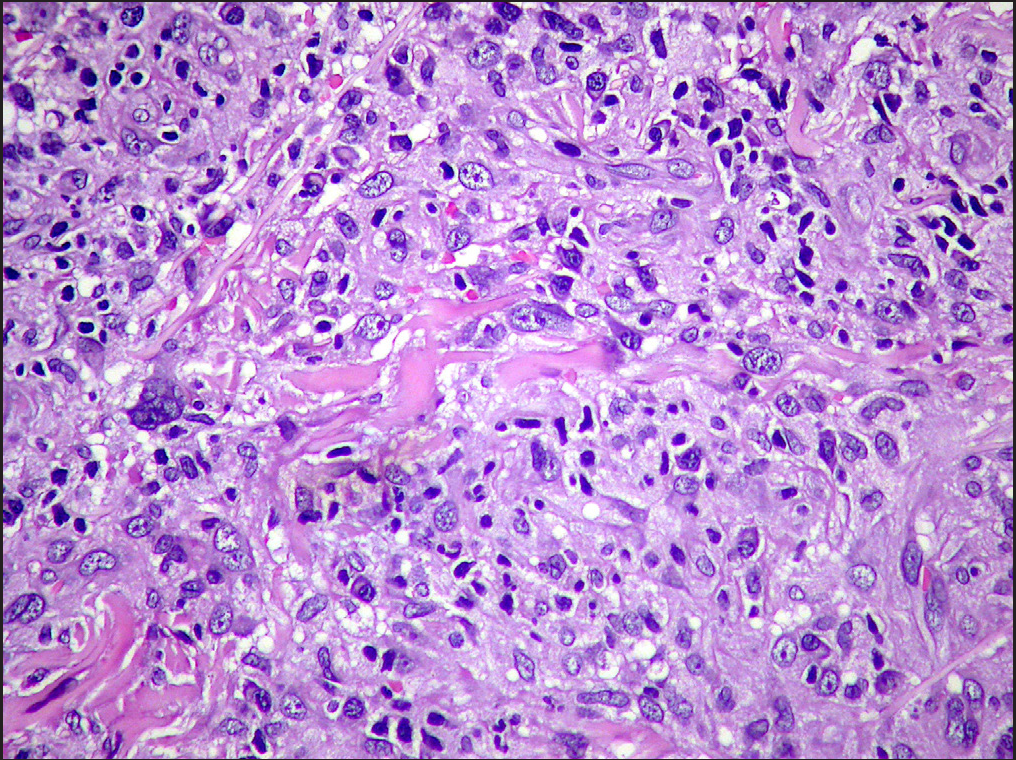
- Dermis: some of the cells of the infiltrate have irregular hyperchromatic nuclei, or with coarse chromatin and marked nuclear pleomorphism (Haematoxylin and eosin, 400 x).
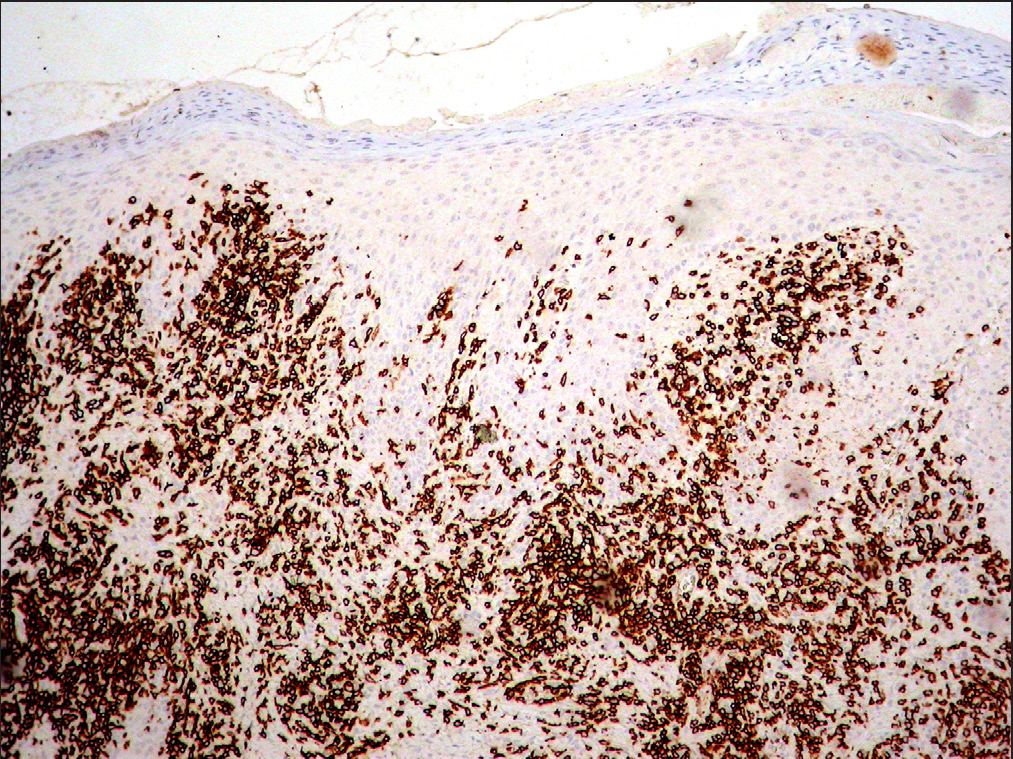
- CD8 was positive in the epidermotropic lymphocytes and in around 80% of the dermal infiltrate.
The patient underwent treatment for secondary syphilis with ceftriaxone 3g/24h for 21 days and HAART therapy for HIV with emtricitabine/tenofovir, dysoproxil fumarate and dolutegravir, resulting in an increase in the CD4 cells number above 250/mm3 in four months. At the last follow-up examination, the skin lesions had an almost complete epithelization with atrophic scars [Figure 1c]. Post-treatment RPR test was positive in dilution 1:8, more than fourfold decrease. The almost complete disappearance of the skin lesions upon antibiotic and antiretroviral therapy was consistent with pseudo lymphoma and the final diagnosis was syphilis and HIV co-infection mimicking CD8+ aggressive epidermotropic CTCL.
In the United States, 28% of males with STIs and 16% of all STIs patients suffer from both HIV and syphilis4 especially men who have sex with man. HIV-positive patients have an eight times higher risk of being co-infected with syphilis and both diseases demonstrate more aggressive course as was observed in the present case. Both syphilis and HIV are reported to mimic cutaneous lymphomas. HIV patients may present with CD8 T-cell pseudolymphoma in immunodeficiency which histopathologically is characterised by lymphocytic epidermotropic infiltrate.4 According to Schartz et al., HIV-specific cytotoxic T-cells are hypothesised to cause the infiltration.5 However, the unusual manifestation of syphilis and HIV co-infection presents with a predominance of CD8-positive lymphocytes and monoclonal TCR rearrangement mimicking aggressive epidermotropic CD8 CTCL.6 Removing the triggering factor remains the mainstream of action, followed by spontaneous resolution of the lesions. Thus, CTCLs caused by infections have a benign prognosis and rapid improvement in clinical presentation after antibiotic and antiviral therapy.7
In conclusion, we report a patient with syphilis and HIV co-infection mimicking aggressive epidermotropic CD8+ CTCL who responded dramatically to antibiotic and antiretroviral therapy, which suggests screening for underlined sexually transmitted infections in all patients with an unusual clinical course of a suspected malignancy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
References
- Syphilis: uncommon presentations in adults. Clin Dermatol. 2005;23:555-64.
- [CrossRef] [PubMed] [Google Scholar]
- Syphilis increases HIV viral load and decreases CD4 cell counts in HIV-infected patients with new syphilis infections. AIDS. 2004;18:2075-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- CD8-positive pseudolymphoma in lues maligna and human immunodeficiency virus with monoclonal T-cell receptor-beta rearrangement. J Cutan Pathol. 2019;46:204-10.
- [CrossRef] [PubMed] [Google Scholar]
- Regression of CD8 pseudolymphoma after HIV antiviral triple therapy. J Am Acad Dermatol. 2003;49:139-41.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous pseudolymphoma: A review on the spectrum and a proposal for a new classification. J Cutan Pathol. 2020;47:76-97.
- [CrossRef] [PubMed] [Google Scholar]






