Translate this page into:
Macular presentation of primary cutaneous follicle center lymphoma with an intermittent clinical course
2 Department of Pathology, Lozano Blesa Clinical Hospital, Zaragoza, Spain
Correspondence Address:
Isabel Abad�as-Granado
C/Mosen Andrés Vicente n° 36, Escalera Izquierda, 1°B 50017 Zaragoza
Spain
| How to cite this article: Abad�as-Granado I, Sánchez-Bernal J, Muñoz-González G, Ara-Martín M. Macular presentation of primary cutaneous follicle center lymphoma with an intermittent clinical course. Indian J Dermatol Venereol Leprol 2019;85:525-527 |
Sir,
Primary cutaneous follicle center lymphoma is defined as the neoplastic proliferation of germinal center cells which are confined to the skin. It is an indolent lymphoma, typically manifesting as solitary or grouped nodules, plaques, and tumors, preferentially located preferentially over the scalp and forehead or on the trunk; however, a clinical variant characterized by macules or inconspicuous lesions on the head has recently been described.[1]
A 52-year-old woman with no relevant medical history developed an extensive, erythematous macular lesion on the scalp. Although her condition was initially diagnosed as seborrheic dermatitis, she did not respond to treatment. Examination revealed a diffuse, ill-defined, erythematous macule, with scarce superficial telangiectasias, coexisting with mild alopecia, over the frontoparietal scalp [Figure - 1]. A skin biopsy was done for suspected lupus erythematosus, angiosarcoma, or lymphoma. Histologic examination confirmed the diagnosis of follicle center cell lymphoma, showing a diffuse lymphoid infiltrate with follicular pattern involving the dermis and subcutaneous fat [Figure - 2]. Neoplastic cells stained positive for CD20 and Bcl-6, whereas staining for Bcl-2 was negative. Lymph node examination, routine laboratory tests, and a computed tomographic scan yielded normal findings. Observing the spontaneous remission of the lesions, it was decided not to perform a bone marrow biopsy or treatment with radiotherapy. The patient has been followed up with a strategy involving watchful waiting and occasional topical steroids. She has been healthy since her diagnosis 4 years ago, other than the intermittent disappearance and reappearance of her scalp lesions [Figure - 3].
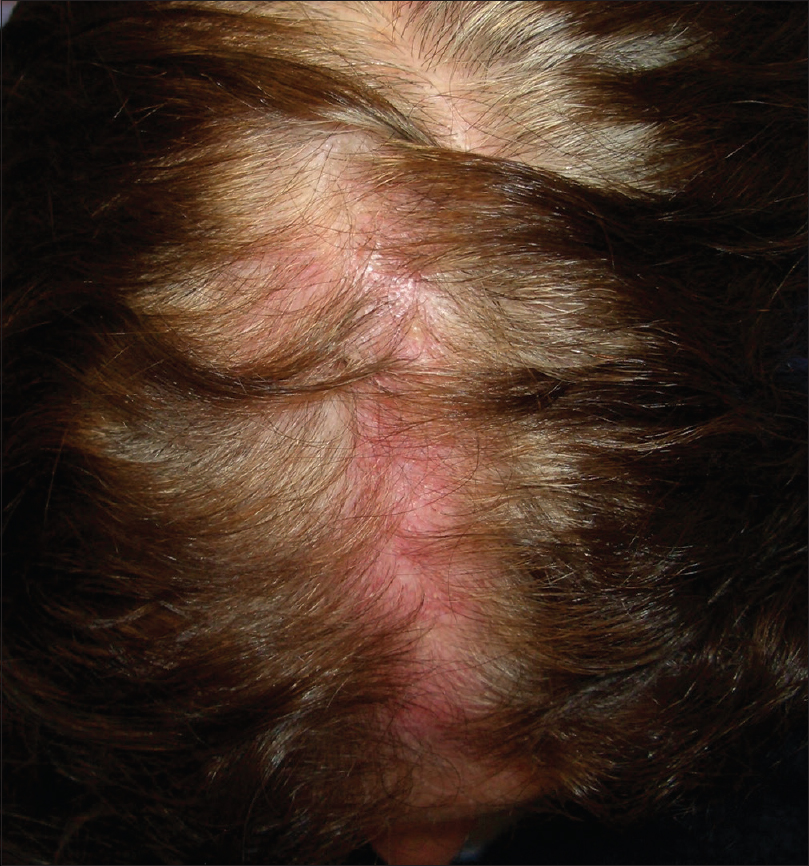 |
| Figure 1: Diffuse, ill-defined, erythematous macule on the frontoparietal scalp |
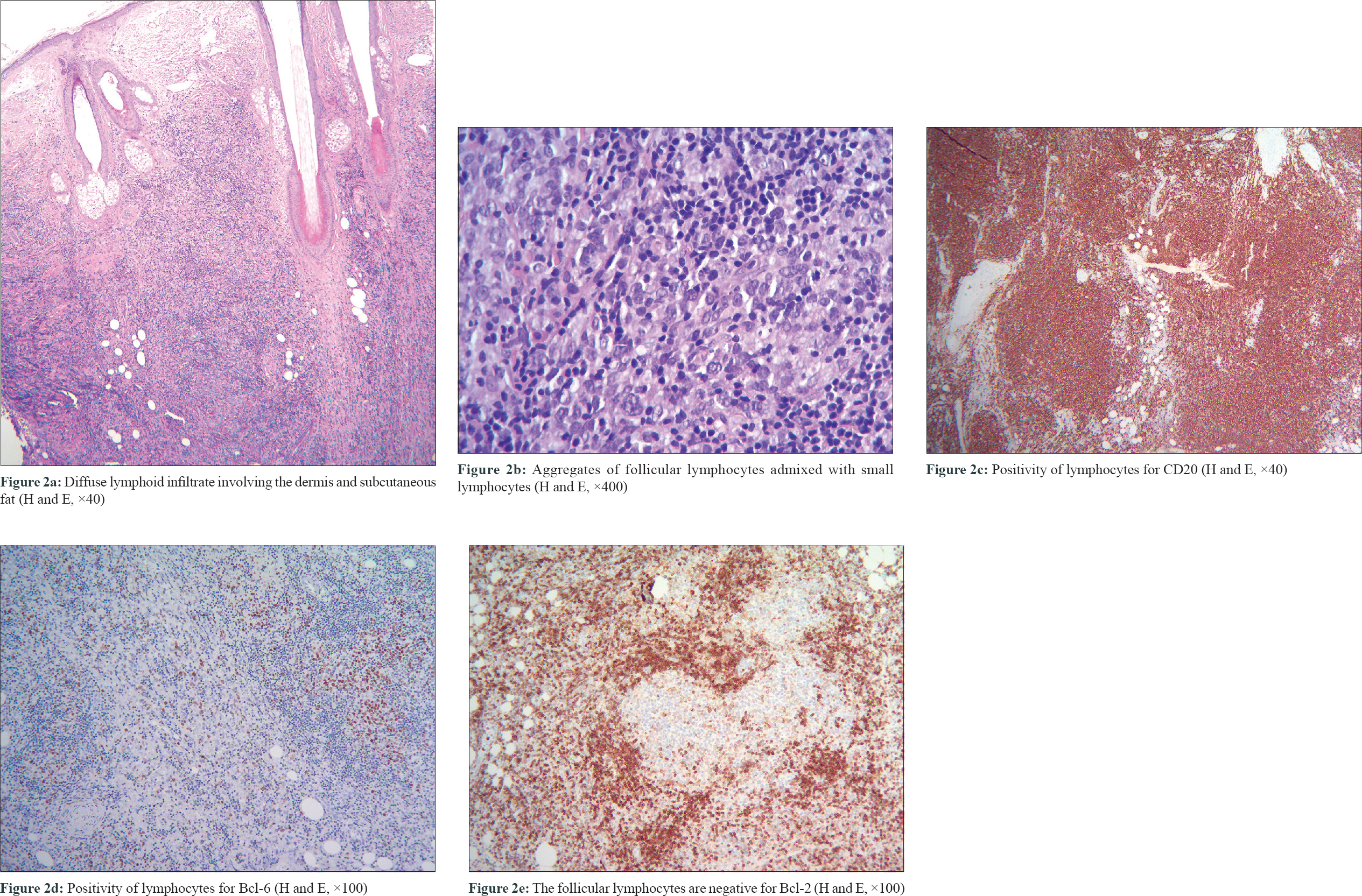 |
| Figure 2 |
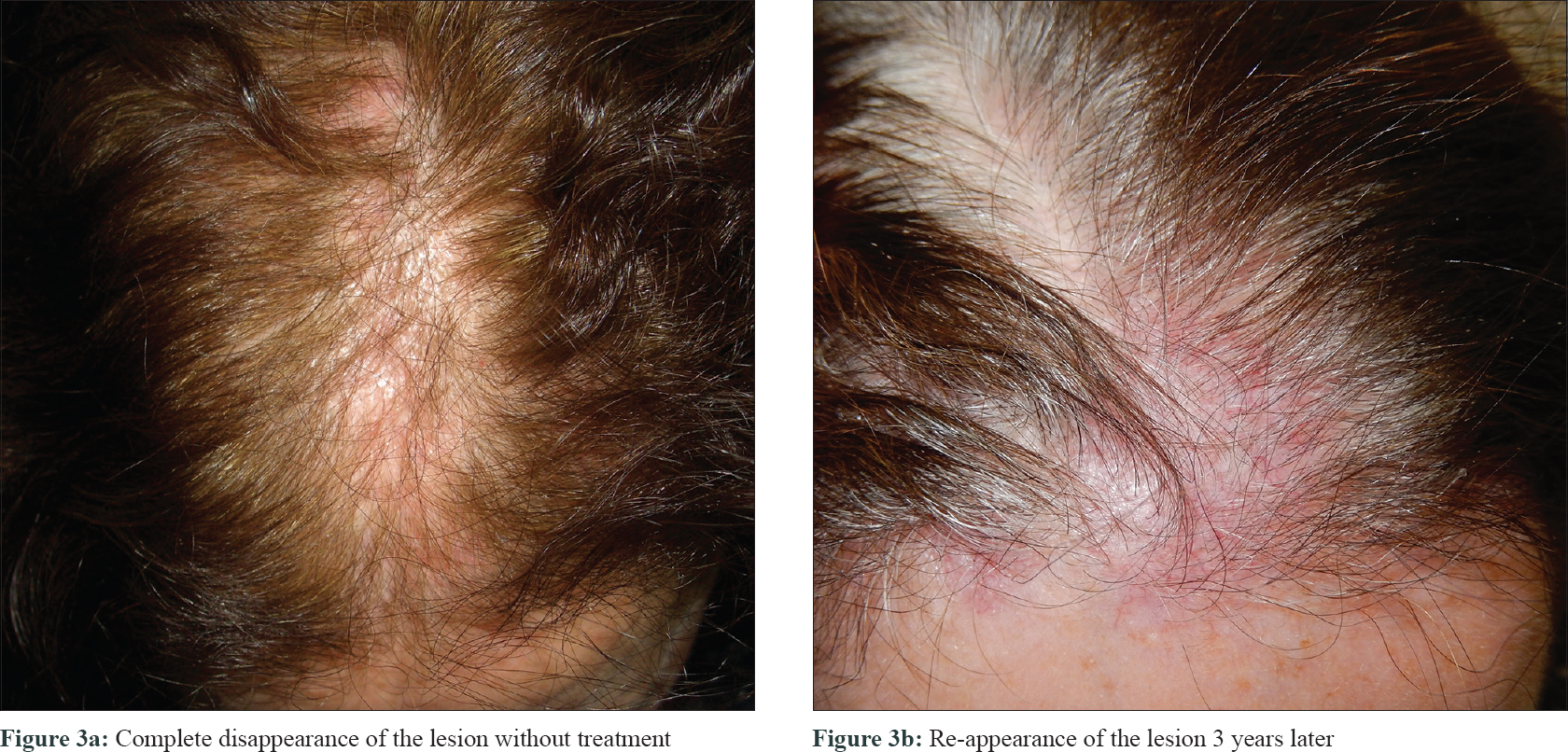 |
| Figure 3 |
Primary cutaneous follicle center lymphoma is the most common subtype of primary cutaneous B-cell lymphoma, representing about 11%–18% of all primary cutaneous lymphomas.[2] It is listed as a specific entity in both the 2005 European Organization for Research and Treatment of Cancer-World Health Organization (WHO) classification of primary cutaneous lymphomas and the 2016 WHO classification of tumors of hematopoietic and lymphoid tissues. It presents clinically with erythematous plaques and tumors, located predominantly over the head and neck, and on the trunk, even though atypical presentations have been described. Massone et al. reported 18 patients presenting with multiple erythematous, miliary, and agminated papules located on the head and neck area,[3] difficult to differentiate from other conditions including rosacea, lupus miliaris disseminatus faciei, and acne.[4] Moreover, Kluk et al. described a case of primary cutaneous follicle center lymphoma which presented with scarring alopecia.[5] Recently, Massone et al. reported a series of 11 patients and 2 with secondary cutaneous follicle center lymphoma presenting with diffuse, ill-defined, partly hypochromic, partly erythematous macules or with inconspicuous lesions located predominantly on the scalp and forehead, very similar to those of our patient.[1] This atypical clinical presentation of follicle center lymphoma poses a major diagnostic challenge. The differential diagnoses are extensive and, include several inflammatory skin conditions such as erysipelas, rosacea, temporal arteritis, macular sarcoidosis, lupus erythematosus, androgenetic or scarring alopecia, Borrelia infection, and neoplastic conditions such as cutaneous metastases or angiosarcoma.[1] In fact, the final diagnosis could be established only upon histopathological examination and immunohistochemistry, which show the same features than more conventional presentations of the disease, allowing a precise diagnosis and classification. Besides posing a diagnostic challenge, the presence of diffuse, ill-defined macules poses another challenge - therapeutic. The extent of the lesions is not clearly visible, and their size makes a surgical or interventional approach, unfeasible. Radiotherapy or rituximab may be valid alternatives and the 'watchful waiting' approach represents a possible management strategy as well.[1] Primary cutaneous follicle center lymphoma is considered indolent and its course is generally benign, with a survival rate of >95% at 5 years. In our case, we highlight the intermittent clinical course, with spontaneous remissions without treatment and recurrence of the lesions on several occasions.
In conclusion, we report a new case of primary cutaneous follicle center lymphoma, showing an atypical clinical presentation characterized by macular lesions, of difficult clinical diagnoses, and an intermittent clinical course. Dermatologists should be aware of this clinical variant of follicle center lymphoma, to establish an early diagnosis and institute appropriate treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Massone C, Fink-Puches R, Cerroni L. Atypical clinical presentation of primary and secondary cutaneous follicle center lymphoma (FCL) on the head characterized by macular lesions. J Am Acad Dermatol 2016;75:1000-6.
[Google Scholar]
|
| 2. |
Bouaziz JD, Bastuji-Garin S, Poszepczynska-Guigné E, Wechsler J, Bagot M. Relative frequency and survival of patients with primary cutaneous lymphomas: Data from a single-centre study of 203 patients. Br J Dermatol 2006;154:1206-7.
[Google Scholar]
|
| 3. |
Massone C, Fink-Puches R, Laimer M, Rütten A, Vale E, Cerroni L, et al. Miliary and agminated-type primary cutaneous follicle center lymphoma: Report of 18 cases. J Am Acad Dermatol 2011;65:749-55.
[Google Scholar]
|
| 4. |
Soon CW, Pincus LB, Ai WZ, McCalmont TH. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol 2011;65:887-9.
[Google Scholar]
|
| 5. |
Kluk J, Charles-Holmes R, Carr RA. Primary cutaneous follicle centre cell lymphoma of the scalp presenting with scarring alopecia. Br J Dermatol 2011;165:205-7.
[Google Scholar]
|
Fulltext Views
4,786
PDF downloads
2,522





