Translate this page into:
Metabolic syndrome and female gender, but not methotrexate, are the important associations of significant liver fibrosis in patients with moderate-to-severe psoriasis as detected by transient elastography
2 Department of Hepatology, PGIMER, Chandigarh, India
3 Department of Immunopathology, PGIMER, Chandigarh, India
Correspondence Address:
Sunil Dogra
Department of Dermatology, Venereology and Leprology, PGIMER, Chandigarh - 160 012
India
| How to cite this article: Mahajan R, Dogra S, Handa S, Razmi T M, Narang T, Rathi S, Dhiman RK, Saikia B, Karim A. Metabolic syndrome and female gender, but not methotrexate, are the important associations of significant liver fibrosis in patients with moderate-to-severe psoriasis as detected by transient elastography. Indian J Dermatol Venereol Leprol 2020;86:649-655 |
Abstract
Background: Many international guidelines on psoriasis management have emphasized upon the need to identify risk factors for liver fibrosis and that the risk may be increased after a certain total cumulative dose of methotrexate.
Methods: Consecutive patients with moderate-to-severe psoriasis were assessed for liver fibrosis using transient elastography and noninvasive scores. Based on the presence of significant liver fibrosis, the Odds ratio associated with various factors was calculated using logistic regression analysis. Receiver operating characteristic curves were calculated to find maximal cutoff values of noninvasive tests to detect fibrosis.
Results: In this cross-sectional study, 134 patients completed the study. Significant fibrosis (liver stiffness measurement ≥7, corresponding to F2 fibrosis or higher) was seen in 33 (24.6%) patients. Neither methotrexate exposure nor total cumulative dose of ≥1.5 was associated with significant fibrosis. Female sex (P = 0.024) and the presence of metabolic syndrome (P = 0.034) were the two variables associated with significant liver fibrosis. On logistic regression analysis, the odds ratio for the female gender and metabolic syndrome was estimated to be 2.51 (95% confidence interval - 1.09–5.81) and 2.33 (95% confidence interval - 1.03–5.27), respectively. Aspartate transaminase to platelet ratio index, nonalcoholic fatty liver disease score and the fibrosis-4 index had low sensitivity in comparison to transient elastography.
Limitations: These included small sample size, small number of patients with a total cumulative methotrexate dose of >3–4.5 g, and lack of control group consisting of healthy persons. Another is the absence of liver biopsies considered as the gold standard in the diagnosis of liver fibrosis.
Conclusions: Metabolic syndrome and female sex are associated with the development of significant liver fibrosis in patients with psoriasis. Methotrexate exposure does not seem to be significantly associated with significant liver fibrosis.
Introduction
Psoriasis has increasingly been associated with metabolic syndrome and its components like obesity and diabetes mellitus.[1] A few studies have shown that the risk of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis are significantly increased in psoriatic population.[2],[3],[4] The prevalence of significant liver fibrosis and cirrhosis in psoriasis has been variably estimated to be 0–33% to 0–26%, respectively.[5] In a case-control study by Laharie et al., significant liver fibrosis was seen in 12/111 (10.8%) patients with psoriasis, Crohn's disease and rheumatoid arthritis.[6]
In the past, the development of liver fibrosis has been attributed to methotrexate use and believed to correlate with the total cumulative dose of the drug.[7],[8] However, methotrexate is used in several other chronic inflammatory diseases and there has been conflicting evidence regarding the role of its cumulative dose leading to advanced liver fibrosis. In one of the larger studies with sequential liver biopsies, Rosenberg et al. suggested that the presence of other risk factors such as diabetes mellitus significantly increases the risk of liver fibrosis in methotrexate treated patients even at lower doses, though the study did not comment on the risk in patients never exposed to methotrexate.[9] The present study was done to estimate the prevalence of significant liver fibrosis (F2 and above) as assessed by transient elastography and to calculate the association of various factors with the development of liver fibrosis, especially methotrexate. In addition, we tried to establish the correlation of the results of transient elastography with other noninvasive tests in patients with psoriasis.
Methods
Study design
Cross-sectional study.
Study setting
Psoriasis clinic at Postgraduate Institute of Medical Education and Research, Chandigarh, India from January 2016 to December 2018. The study was initiated after taking approval from the institutional ethics committee (NK/978/Res/351).
Sample size
Assuming the prevalence of liver fibrosis in psoriasis patients to be 10.8% and the precision to be 5%, the power of the study was calculated as 80% with 95% confidence interval and the sample size was calculated as 149 (based on the formula n = Z[2] P (1-P)/d[2]; n = sample size, Z = Z statistic for a level of confidence, P = expected prevalence, d = precision).[9]
Case definitions
Methotrexate exposure
A patient of moderate-to-severe psoriasis (with body surface area involvement >10% or psoriasis area and severity index >10) aged >18 years who was on methotrexate was considered methotrexate-exposed. He/she may or may not have received methotrexate in the past. In case the patient had never received methotrexate in the past and was currently on systemic therapy other than methotrexate, he/she was considered methotrexate naïve.
Liver fibrosis
The extent of liver fibrosis was evaluated using vibration controlled transient elastography (FibroScan™, Echosens, France). It was defined based on the values of liver stiffness measurement: Stage 1 liver fibrosis – liver stiffness measurement ≥6.1 kPa, Stage 2 liver fibrosis – ≥7.0 kPa, Stage 3 liver fibrosis – ≥9.0 kPa, Stage 4 liver fibrosis – ≥11.8 kPa. Stage 2–4 liver fibrosis was also defined as significant liver fibrosis.[10]
Liver stiffness measurement cutoff for significant liver fibrosis (F2 or higher) was taken as 7.0 kPa, and that for advanced fibrosis (F3 or higher) was 9.0 kPa. As data on the noninvasive assessment of methotrexate-induced liver injury is sparse, we used the cutoffs derived from a model of nonalcoholic fatty liver disease used in previous studies in a similar population to evaluate fibrosis.[10]
Patient assessment
Consecutive patients of psoriasis attending the psoriasis clinic were screened for inclusion into the study. An informed consent was taken. Detailed history regarding the duration and extent of the disease, family history, past treatment and aggravating/initiating factors was recorded. In addition to assessment of body surface area and psoriasis area and severity index, following details regarding the presence of other risk factors for liver fibrosis were noted - overweight/obesity defined as body mass index ≥25 and ≥30, respectively, diabetes mellitus, significant alcohol intake defined as alcohol intake >14 drinks/week,[6] patients' exposure to methotrexate and presence of metabolic syndrome as per the International Diabetes Federation criteria.[11] Methotrexate and other systemic therapies were initiated as per standard guidelines.[7] Patients who tested positive either for hepatitis B or hepatitis C or HIV infection were excluded from the study.
Assessing liver fibrosis
Only patients with 10 validated measurements and interquartile range <30% of median liver stiffness on FibroScan were included. In addition, based on history and serum biochemistry, we estimated other noninvasive markers of liver fibrosis - aspartate transaminase to platelet ratio index, nonalcoholic fatty liver disease and fibrosis-4 index. Liver biopsy was offered to those patients who showed significant liver fibrosis on FibroScan. All subjects were treated appropriately for their disease severity.
- The aspartate transaminase to platelet ratio index was calculated as (aspartate aminotransferase elevation/platelet count) ×100 where the aspartate aminotransferase elevation is the aspartate aminotransferase/upper limit of normal for aspartate aminotransferase, and the platelet count is expressed as platelets/mm[3] ÷ 1000. An aspartate transaminase to platelet ratio index I threshold of 1.0 had an estimated sensitivity and specificity of 76 and 72% for cirrhosis[12]
- Nonalcoholic fatty liver disease score combines age, hyperglycemia, body mass index, platelet count, albumin and aspartate aminotransferase/alanine aminotransferase ratio as independent indicators of advanced liver fibrosis. By applying a high cutoff score (0.676), the presence of advanced fibrosis could be diagnosed with high accuracy (positive predictive value of 90% and 82% in the estimation and validation groups, respectively)[13]
- The fibrosis-4 index combines standard biochemical values (platelets, aspartate aminotransferase, alanine aminotransferase) and age. A fibrosis-4 index <1.45 had a negative predictive value of 94.7% to exclude severe fibrosis with a sensitivity of 74.3%. A fibrosis-4 index higher than 3.25 had a positive predictive value to confirm the existence of significant fibrosis (F3–F4) of 82.1% with a specificity of 98.2%.[14]
Statistical analysis
Normality of quantitative data was checked by measures of Kolmogorov-Smirnov test. Comparison of means was done by student t-test for normally distributed or Mann-Whitney U-test for skewed distribution. To analyze the efficacy of the noninvasive tests – aspartate transaminase to platelet ratio index, nonalcoholic fatty liver disease score and fibrosis-4 index, sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy were calculated keeping transient elastography as the gold standard. We combined the two most significant parameters into possible derivation to increase the sensitivity and specificity to separate cases with liver fibrosis from age-matched normal controls. Receiver operating characteristic curves was calculated to find maximal cutoff values of aspartate transaminase to platelet ratio index, nonalcoholic fatty liver disease and fibrosis-4 index and combined variables to detect fibrosis.
To find independent associations for significant liver fibrosis, logistic regression analysis was carried out. The clinical factors which came out to be significant in bivariate analysis were put to bivariate logistic regression analysis. After controlling the factors which came out to be nonsignificant in bivariate logistic regression analysis, multinomial logistic regression analysis was carried and adjusted odds ratios were calculated. All the statistical tests were two-sided and performed at a significance level of α = 0.05. The analysis was conducted using IBM Statistical Package for Social Sciences statistics (version 22.0).
Results
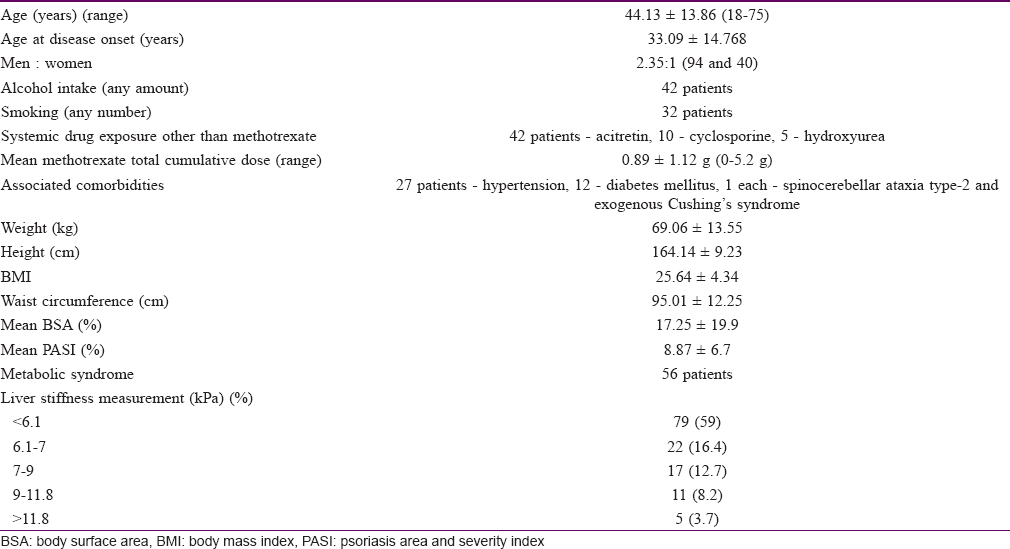
In this cross-sectional study, 134 patients participated and were analyzed at the end of the study period [Figure - 1] and [Table - 1]. Of 134 patients, significant liver fibrosis (F2 or higher, liver stiffness measurement ≥7) was seen in 33 (24.6%) patients. Of these 33 patients, liver stiffness corresponding to F2 fibrosis was seen in 17 (12.7%), F3 in 11 (8.2%) and F4 in 5 (3.7%) patients. To assess the effect of exposure to methotrexate, we compared the frequencies of development of significant liver fibrosis among the methotrexate exposed (at any total cumulative dose) and nonexposed which was found to be nonsignificant (26/104 i.e.; 25% among methotrexate exposed compared to 7/30 i.e.; 23% among methotrexate naive; P = 1.0). We also tried to find out any effect of methotrexate exposure at a pre-specified total cumulative dose cutoff of 1.5 g. However, we did not find any significant association of the total cumulative dose of methotrexate (at the prespecified cutoff of 1.5 g) and development of significant liver fibrosis (19/80 i.e.; 23.7% among those with a total cumulative dose of methotrexate <1.5 g compared to 7/24 i.e.; 29.1% among those with a total cumulative dose of methotrexate >1.5 g; P = 0.59). Other potentially hepatotoxic drugs (such as acitretin, cyclosporine, hydroxyurea, etc), were not found to have a significant association with liver fibrosis.
 |
| Figure 1: Recruitment flow of study participants in this study |
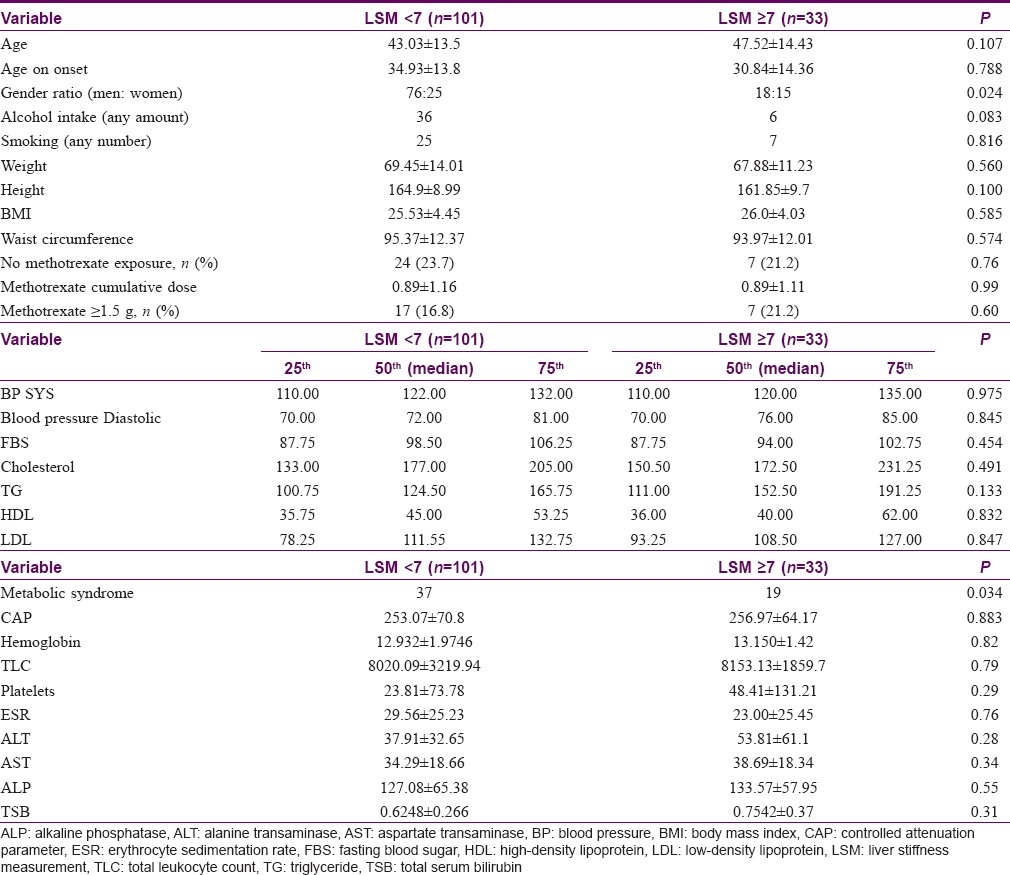
In addition, we compared the differences between the variables between the two groups; one who had developed significant liver fibrosis compared to those who did not, as summarized in [Table - 2]. Among the several variables, female gender (P = 0.024) and the presence of metabolic syndrome (P = 0.034) were significantly higher in the group who developed significant liver fibrosis. To assess the strength of their association, we used the logistic regression analysis which confirmed the association of female gender (odds ratio-2.51; 95% confidence interval - 1.09–5.81) and metabolic syndrome (odds ratio - 2.33; 95% confidence interval - 1.03–5.27) with significant liver fibrosis.
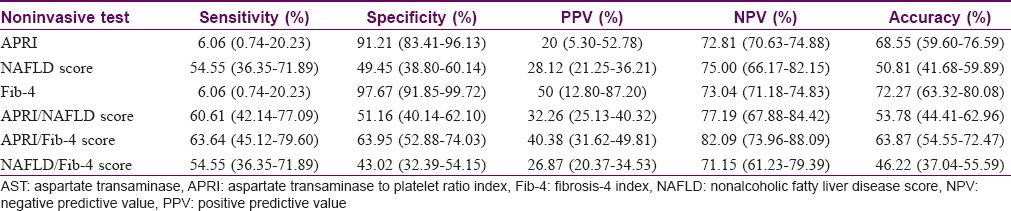
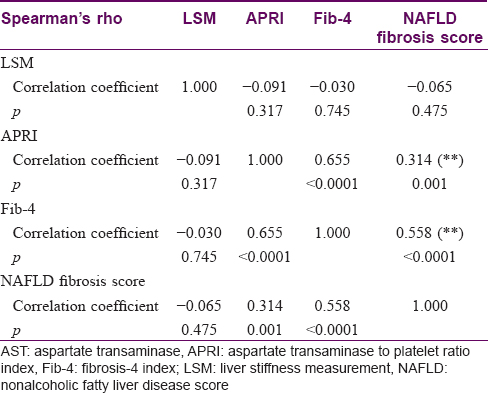
As a secondary outcome, we calculated the area under the receiver operating curve of the various noninvasive tests. [Table - 3] shows the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of these noninvasive tests when used alone or in combination. When used alone, aspartate transaminase to platelet ratio index enabled the identification of patients with significant liver fibrosis with an area under the receiver operating characteristic curve of 0.61 (95% confidence interval 0.50–0.73). These values for nonalcoholic fatty liver disease and fibrosis-4 index were 0.52 (95% confidence interval 0.40–0.64) and 0.52 (95% confidence interval 0.39–0.63), respectively. Using logistic regression model, we tried to combine the area under the receiver operating characteristic curve of aspartate transaminase to platelet ratio index/nonalcoholic fatty liver disease score, aspartate transaminase to platelet ratio index/fibrosis-4 score and nonalcoholic fatty liver disease/fibrosis-4 score. Area under the receiver operating characteristic curve for combined nonalcoholic fatty liver disease score/aspartate transaminase to platelet ratio index, combined nonalcoholic fatty liver disease score/fibrosis-4 index and combined fibrosis-4/aspartate transaminase to platelet ratio index were 0.61 (95% confidence interval 0.50–0.72), 0.53 (95% confidence interval 0.41–0.65) and 0.63 (95% confidence interval 0.52–0.74), respectively. We also measured the correlation among the results of FibroScan and other noninvasive tests for the detection of liver fibrosis. It was observed that the liver stiffness measurement values did not correlate significantly with aspartate transaminase to platelet ratio index, fibrosis-4 and nonalcoholic fatty liver disease fibrosis score [Table - 4].
Discussion
Methotrexate has remained the gold standard in the treatment of psoriasis, although concerns over methotrexate-induced hepatotoxicity and the consequent development of significant liver fibrosis have always been held against its continued long-term use in psoriasis.[7] The most recent American Academy of Dermatology guidelines recommend that in patients without a known risk factor of liver disease, a liver biopsy should be done after 3.5 g of methotrexate with a lower thresh-hold in presence of other risk factors.[8] The point prevalence of significant liver fibrosis in our cohort was 26.3% which is quite high. The Rotterdam study observed severe fibrosis in 8.1% of 74 psoriasis patients not on systemic therapy using a cutoff transient elastography of >9.5 kPa, in comparison to 3.6% of 1461 non-psoriatic controls.[15] This reinforces the concept that treating dermatologists need to actively look for hepatic comorbidities in a patient with psoriasis.
Among the various risk factors assessed, female gender and metabolic syndrome were significantly associated with significant liver fibrosis with an odds ratio of 2.51 and 2.33, respectively. The frequency of metabolic syndrome in the present cohort (56/143 or 41.7%) was similar to that reported in previous literature. An important consideration here is that chronic viral infection was already ruled out (based on the selection criteria), and the population under study had a minimal alcohol intake. While we observed a high prevalence of significant liver fibrosis in our cohort of psoriasis patients, we did not find methotrexate exposure (any exposure or at a predefined cutoff of 1.5 g) to be a significant determinant of significant liver fibrosis. Another interesting observation was the lack of use of biologics in any of the patients in the present cohort. India being a developing country still has certain limitations like limited coverage of medical insurance so that only few patients can afford costly medications like biologics; which in turn emphasizes the need to establish the long-term safety of cheaper alternatives like methotrexate. While it is also important to look for the role of other anti-psoriatic drugs some of which have been associated with hepatoxicity as an adverse effect, but have not been conclusively linked with significant liver fibrosis.
Our observations are also consistent with some of the previously published literature. Cheng and Rademaker refer to a meta-analysis of 636 patients on methotrexate from 15 studies which did not show a correlation between cirrhosis and cumulative dose but it showed an increased risk of hepatic fibrosis in patients who drank ≥100 g alcohol/week (17.8% vs 4.5%) and who had psoriasis versus rheumatoid arthritis (7.7% vs 2.7%).[16] Although the daily alcohol consumption was low among the study population, it cannot be denied that it remains a very important factor towards development of significant liver fibrosis. However, another meta-analysis showed that methotrexate was associated with a small but increased risk (pooled risk difference of 0.22; 95% confidence interval: 0.04–0.41) of liver fibrosis compared with psoriasis patients not treated with methotrexate.[17] In other inflammatory diseases like Crohn's disease, total cumulative dose of methotrexate has not shown to have a direct bearing on liver fibrosis.[18],[19] In another study on noninvasive assessment of liver fibrosis in 518 patients (Crohn's disease, 124; rheumatoid arthritis, 149; psoriasis, 111), of which 390 were being treated with methotrexate, factors associated with liver fibrosis were the body mass index >28 kg/m[2] and high alcohol consumption but not the duration of methotrexate nor its cumulative dose.[6]
Obesity and metabolic syndrome have become the leading causes of liver enzyme derangement due to associated nonalcoholic fatty liver disease.[20] The prevalence and severity of nonalcoholic fatty liver disease are higher in men than in women during the reproductive age, an association which is reversed after menopause.[21],[22] The higher frequency of significant liver fibrosis among women in the present study needs to be further explored despite the observation that both alcohol intake and smoking were significantly more among men compared to women.
The secondary objective of the study was to assess the performance of relatively cheaper biochemical tests/algorithms to detect significant liver fibrosis in psoriasis patients taking into consideration transient elastography as the gold standard. This is important as the highly sensitive, specific and validated algorithms FibroTest and enhanced liver fibrosis tests are costly and difficult to administer on a large scale in resource-poor settings. A systematic review and meta-analysis observed the sensitivity of FibroScan to be 50% and 88%, respectively.[23] In their retrospective analysis, Rongngern et al. found that the area under the receiver operating characteristic curve (0.78) indicated that transient elastography was capable of identifying patients with and without liver injury and that total cumulative dosage of methotrexate, age, gender, metabolic syndrome and metabolic components were not significantly associated with transient elastography values≥7.1 kPa and Roenigk grade≥3a.[24] Lynch et al. studied 77 psoriasis patients and observed that body mass index (r=0.40, P=.005) and age (r=0.52, P=.005) correlated with abnormal transient elastography results.[25] Similar to the observations regarding correlation between liver stiffness measurement and other tests, they did not find any correlation between procollagen II N-Terminal propeptide (PIIINP) levels and transient elastography results or between procollagen II N-Terminal propeptide levels and FibroTest results.
We did not find the performance of aspartate transaminase to platelet ratio index, fibrosis-4 and nonalcoholic fatty liver disease score fibrosis score to be satisfactory when used alone or in conjunction with each other with low sensitivity. In general, noninvasive markers of liver fibrosis such as elastographic procedures (FibroScan, shear wave elastography) and serum biomarker-based tests (FibroTest, enhanced liver fibrosis test) are powerful tools to rule in and rule out cirrhosis. They do not seem to accurately characterize intermediate stages of liver fibrosis over one-third of our study population having levels of liver stiffness between 6.1 and 11.8 kPa, corresponding to F1-F4 fibrosis. Nevertheless, it seems that these techniques can reliably estimate the presence of significant fibrosis.
Limitations of the present study include the lack of liver biopsies often considered as the gold standard in the diagnosis of liver fibrosis. Although it was offered to patients with significant liver fibrosis, all of them refused it considering its invasive nature and potential complications. Inclusion of healthy controls could have allowed us to comment on the role of psoriasis as an independent risk factor for liver fibrosis. In addition, the effect of the other hepatotoxic drugs and of the duration of methotrexate exposure (recent or prolonged) could not be estimated. Another was a fewer number of patients with a very high total cumulative dosage of methotrexate. In fact, in the present study, less than 10 patients had a total cumulative dosage of more than 3.5 g and they had normal liver stiffness measurement values. Till a decade back, American Academy of Dermatology guidelines suggested 1.5 g as the cutoff for advising liver biopsy hence, it was very unlikely that many dermatologists would continue methotrexate beyond this cutoff. Instead, most would choose to rotate to some other therapy. Therefore, we were unlikely to get many patients with >3–4.5 g of methotrexate.
Conclusion
The observations in the study suggest that metabolic syndrome and female gender are important associations of significant liver fibrosis. The results highlight the need to further study the role played by methotrexate in causing significant liver fibrosis in psoriasis patients since it continues to be widely prescribed either as monotherapy or in combination with biologics.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Prey S, Paul C, Bronsard V, Puzenat E, Gourraud PA, Aractingi S, et al. Cardiovascular risk factors in patients with plaque psoriasis: A systematic review of epidemiological studies. J Eur Acad Dermatol Venereol 2010;24 Suppl 2:23-30.
[Google Scholar]
|
| 2. |
Wenk KS, Arrington KC, Ehrlich A. Psoriasis and non-alcoholic fatty liver disease. J Eur Acad Dermatol Venereol 2011;25:383-91.
[Google Scholar]
|
| 3. |
Gisondi P, Targher G, Zoppini G, Girolomoni G. Non-alcoholic fatty liver disease in patients with chronic plaque psoriasis. J Hepatol 2009;51:758-64.
[Google Scholar]
|
| 4. |
Miele L, Vallone S, Cefalo C, La Torre G, Di Stasi C, Vecchio FM, et al. Prevalence, characteristics and severity of non-alcoholic fatty liver disease in patients with chronic plaque psoriasis. J Hepatol 2009;51:778-86.
[Google Scholar]
|
| 5. |
Laharie D, Terrebonne E, Vergniol J, Chanteloup E, Chabrun E, Couzigou P, et al. The liver and methotrexate. Gastroenterol Clin Biol 2008;32:134-42.
[Google Scholar]
|
| 6. |
Laharie D, Seneschal J, Schaeverbeke T, Doutre MS, Longy-Boursier M, Pellegrin JL, et al. Assessment of liver fibrosis with transient elastography and FibroTest in patients treated with methotrexate for chronic inflammatory diseases: A case-control study. J Hepatol 2010;53:1035-40.
[Google Scholar]
|
| 7. |
Kalb RE, Strober B, Weinstein G, Lebwohl M. Methotrexate and psoriasis: 2009 National Psoriasis Foundation consensus conference. J Am Acad Dermatol 2009;60:824-37.
[Google Scholar]
|
| 8. |
Pathirana D, Ormerod AD, Saiag P, Smith C, Spuls PI, Nast A, et al. European S3-guidelines on the systemic treatment of psoriasis vulgaris. J Eur Acad Dermatol Venereol 2009;23 Suppl 2:1-70.
[Google Scholar]
|
| 9. |
Rosenberg P, Urwitz H, Johannesson A, Ros AM, Lindholm J, Kinnman N, et al. Psoriasis patients with diabetes type 2 are at high risk of developing liver fibrosis during methotrexate treatment. J Hepatol 2007;46:1111-8.
[Google Scholar]
|
| 10. |
Kumar R, Rastogi A, Sharma MK, Bhatia V, Tyagi P, Sharma P, et al. Liver stiffness measurements in patients with different stages of nonalcoholic fatty liver disease: Diagnostic performance and clinicopathological correlation. Dig Dis Sci 2013;58:265-74.
[Google Scholar]
|
| 11. |
Alberti KG, Zimmet P, Shaw J; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome – A new worldwide definition. Lancet 2005;366:1059-62.
[Google Scholar]
|
| 12. |
Papastergiou V, Tsochatzis E, Burroughs AK. Non-invasive assessment of liver fibrosis. Ann Gastroenterol 2012;25:218-31.
[Google Scholar]
|
| 13. |
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, et al. The NAFLD fibrosis score: A noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 2007;45:846-54.
[Google Scholar]
|
| 14. |
Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: An inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology 2007;46:32-6.
[Google Scholar]
|
| 15. |
van der Voort EA, Koehler EM, Nijsten T, Stricker BH, Hofman A, Janssen HL, et al. Increased prevalence of advanced liver fibrosis in patients with psoriasis: A cross-sectional analysis from the Rotterdam study. Acta Derm Venereol 2016;96:213-7.
[Google Scholar]
|
| 16. |
Cheng HS, Rademaker M. Monitoring methotrexate-induced liver fibrosis in patients with psoriasis: Utility of transient elastography. Psoriasis (Auckl) 2018;8:21-9.
[Google Scholar]
|
| 17. |
Maybury CM, Jabbar-Lopez ZK, Wong T, Dhillon AP, Barker JN, Smith CH. Methotrexate and liver fibrosis in people with psoriasis: A systematic review of observational studies. Br J Dermatol 2014;171:17-29.
[Google Scholar]
|
| 18. |
Laharie D, Zerbib F, Adhoute X, Boué-Lahorgue X, Foucher J, Castéra L, et al. Diagnosis of liver fibrosis by transient elastography (Fibroscan) and non-invasive methods in Crohn's disease patients treated with methotrexate. Aliment Pharmacol Ther 2006;23:1621-8.
[Google Scholar]
|
| 19. |
Barbero-Villares A, Mendoza Jiménez-Ridruejo J, Taxonera C, López-Sanromán A, Pajares R, Bermejo F, et al. Evaluation of liver fibrosis by transient elastography (Fibroscan®) in patients with inflammatory bowel disease treated with methotrexate: A multicentric trial. Scand J Gastroenterol 2012;47:575-9.
[Google Scholar]
|
| 20. |
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84.
[Google Scholar]
|
| 21. |
Lonardo A, Nascimbeni F, Ballestri S, Fairweather D, Win S, Than TA, et al. Sex differences in nonalcoholic fatty liver disease: State of the art and identification of research gaps. Hepatology 2019;70:1457-69.
[Google Scholar]
|
| 22. |
Lee K, Sung JA, Kim JS, Park TJ. The roles of obesity and gender on the relationship between metabolic risk factors and non-alcoholic fatty liver disease in Koreans. Diabetes Metab Res Rev 2009;25:150-5.
[Google Scholar]
|
| 23. |
Montaudié H, Sbidian E, Paul C, Maza A, Gallini A, Aractingi S, et al. Methotrexate in psoriasis: A systematic review of treatment modalities, incidence, risk factors and monitoring of liver toxicity. J Eur Acad Dermatol Venereol 2011;25 Suppl 2:12-8.
[Google Scholar]
|
| 24. |
Rongngern P, Chularojanamontri L, Wongpraparut C, Silpa-Archa N, Chotiyaputta W, Pongpaibul A, et al. Diagnostic performance of transient elastography for detection of methotrexate-induced liver injury using Roenigk classification in Asian patients with psoriasis: A retrospective study. Arch Dermatol Res 2017;309:403-8.
[Google Scholar]
|
| 25. |
Lynch M, Higgins E, McCormick PA, Kirby B, Nolan N, Rogers S, et al. The use of transient elastography and FibroTest for monitoring hepatotoxicity in patients receiving methotrexate for psoriasis. JAMA Dermatol 2014;150:856-62.
[Google Scholar]
|
Fulltext Views
5,044
PDF downloads
2,646





