Translate this page into:
Majocchi's granuloma over the face
2 Department of Dermatology, University of Osnabrueck, Osnabrueck, Germany
Correspondence Address:
Min Zheng
Department of Dermatology, Second Affiliated Hospital, Zhejiang University School of Medicine, 88 Jiefang Rd, Hangzhou 310009
China
| How to cite this article: Liu C, Landeck L, Cai SQ, Zheng M. Majocchi's granuloma over the face. Indian J Dermatol Venereol Leprol 2012;78:113-114 |
Sir,
Majocchi′s granuloma (MG) is an atypical and uncommon presentation of dermatophytic infection involving the invasion of dermal and subcutaneous tissue by fungal organisms. [1] It usually begins as a suppurative folliculitis and may culminate in the development of widespread granulomas. MG is a rare disease, and immunosuppressed patients are at increased risk, especially those with T-cell deficiencies. [1] MG may occur in patients receiving immunosuppressive therapy for leukemia or lymphoma, autoimmune diseases or other malignancies and post-organ transplantation. However, MG has also been described after shaving procedures of the legs. Most commonly, Trichophyton rubrum is identified. MG may develop on any hair-bearing area, but, most often, the scalp, the face, forearms, hands, and legs are involved. However, there are only a few reports in the literature of facial involvement. [2],[3],[4] The prognosis of MG can be regarded as good, because there is effective pharmacotherapy available for it. Itraconazole and griseofulvin therapy is effective. [1],[5] Treatment should be continued until all lesions are cleared. Prolonged treatment may be necessary in immunocompromised patients. [5]
We describe a case of MG of the face and the scalp in a 55-year-old female who had been diagnosed with eczema and received systemic (i.m. and oral) as well as topical corticosteroids over a period of 7 months. Dermatologic investigation of the facial skin and scalp presented erythematous papules, plaques and nodules with and without scaling. On the scalp, the skin lesions were accompanied by alopecia [Figure - 1]. On medical examination, there was no regional lymphadenopathy observed. Findings of laboratory tests, including complete blood count, serum glucose, aspartate aminotransferase and alanine aminotransferase level, human immunodeficiency virus (HIV) antibody and T cell subtypes, were within the normal range and did not suggest any systemic disease or immunodeficiency.
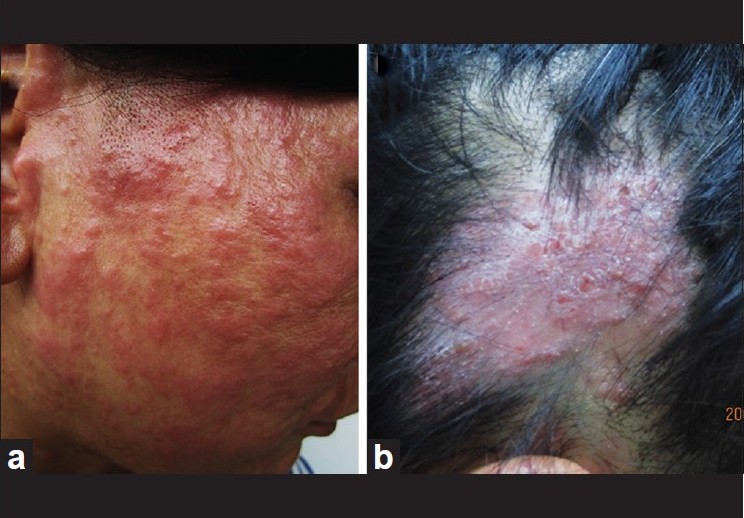 |
| Figure 1: Clinical findings: Erythematous papules, plaques and nodules with and without scaling at the face (a) and the scalp (b) of our patient. Additional lesions of alopecia affecting the scalp |
For histological examination, a punch biopsy was taken from the scalp and cultured on potato dextrose agar. This showed a dermal abscess and, after staining with PAS (Periodic Acid Schiff Stain), spores and hyphae were seen [Figure - 2]. Enzyme-linked immunosorbent assay-polymerase chain reaction of the biopsy identified T. rubrum, which was also grown on culture of the biopsy tissue as characteristic granular white colonies with blood-red reverse. The diagnosis of MG following immunosuppression with corticosteroids was made. It seems likely that the systemic corticosteroid treatment worsened the fungal infection. Other immunodeficiencies were ruled out upon investigation. The origin of the infection was most probably due to the patient′s pet.
The patient was treated with systemic itraconazole (200 mg once daily) and topical terbinafine (twice-daily) for 8 weeks.
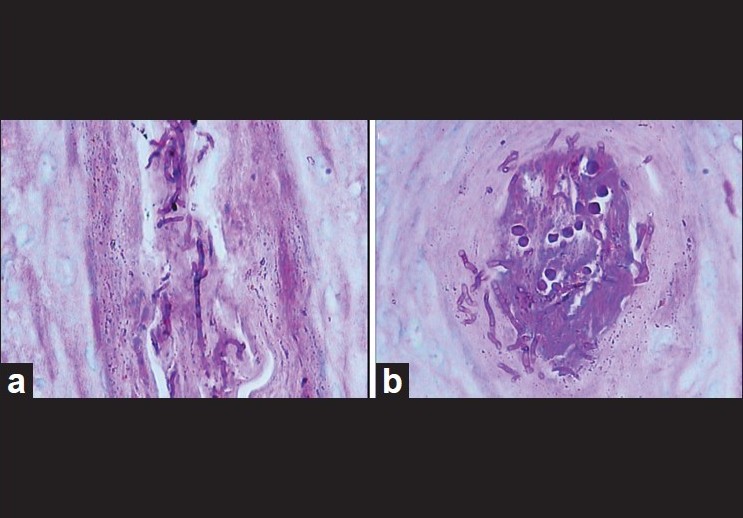 |
| Figure 2: Typical hyphae and spores in ruptured hair follicule in deep dermis by Periodic Acid Schiff stain (a), longitudinal section (×400). (b) Cross-section (×400) |
All lesions resolved without scarring at the end of antifungal therapy; hair re-growth was observed at the former lesions affecting the scalp.
In conclusion, dermatologists should consider the diagnosis of MG even in otherwise healthy individuals, especially when their medical history reveals a corticosteroid treatment for recurrent eczema.
| 1. |
Elgart ML. Tinea incognito: An update on Majocchi granuloma. Dermatol Clin 1996;14:51-5.
[Google Scholar]
|
| 2. |
Gill M, Sachdeva B, Gill PS, Arora B, Deep A, Karan J. Majocchi's granuloma of the face in an immunocompetent patient. J Dermatol 2007;34:702-4.
[Google Scholar]
|
| 3. |
Smith KJ, Neafie RC, Skelton HG 3 rd , Barrett TL, Graham JH, Lupton GP. Majocchi's granuloma. J Cutan Pathol 1991;18:28-35.
[Google Scholar]
|
| 4. |
Chen HH, Chiu HC. Facial Majocchi's granuloma caused by Trichophyton tonsurans in an immunocompetent patient. Acta Derm Venereol 2003;83:65-6.
[Google Scholar]
|
| 5. |
Tan E, Goh CL. Unusual papular lesions in a healthy man. Arch Dermatol 2002;138:117-22.
[Google Scholar]
|
Fulltext Views
5,941
PDF downloads
3,433





