Translate this page into:
Metachronous multiple primary malignant neoplasms in a patient with dermatomyositis
Correspondence Address:
Hong Fang
Department of Dermatology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Qingchun Road, Hangzhou, Zhejiang Province
China
| How to cite this article: Cai Y, Qiao J, Fang H. Metachronous multiple primary malignant neoplasms in a patient with dermatomyositis. Indian J Dermatol Venereol Leprol 2012;78:665 |
Sir,
The association between malignancy and dermatomyositis (DM) has been well-described. The tumors more frequently associated with DM are ovarian, breast, uterine, lung, digestive, and nasopharyngeal. [1],[2] The occurrence of multiple malignancies in an individual associated with DM was rarely reported. [3] Here, we report a Chinese woman with DM had metachronously suffered from invasive lobular carcinoma of the right breast, invasive ductal carcinoma of the left breast, and poorly differentiated endometrioid adenocarcinoma of both ovaries and left fallopian tube.
A 52-year-old Chinese woman presented with a 5-week history of pruritic, violaceous erythema over the face, prothorax, upper back, and upper limb. She also complained difficulty in raising her hands over the level of her shoulders. Her medical history was a right mastectomy for invasive lobular carcinoma followed by 5 cycles of chemotherapy 13 years ago, and a left mastectomy for invasive ductal carcinoma followed by 6 cycles of chemotherapy 3 years ago. Physical examination revealed a periorbital erythema with edematous and violaceous appearance. Edematous erythema and telangiectasias were noted on the face and on the "V" of the neck. Poikiloderma was found over the nape, the shoulders, the extensor surfaces of the arms, and the upper back. Scaly papules involved the extensor aspects of the wrist, interphalangeal, and metacarpophalangeal joints of the hands. Periungual erythema, cuticular overgrowth, and nailfold telangiectasia were revealed on the fingers of bilateral hands [Figure - 1]. Muscle tenderness was detected in the proximal extremities. Power in the upper limbs was 4/5 motor strength. Cardio-respiratory and abdominal examination was unremarkable. Laboratory tests showed elevated muscle enzymes with creatine phosphokinase of 206 U/L (NR 26 ~ 140), lactate dehydrogenase of 272 U/L (NR 135 ~ 225), and hydroxybutyrate dehydrogenase of 190 U/L (NR 72 ~ 182). Serum CA-125 level was 88.6 U/ml (NR 0 ~ 35). Anti-nuclear antibody was positive at a lower titer of 1:40, RNP antibody was positive. The full blood cell count, liver function, renal function, electrolytes, and coagulation studies were within normal ranges. Electromyography features supported the impression of inflammatory myositis. According to Bohan and Peter′s definition, 5 major criteria were used for the diagnosis of PM and DM, the diagnosis of DM was established. Gynecological ultrasonography showed a mass with septation in the left iliac space, which was 5.2 cm × 4.5 cm × 3.8 cm in size. A carcinoma of ovary was highly suspected. Then, the patient underwent total abdominal hysterectomy, bilateral salpingo-oophorectomy, infra-colic omentectomy, pelvic and para-aortic lymphadenectomy. Histopathology and immunohistochemistry examination of the resected specimens confirmed the diagnosis of a poorly differentiated endometrioid adenocarcinoma involving the both ovaries and left fallopian tube [Figure - 2]. The patient had received treatment with intravenous methylprednisolone 40 mg/day after the diagnosis of DM. After treating for 2 weeks, intravenous methylprednisonlone was switched to oral prednisone and tapered to 10 mg daily for maintenance. No recurrence was observed during follow-up.
 |
| Figure 1: Violaceous erythema on (a) the face and (b) the "V" area of the neck, (c) poikiloderma over the shoulders, gottron's papules on (d, e) the knuckles and (f) the wrist, (g) periungual telangiectasia and cuticular overgrowth |
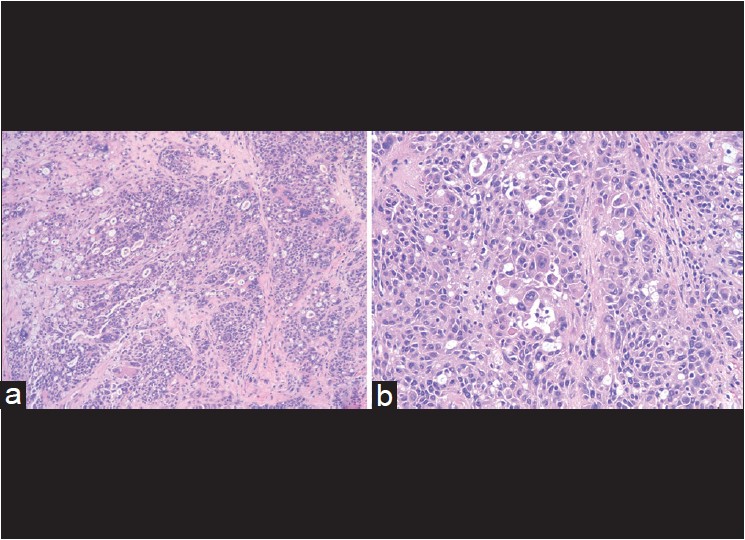 |
| Figure 2: Histopathology of endometrioid adenocarcinoma (H and E, a ×100 b ×400). The tumor cells presented as adenoid or solid nests, with significant atypia and invasive growth. Mucous was deposited in the cytoplasm of some tumor cells |
The association of breast cancer and ovarian carcinoma with DM is well-documented while individuals with the 2 malignancies associated with DM are rare. [4] To the best of our knowledge, DM patient with multiple primary malignant neoplasms, i.e. metachronous carcinoma of both breasts and carcinoma of both ovaries and left fallopian tube, has not been described previously. Warren and Gates [5] established a set of criteria to diagnose multiple primary malignant neoplasms (MPMNs): Each of the tumors must present a definite picture of malignancy; each is distinct; the probability of one being a metastasis of the other must be excluded. The synchronous tumors are defined as two or more primary tumors that are diagnosed within 6 months of the first primary tumor, whereas the metachronous cancers are those that are detected after an interval of more than 6 months. Our case is a patient with DM associated with 3 primary tumors at an interval of 13 years. All tumors were determined by biopsy to be malignant and independent of each other, which were diagnosed as metachronous MPMNs according to Warren′s criteria.
There are no definitive criteria to establish the diagnosis of cancer-associated dermatomyositis. It is most commonly confirmed by studies that cancer-associated dermatomyositis is a paraneoplastic phenomenon. The limit of 3 years that malignancy occurs around the diagnosis of dermatomyositis was established by consensus. In our patient, she had 3 cancers; we speculate that dermatomyositis developed as a paraneoplastic manifestation secondary to endometrioid adenocarcinoma of ovaries and fallopian tube. The metachronous bilateral primary breast cancer supports that the patient is a genetically predisposed individual to developed malignancy.
| 1. |
Levine SM. Cancer and myositis: New insights into an old association. Curr Opin Rheumatol 2006;18:620-4.
[Google Scholar]
|
| 2. |
Chen YJ, Wu CY, Huang YL, Wang CB, Shen JL, Chang YT. Cancer risks of dermatomyositis and polymyositis: A nationwide cohort study in Taiwan. Arthritis Res Ther 2010;12:R70.
[Google Scholar]
|
| 3. |
Voravud N, Dimopoulos M, Hortobagyi G, Ross M, Theriault R. Breast cancer and second primary ovarian cancer in dermatomyositis. Gynecol Oncol 1991;43:286-90.
[Google Scholar]
|
| 4. |
Hashimoto M, Yoshifuji H, Mimori T. A case of dermatomyositis associated with different types of cancers at intervals of six years. Nihon Rinsho Meneki Gakkai Kaishi 2004;27:427-30.
[Google Scholar]
|
| 5. |
Warren S, Gates O. Multiple primary malignant tumors: A survey of the literature and a statistical study. Am J Cancer 1932;16:1358-414.
[Google Scholar]
|
Fulltext Views
1,412
PDF downloads
2,073





