Translate this page into:
Methods to overcome poor responses and challenges of laser hair removal in dark skin
2 Cutis Institute of Dermatology, Srinagar, Jammu and Kashmir, India
Correspondence Address:
Shehnaz Zulfikar Arsiwala
Renewderm Centre, New Mazgaon Co-op Society, A Wing 3rd Floor, Nesbit Road, Mazgaon, Mumbai, Maharashtra
India
| How to cite this article: Arsiwala SZ, Majid IM. Methods to overcome poor responses and challenges of laser hair removal in dark skin. Indian J Dermatol Venereol Leprol 2019;85:3-9 |
Abstract
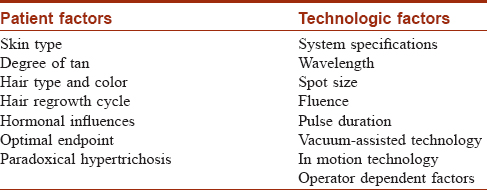
Conventional and advance technologies are available for laser hair removal. Complete and permanent hair reduction is not yet possible by treatment with lasers. Ideal patient for any conventional laser hair removal treatment is one who has thick, dark terminal hair, light skin and normal hormonal status. Factors that contribute to variable outcomes in laser hair removal can be broadly divided into patient related ones and the technology related ones. Skin type, hair color, thickness and density, degree of tan, hormonal dysfunction etc., constitute the patient related factors. The wavelength, fluence, spot size and pulse duration of the laser system are the technology related factors. There are some patients who respond variably, unpredictably or poorly to laser hair removal despite ensuring that indication for treatment is appropriate with adequate parameters of the laser system. This article reviews various patient related and technology related factors which lead to variable-to-poor outcomes in laser hair removal; and various challenges and limitations of laser hair removal technology in patients with dark skin types.
Introduction
Demand for laser hair removal has increased exponentially during the last decade. Traditional methods of hair removal such as threading, plucking and waxing have largely been replaced by interventions using laser and light sources as the latter methods are substantially superior in achieving long term hair reduction. Laser hair removal is said to be permanent when there is a stable decrease in the number of terminal hair for a period longer than the complete hair growth cycle at a given site after treatment.[1] The target chromophore in laser hair reduction is melanin. Laser energy is absorbed by melanin in the hair follicle. Hair bulb, bulge and papilla are heated consequent to the absorption of laser energy. Energy is delivered to the target in lesser time than required for heat diffusion to the surrounding tissue which remains unaffected. Simultaneous cooling of the epidermis to protect it will achieve selective photothermolysis wherein there is selective absorption of wavelength by the chromophore.[1] Evidence indicates that complete, total and persistent hair removal with lasers cannot be achieved.[1] There is evidence which indicates that lasers induce complete but temporary hair loss, followed by partial, permanent hair reduction. Lasers produce significant delay in hair regrowth after treatment, which can last from weeks to months. After laser treatment, the terminal hairs are replaced by fine vellus hairs. Efficacy is improved when treatment is repeated.[1],[2]
Photothermal, photomechanical and photochemical mechanisms contribute to laser hair removal. Photothermal energy of laser causes a rise in temperature in hair bulb and bulge causing thermal destruction of hair follicle. Photomechanical energy initiates shock wave formation and photochemical energy is generated by free radicals.[2]
Wavelengths in the range of 600–1200 nm produced by conventional systems such as ruby (694 nm), long-pulsed alexandrite (755 nm), long-pulsed diode (810 nm), long-pulsed Nd: YAG (1064 nm) and intense-pulsed light can achieve this. Radiofrequency also injures hair photothermally. Q-switched Nd: YAG laser (1064 nm), with or without the addition of a topical carbon suspension, destroys hair thermomechanically.[3],[4]
New techniques include low-fluence laser hair removal applied in motion with a high repetition rate to achieve progressive photothermolysis. Repeated and fast emission of pulses of low energy progressively heats the chromophore to temperatures of 45–50° over a period of time and safeguards the epidermis from overheating as opposed to a sudden rise in temperature to 65° in conventional systems.[5] There are various factors related to patient and technology which could result in variable, unpredictable or poor responses to laser hair removal in spite of ensuring appropriate indications and adequate parameters of laser use. These are reviewed in this article.
Factors that contribute to variable outcomes in laser hair removal can be broadly divided into patient factors and technological factors [Table - 1].
Patient Related Factors
An ideal patient for conventional laser hair removal is one who has thick dark terminal hairs, light skin and normal hormonal status.[1] Patient selection should not be compromised during laser hair removal as these can decrease response to treatment. These are explained in the following sections.
Skin type
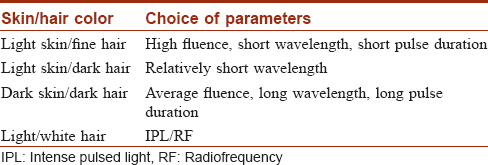
Dark skin types necessitate that sufficient caution is taken for the safe application of a laser hair removal by any wavelength. Clinical studies show that in skin types 4-6, there is increased amount of epidermal melanin which acts as a competing chromophore to melanin in hair bulb and shaft. This leads to a higher frequency of adverse effects. To minimize these adverse reactions, most clinicians use less fluence which can reduce efficacy and response in laser hair removal.
The long-pulsed Nd: YAG laser remains the recommended choice in very dark individuals and tanned patients due to its longer wavelength. Safety of patients with type 5-6 skin is a challenge for laser hair removal due to high density of competing chromophore in the epidermis.[6] A wavelength which is less absorbed by melanin maybe less effective clinically as target chromophore for hair removal laser is melanin in hair bulb and bulge.[7],[8]
A study reported that diode laser was better than the alexandrite laser because emission from the former could penetrate deeper into the dermis.[9]
Compared to intense pulsed light, long-pulsed Nd: YAG laser has been found to be more effective - as reported by both subjects and clinicians.[10],[11] Safety and efficacy of laser hair removal is compromised in patients with darker skin types with short-pulse durations and high fluences.[6],[12]
Tanning of skin
Complications like first or second degree epidermal burns from short wavelengths exist. Some physicians are compelled to use lower fluences to prevent burns at the cost of efficacy. Reports of complications from short wavelengths in the form of first- or second-degree epidermal burns result in use of suboptimal laser fluence and reduces efficacy of the procedure.[3],[13] This is a limitation of laser hair removal in dark skin types as hair reduction can be achieved but at the cost of epidermal burns.
Hair type and color
Terminal hairs, not vellus hairs, are considered suited for laser hair reduction as they absorb laser energy more. Good response to laser hair reduction occurs when the targeted hair has a high concentration of chromophores. Thin fine hairs have less pigment, and hence, are poor choices for laser hair reduction even with best fluences and multiple treatments compared to thick terminal hairs. Hairs less than 30 microns in diameter are not ideal for laser hair removal. When vellus or thin hairs are treated, responses may be poor due to relatively less chromophore in them. This is true when treating areas such as upper lip where chromophore in vellus hairs is less for laser wavelength absorption.[6],[14],[15]
Pigmentation of hair
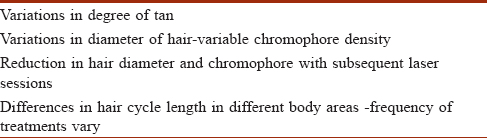
Melanin is the chromophore for laser absorption. Persons with black, brown, red, dark or blonde hairs achieve long-lasting results but those with light blonde or white hairs experience only temporary reduction for up to 12 weeks. However, considerable variations in treatment results are often seen among patients with dark hair.[6] Most patients with brown or black hair obtain a 2- to 6-month growth delay after a single treatment. Though permanent hair loss is not expected in all individuals, lessening of hair density and thickness are.[14],[15] White and gray hairs have no melanin and are not known to respond to lasers. Nd: YAG laser works less effectively than alexandrite and intense pulsed light due to its poor affinity for melanin, which illustrates the role of chromophores in determining responsiveness of hairs to lasers.[16] Some studies have shown that externally applied chromophores such as carbon suspension cause temporary reduction in white or gray hairs.[6],[13],[15],[17] But this is not proven to be an effective hair removal method the dermal papilla and stem cells are not destroyed by this method. These results suggest that photodynamic therapy may damage the nonpigmented hair matrix but not stem cells or dermal papillae. Repeated photodynamic therapy may impair the hair-regeneration capacity via a bystander effect on bulge stem cells or dermal papillae. Study by Shin et al. it was possible to remove nonpigmented hair using photodynamic therapy [Table - 2] and [Table - 3].[18]
Stage of hair cycle
Hair in early anagen phase is most susceptible to laser treatment. Areas with high anagen hair percentages respond well to laser hair removal. After a session of laser hair reduction, re-growth of hair may be delayed up to 6 or 8 weeks; subsequent sessions after very brief intervals are associated with poor outcome. One has to plan the subsequent sessions after taking the hair growth cycles of various body areas into consideration. Duration of anagen phase is different in different areas of the body. An interval of 1-2 months between sessions is optimum and this depends on the body location.
Laser hair removal at short intervals results in inadequate time for initiation of anagen phase that may not allow laser energy absorption in the hair bulb or bulge. Prolonged intervals result in deeper migration of anagen bulb to the subcutis, thus reducing efficacy when shorter wavelength lasers are used. Clinically, this is a limitation as it is difficult to gauge by examination if the hair is in early anagen phase.
How to enable adequate energy diffusion to the bulge is a dilemma. Perifollicular edema and erythema are the only clinical features which can help to gauge the optimum endpoint. If the area to be treated has very high density hair growth, treatment would result in better outcome compared to treatment in a low-density hair growth area [Table - 2] and [Table - 3].[17]
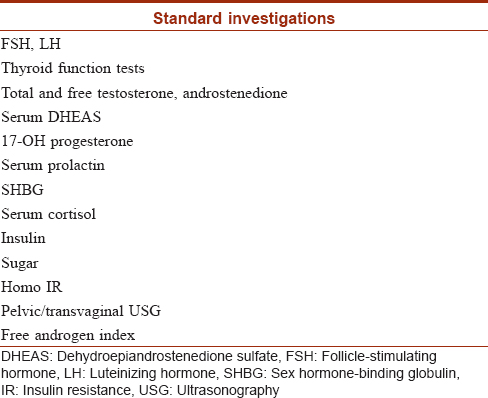
Hormonal influences
Several underlying medical and hormonal factors strongly influence the outcome of laser hair removal from androgen-sensitive areas. These conditions constitute the largest segment of patients who experience variable-to-poor response to laser hair removal. Polycystic ovarian syndrome, thyroid dysfunctions, adrenal hyperplasias and hyperprolactinemia are hormonal dysfunctions which influence hair re-growth following laser hair removal.
Various investigations need to be done before starting laser hair removal in patients suspected to have endocrine diseases. These are shown in [Table - 4]. Some women with mild hirsutism and subtle symptoms and signs of hyperandrogenism can have elevated androgen levels. Hence they also deserve a laboratory evaluation.[16],[17]
To optimize outcomes in variable to poor responsive patients, the following measures are helpful according to hirsutism management guidelines:[19],[20],[21],[22]
- Hirsutism that persists despite six or more months of monotherapy with an oral contraceptive demands additional pharmacological therapies.
- Adding an antiandrogen is justified for women who choose hair removal therapy by laser/photoepilation desiring a more rapid initial response.
- Adding eflornithine cream during treatment for women with known hyperandrogenemia who choose laser hair removal therapy is another reason for starting pharmacological therapies for hirsutism.
A trial of at least 6 months before making changes in dose, changing medication or adding pharmacologic therapy to minimize hair regrowth with lasers is justified. Concomitant hormone therapy in cases of cutaneous hyperandrogenism may overcome poor outcomes of a standalone laser hair reduction procedure.[20],[21]
Establishing the etiology, using evidence-based strategies to improve hirsutism, and treating the underlying disorder are essential for proper management of women with hirsutism.[23],[24]Suppression of cutaneous androgen influence alleviates underlying hormonal imbalance to achieve peripheral androgen blockage. This, along with laser hair removal optimises results. Oral contraceptives cause suppression of production of luteinizing hormone and follicle-stimulating hormone, leading to a decrease in ovarian androgen production and decrease in adrenal androgen. Low-androgenic progestins are preferred as they cause antagonism of 5α-reductase and androgen receptor.[23] Insulin sensitizers such as metformin significantly decrease insulin resistance.[24] Patients with untreated hormonal diseases can have variable-to-poor responses to laser hair removal and require more number of sessions than patients with normal hormone levels.[23],[25]
Usual dosage of spironolactone in hirsutism is 100 to 200 mg daily. It can be used for only the first 10 days of the menstrual cycle (50 or 100 mg dose) and is best combined with an oral contraceptive pill, or can be used in low dose with a combined oral contraceptive pill (cyproterone acetate and ethinyl estradiol).
Finasteride at a dose of 1 mg is occasionally used in the treatment of hirsutism. Metformin and other insulin sensitizers are less effective than antiandrogens in reducing hirsutism. Metformin is effective in inducing ovulation in patients with polycystic ovary syndrome. GnRH analogues may be effective if oral contraceptives and antiandrogen drugs are unsuccessful in patients with severe hyperandrogenism. They suppress secretion of luteinizing hormone and synthesis of ovarian androgen.[23]
Hyperprolactinemia
During pregnancy there is an increase in the levels of prolactin Hyperprolactin state has a melanocyte stimulating effect. All light therapies are ineffective for hair reduction in cases of hyperprolactinemia due to pregnancy or amenorrhea galactorrhea syndrome which upregulate melanocyte stimulating hormone in stem cells of the hair.
In authors' experience, hyperprolactinemia is a very important factor for poor laser hair response. The outcome of laser hair reduction is poor despite the patient being on treatment with medications. These patients according to an author's experience (unpublished data) have prolactin levels between 30 and 90 ng/dl and are refractory to any modality - conventional or advanced- for laser hair removal. There is strong evidence for less response to laser hair removal in polycystic ovarian disease.[20],[21] Hyper prolactinemic states are often associated with polycystic ovarian syndrome.[20],[21] Specific studies on laser response in hyperprolactinemic states are needed.
Hyperprolactinemic states cause upregulation of melanocyte-stimulating hormone, influence reactivation of progenitor stem cells in hair bulb and bulge and may cause poor response to laser hair removal. Hirsutism of hyperprolactinemia is usually of low grade with terminal hair being fine and long rather than being thick and dark. Low chromophore may be another reason for poor response in this condition.
Paradoxical Hypertrichosis after Laser Removal
Laser treatment has also been known to cause a paradoxical increase in hair growth. Even though hair follicles are destroyed, it is likely that vellus hair follicles may persist and these can continually be converted into terminal pigmented hairs in the presence of androgen excess. This probably explains why many women experience hair regrowth after laser hair removal. Paradoxical hypertrichosis is seen with all laser types with low fluences. Paradoxical hypertrichosis is seen in those with dark skin. Chin and neck are common sites for paradoxical hypertrichosis reported in approximately 6-10% of cases of laser hair reduction.[26]
Uniform volumetric heating with specific heat ratio may destroy the bulge that houses progenitor stem cells that cause paradoxical regrowth under hormonal excess. The accumulative and sustainable heat causes irreversible damage to biological regulatory factors of the hair follicle (stem cells, etc.). Paradoxical hypertrichosis is treated with further sessions of high fluence and short-pulse duration, increased cooling and stacking of pulses.[26],[27]
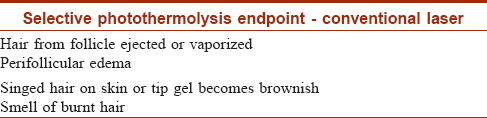
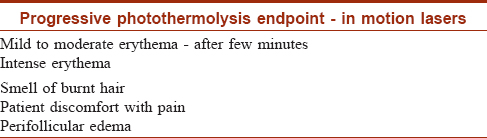
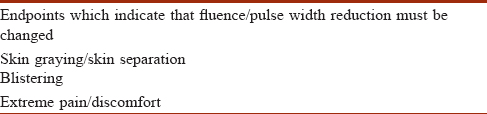
Optimal endpoint in conventional, large spot size or in-motion laser technologies
Appropriate end point indicates successful laser absorption by the chromophore and should be observed post treatment. However, this is not absolutely essential as hair reduction does occur in absence of visible end point in dark skinned individuals. [Table - 5], [Table - 6], [Table - 7] highlight endpoints for conventional and in motion laser hair removal techniques.
Technological Factors
Device-based factors
Numerous laser and light-based devices are employed for permanent hair reduction.
While there are scientific studies demonstrating the efficacy of each of these devices, the results vary a lot among these studies. Employing the right laser device according to the patient's skin and hair type is of paramount importance in achieving satisfactory results. There are limited number of studies on the comparative efficacy and safety of different hair removal devices.
Comparison of different laser and light-based devices
Majority of the studies have documented a superior efficacy of alexandrite and diode laser systems in hair removal in comparison to other lasers or light-based devices. In a study that compared the efficacy of three laser devices, a mean hair reduction of 59.5, 70.3 and 47.4% was reported after three sessions with diode, alexandrite and Nd: YAG lasers, respectively.[28]
In a randomized, split-face study, a mean reduction in hair count of 46% and 27% was reported after alexandrite and intense-pulsed light systems, respectively.[29]
In a comparative study on long-pulsed Nd: YAG laser and intense-pulsed light system in skin types 4–6, the former device was found to be more effective than the latter for hair removal with fewer side effects.[30]
Similarly some recent studies have demonstrated superior hair reducing efficacy of Nd: YAG laser over intense-pulsed light system in dark skin.[10],[30]
Factors Related to Laser Hair Removal System
Fluence
A proper fluence is of paramount importance in getting the required therapeutic effect in laser hair removal. While higher fluences can increase efficacy they can also increase adverse effects. The right fluence is determined by the highest tolerable energy or a test patch that generates perifollicular erythema and edema.
With a diode laser, fluences in the range of 30–35 J/cm2 are adequate for Type 2 to 3 skin. For darker skin types the fluences used are relatively less, usually in the range of 20–24 J/cm2. Using suboptimal fluence is one of the most important causes of a poor response to laser hair removal.
With lower fluences, temporary rather than permanent removal is achieved. Roosen et al.31 st udied the effect of low fluence photoepilation on hair follicles. Their findings suggest that transition of anagen follicles to catagen phase happens with low fluences. Long-term hair removal largely depends on hair color, skin color and the tolerated fluence.
Spot size
Spot size means the size of the laser probe or head that is used during a laser procedure. This in effect means the area over which the laser beam is delivered in a single shot of laser treatment. The importance of spot size lies in scattering of laser energy by collagen fibers outside the treatment zone. More photons are likely to get scattered if smaller spot sizes are used, while with larger spot sizes a higher percentage of photons are delivered to the skin and are likely to remain within the treatment area.[32] Thus, in laser hair removal, larger spot sizes are usually associated with a better treatment response. One comparative study showed a better response with an 18-mm spot size in comparison with 12-mm spot size in axillary hair removal.[15],[33] Therefore, optimum spot size for laser delivery is one of the important factors for achieving a significant therapeutic response in laser-assisted hair removal.
Pulse duration
Optimal pulse duration in hair removal is calculated based on thermal relaxation time. For terminal hairs, the calculated thermal relaxation time is in the range of 100 ms. Thus, the pulse duration used for laser hair removal has to be in this range only. Inadequate pulse duration is another important reason for a subnormal therapeutic effect.[34],[35]
Vacuum-assisted low-fluence laser hair removal
Using vacuum while performing laser hair removal assists in specifically targeting the chromophore in a better fashion in laser hair removal. Low-fluence diode laser using a larger spot size under vacuum has been shown to be as efficacious as standard hair removal with high-fluence diode laser. A comparative study on 14 patients who received five sessions of laser hair removal in the axillae with these two techniques demonstrated comparable results. In addition, the lower fluence vacuum-based technique was found to be less painful than the standard technique.[12],[36]
Vacuum-assisted low fluence hair removal has been successfully used in tackling large body areas as the treatment time gets shortened with larger spot size used in this technique. Zhou et al. suggest that the significantly low levels of pain obtained during treatment with the vacuum-assisted large handpiece technology are due to the negative pressure generated by the vacuum.[12]
Evidence from literature indicates that even at low level of fluence (12 J/cm2), lasers with large spot size and vacuum assisted technology were shown to provide comparable hair reduction as the conventional diode laser (25–30 J/cm2) with 3-month follow-up after five treatment sessions.[35] Hashimi et al. highlighted the effect of vacuum in creating a three-dimensional geometry to lift the skin while treating and combined it with gold-plated chamber. This indicates that when target is closer to the hand piece in vacuum technology there is better delivery of laser light compared to the relatively flat surface of conventional diode laser handpiece.[36]
Operator-Based Factors
Physician versus non-physician operator
In laser hair removal clinics, the procedure is either performed by a trained physician or by a trained nursing staff. Efficacy of laser hair removal is dependent not only on the laser device but also on who is performing the procedure. The best evidence favoring this statement has come from a review of the complications associated with non-physician supervised laser hair removal. The incidence of adverse effects has been shown to be significantly associated with non-physician performed laser hair removal.[37],[38],[39]
Technique
Improper technique employed during laser hair removal, resulting in skip areas, can lead to poor or incomplete therapeutic response with islands of untreated hair. For example, with standard diode laser, one has to overlap the laser shots to the tune of 10% of the area owing to the presence of metallic circumference of the laser probe.
Cooling devices and methods are of crucial importance in laser hair removal, especially in skin types 3–5, to facilitate epidermal protection and to prevent laser burns. While external cooling can be achieved with ice compresses or cryogen cooling, most current technologies have integrated cooling systems- some of them having graded cooling methods to achieve low-to-very low temperatures.[1],[6],[7]
Other possible factors which influence response to laser hair removal include doing laser treatment on epilated or waxed treatment areas; not shaving the treatment area properly; or doing laser treatment on a freshly bleached hair all of which lead to incomplete or poor response.[40]
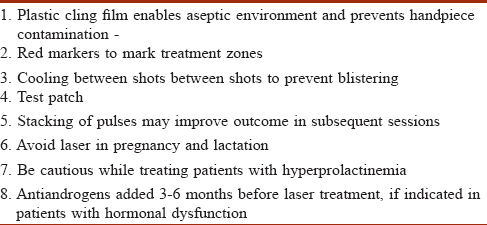
[Table - 8] highlights the tips to optimize the efficacy of laser hair removal.
Conclusion
Successful laser hair removal outcomes depend on adequate patient profile and technological parameter of the laser machines. When responses are poor despite standard parameters and usage in appropriate indications, one has to consider the various factors such as hormonal influences, technological specifications of the laser system and multiple complex variables in order to optimize the outcomes of laser hair removal in dark skin types.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Haedersdal M, Haak CS. Hair removal. Curr Probl Dermatol 2011;42:111-21.
[Google Scholar]
|
| 2. |
Lawrence WT. Hair removal laser and nonlaser light systems. Plastic surgery educational foundation DATA committee. Plast Reconstr Surg 2000;105:459-61.
[Google Scholar]
|
| 3. |
Dierickx CC. Hair removal by lasers and intense pulsed light sources. Dermatol Clin 2002;20:135-46.
[Google Scholar]
|
| 4. |
Altshuler GB, Anderson RR, Manstein D, Zenzie HH, Smirnov MZ. Extended theory of selective photothermolysis. Lasers Surg Med 2001;29:416-32.
[Google Scholar]
|
| 5. |
Arsiwala S. Lasers in dermatology: Laser hair removal. In: Majid I, editor. IADVL Recent Advances in Dermatology. 1st ed. New Delhi: Jaypee; 2016. Chp. 53, 517-24.
[Google Scholar]
|
| 6. |
Battle EF Jr., Hobbs LM. Laser-assisted hair removal for darker skin types. Dermatol Ther 2004;17:177-83.
[Google Scholar]
|
| 7. |
Chan CS, Dover JS. Nd: YAG laser hair removal in Fitzpatrick skin types IV to VI. J Drugs Dermatol 2013;12:366-7.
[Google Scholar]
|
| 8. |
Mittal R, Sriram S, Sandhu K. Evaluation of long-pulsed 1064 nm Nd: YAG laser-assisted hair removal vs. multiple treatment sessions and different hair types in Indian patients. J Cutan Aesthet Surg 2008;1:75-9.
[Google Scholar]
|
| 9. |
Mustafa FH, Jaafar MS, Ismail AH, Mutter KN. Comparison of alexandrite and diode lasers for hair removal in dark and medium skin: Which is better? J Lasers Med Sci 2014;5:188-93.
[Google Scholar]
|
| 10. |
Ismail SA. Long-pulsed Nd: YAG laser vs. intense pulsed light for hair removal in dark skin: A randomized controlled trial. Br J Dermatol 2012;166:317-21.
[Google Scholar]
|
| 11. |
Rao J, Goldman MP. Prospective, comparative evaluation of three laser systems used individually and in combination for axillary hair removal. Dermatol Surg 2005;31:1671-6.
[Google Scholar]
|
| 12. |
Zhou ZC, Guo LF, Gold MH. Hair removal utilizing the LightSheer duet HS hand piece and the LightSheer ET: A comparative study of two diode laser systems in Chinese women. J Cosmet Laser Ther 2011;13:283-90.
[Google Scholar]
|
| 13. |
Nanni CA, Alster TS. Laser-assisted hair removal: Side effects of Q-switched Nd: YAG, long-pulsed ruby, and alexandrite lasers. J Am Acad Dermatol 1999;41:165-71.
[Google Scholar]
|
| 14. |
Haedersdal M, Wulf HC. Evidence-based review of hair removal using lasers and light sources. J Eur Acad Dermatol Venereol 2006;20:9-20.
[Google Scholar]
|
| 15. |
Ibrahimi OA, Avram MM, Hanke CW, Kilmer SL, Anderson RR. Laser hair removal. Dermatol Ther 2011;24:94-107.
[Google Scholar]
|
| 16. |
Karaca S, Kaçar SD, Ozuğuz P. Comparison of SHR mode IPL system with alexandrite and Nd: YAG lasers for leg hair reduction. Balkan Med J 2012;29:401-5.
[Google Scholar]
|
| 17. |
Small R. Laser hair removal. In: Mayeaux S, editor. The Essential Guide to Primary Care Procedures. Philadelphia, PA: Lippincott Williams and Wilson; 2009. p. 234-48.
[Google Scholar]
|
| 18. |
Shin H, Yoon JS, Koh W, Kim JY, Kim CH, Han KM, et al. Nonpigmented hair removal using photodynamic therapy in animal model. Lasers Surg Med 2016;48:748-62.
[Google Scholar]
|
| 19. |
Martin KA, Chang RJ, Ehrmann DA, Ibanez L, Lobo RA, Rosenfield RL, et al. Evaluation and treatment of hirsutism in premenopausal women: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 2008;93:1105-20.
[Google Scholar]
|
| 20. |
McGill DJ, Hutchison C, McKenzie E, McSherry E, Mackay IR. Laser hair removal in women with polycystic ovary syndrome. J Plast Reconstr Aesthet Surg 2007;60:426-31.
[Google Scholar]
|
| 21. |
Lapidoth M, Dierickx C, Lanigan S, Paasch U, Campo-Voegeli A, Dahan S, et al. Best practice options for hair removal in patients with unwanted facial hair using combination therapy with laser: Guidelines drawn up by an expert working group. Dermatology 2010;221:34-42.
[Google Scholar]
|
| 22. |
Gacaferri Lumezi B, Goci A, Lokaj V, Latifi H, Karahoda N, Minci G, et al. Mixed form of hirsutism in an adolescent female and laser therapy. Iran Red Crescent Med J 2014;16:e9410.
[Google Scholar]
|
| 23. |
Agrawal NK. Management of hirsutism. Indian J Endocrinol Metab 2013;17:S77-82.
[Google Scholar]
|
| 24. |
Nawrocka-Rutkowska J, Ciećwież S, Marciniak A, Brodowska A, Wiśniewska B, Kotlega D, et al. Insulin resistance assessment in patients with polycystic ovary syndrome using different diagnostic criteria – impact of metformin treatment. Ann Agric Environ Med 2013;20:528-32.
[Google Scholar]
|
| 25. |
Karn D, Krishna C, Timalsina M, Gyawali P. Hormonal profile and efficacy of long pulse Nd-YAG laser in treatment of hirsutism. J Nepal Health Res Counc 2014;12:59-62.
[Google Scholar]
|
| 26. |
Alajlan A, Shapiro J, Rivers JK, MacDonald N, Wiggin J, Lui H, et al. Paradoxical hypertrichosis after laser epilation. J Am Acad Dermatol 2005;53:85-8.
[Google Scholar]
|
| 27. |
Desai S, Mahmoud BH, Bhatia AC, Hamzavi IH. Paradoxical hypertrichosis after laser therapy: A review. Dermatol Surg 2010;36:291-8.
[Google Scholar]
|
| 28. |
Khoury JG, Saluja R, Goldman MP. Comparative evaluation of long-pulse alexandrite and long-pulse Nd: YAG laser systems used individually and in combination for axillary hair removal. Dermatol Surg 2008;34:665-70.
[Google Scholar]
|
| 29. |
McGill DJ, Hutchison C, McKenzie E, McSherry E, Mackay IR. A randomised, split-face comparison of facial hair removal with the alexandrite laser and intense pulsed light system. Lasers Surg Med 2007;39:767-72.
[Google Scholar]
|
| 30. |
Goh CL. Comparative study on a single treatment response to long pulse Nd: YAG lasers and intense pulse light therapy for hair removal on skin type IV to VI – is longer wavelengths lasers preferred over shorter wavelengths lights for assisted hair removal. J Dermatol Treat 2003;14:243-7.
[Google Scholar]
|
| 31. |
Roosen GF, Westgate GE, Philpott M, Berretty PJ, Nuijs T, Bjerring P, et al. Temporary hair removal by low fluence photoepilation: Histological study on biopsies and cultured human hair follicles. Lasers Surg Med 2008;40:520-8.
[Google Scholar]
|
| 32. |
Grunewald S, Bodendorf MO, Zygouris A, Simon JC, Paasch U. Long-term efficacy of linear-scanning 808 nm diode laser for hair removal compared to a scanned alexandrite laser. Lasers Surg Med 2014;46:13-9.
[Google Scholar]
|
| 33. |
Gupta G. Diode laser: Permanent hair “Reduction” not “Removal”. Int J Trichology 2014;6:34.
[Google Scholar]
|
| 34. |
Esmat S, Abdel-Halim MR, El-Tawdy A, Fawzy MM, Ragheb A, Hasan N, et al. Does increasing the pulse duration increase the efficacy of long pulsed Nd: YAG laser assisted hair removal? A split-chin clinical trial. Eur J Dermatol 2014;24:391-2.
[Google Scholar]
|
| 35. |
Halachmi S, Lapidoth M. Low-fluence vs. standard fluence hair removal: A contralateral control non-inferiority study. J Cosmet Laser Ther 2012;14:2-6.
[Google Scholar]
|
| 36. |
Vano-Galvan S, Jaen P. Complications of nonphysician-supervised laser hair removal: Case report and literature review. Can Fam Physician 2009;55:50-2.
[Google Scholar]
|
| 37. |
Jalian HR, Jalian CA, Avram MM. Common causes of injury and legal action in laser surgery. JAMA Dermatol 2013;149:188-93.
[Google Scholar]
|
| 38. |
Bayle P, Saval F, Rougé D, Telmon N. Complications after laser hair removal: The standpoint of a dermatological legal expert regarding liability. Ann Dermatol Venereol 2015;142:176-82.
[Google Scholar]
|
| 39. |
Kelsall D. Laser hair removal: No training required? CMAJ 2010;182:743.
[Google Scholar]
|
| 40. |
Mustafa F, Jaafar MS. Shaving area of unwanted hair before laser operation is useful in cosmetic procedure: A simulation study. Journal of Dermatology & Dermatologic Surgery 2015;19:36-42.
[Google Scholar]
|
Fulltext Views
42,948
PDF downloads
6,547





