Translate this page into:
Microsporum canis tinea capitis in a centenarian patient
2 Department of Dermatology, University of Athens, "A. Sygros" Hospital, Athens, Greece
3 Department of Mycology, University of Athens, "A. Sygros" Hospital, Athens, Greece
Correspondence Address:
Efstathios Rallis
11 Pafsaniou Street, Athens, GR-11635
Greece
| How to cite this article: Rallis E, Koumantaki-Mathioudaki E, Papadogeorgakis H. Microsporum canis tinea capitis in a centenarian patient. Indian J Dermatol Venereol Leprol 2011;77:626 |
Sir,
Tinea capitis is a dermatophyte infection of the scalp and hair. It is overwhelmingly an infection of prepubertal children, but is being increasingly recognized in adults though it was once considered to be uncommon in this age-group. [1] Microsporum canis (M. canis) is the dominant cause of tinea capitis in Greece. [2] In this article we present probably the oldest patient with M. canis tinea capitis to be reported in the literature.
A 100-year-old immunocompetent female was referred to our hospital because of scaly alopecia with pustules and crusts of 2 months duration [Figure - 1]. Hairs in the affected area were gray and breaking off just above the level of the scalp. Scaly lesions on the forehead and the eyebrows, resembling seborrheic dermatitis, could also be seen. The lesions had not responded to oral amoxicillin and topical fusidic acid, which had been prescribed by her physician.
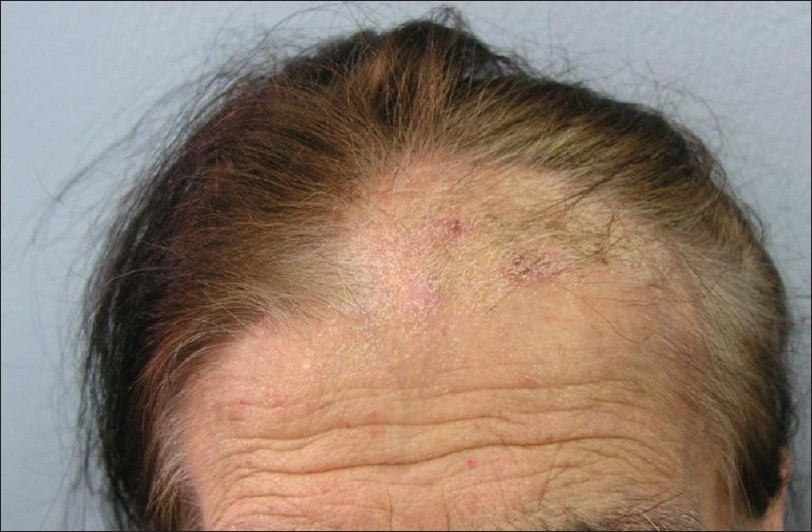 |
| Figure 1: Microsporum canis tinea capitis in a centenarian female. Scaly lesions on the forehead and the eyebrows can be seen |
The patient had a body weight of 48 kg. She lived in a village in the mountains. She mentioned no contact with animals and did not use any clothing for the head. No fungal infections were detected on other parts of her skin or her nails and hair and none of her close family members had been similarly affected. Despite her age, the medical history was unremarkable apart from a history of chronic gastritis for which she was not receiving any medication. She had no evidence of any sort of immunological deficiency.
Culture of bacterial swabs was negative. Mycological examination was performed on the scales from the lesion and hair samples. Direct examination of a 20% KOH preparation was positive. The specimens were also inoculated on Sabouraud 2% glucose-chloramphenicol agar and Sabouraud 2% glucose cycloheximide-chloramphenicol agar and revealed the presence of the ectothrix M. canis [Figure - 2]. The scalp of the patient was also examined under a Wood′s lamp and it fluoresced a green color.
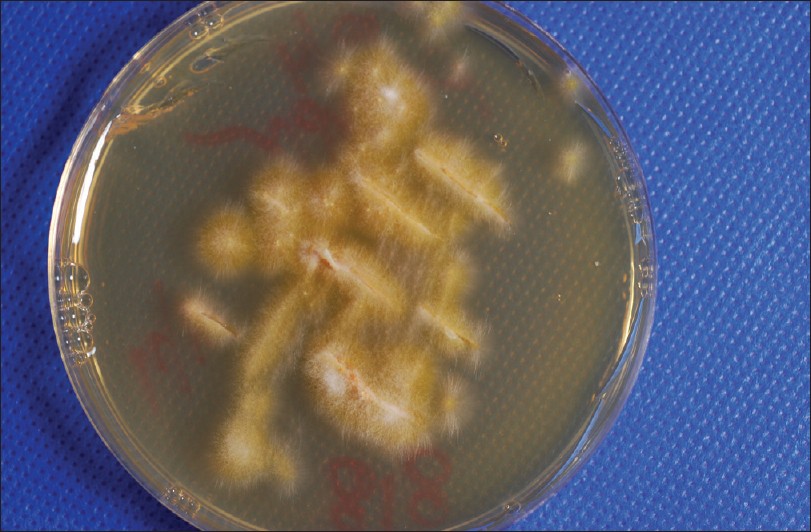 |
| Figure 2: Culture of the specimens revealed the presence of M. canis |
We decided to treat her with itraconazole pulse therapy. Each pulse comprised of capsule itraconazole 100 mg (Verisfield, Athens, Greece) twice daily for 1 week, with an interval of 3 weeks between the pulses. [3] To avoid gastrointestinal symptoms and/or exacerbation of gastritis due to itraconazole and because of her low body weight, we decided to administer a dose of 100 mg of the medication for three pulses instead of the standard 5 mg/kg/day; in case of treatment failure, we would switch to a continuous regimen of 100 mg itraconazole.
After 2 months of pulse therapy she called us over the phone as she was not able to visit our department. She reported that her hair had gradually grown back again and we suggested that she discontinue the treatment. Three months after discontinuation of the treatment she visited the department again. There was complete remission of the dermatophyte infection; all scaly lesions had subsided and there was no evidence of recurrence [Figure - 3]. Mycological examination was negative. She did not report any adverse events during the treatment period.
 |
| Figure 3: Complete resolution was achieved after two 1-week pulses of itraconazole |
Dermatophytic colonization of the scalp usually disappears at puberty. Tinea capitis in adults has been reported to occur in patients who are immunosuppressed or HIV-infected; [4] however, there is not enough evidence to support this. Devliotou-Panagliotidou et al. [1] reported 35 adults with tinea capitis, 27 of them with a typical pattern of menopause but none with any immunological deficiency.
A female predominance in the adult cases has been reported but has not been explained. [5] Numerous factors have been incriminated, such as contact with affected family members, hormonal differences, the composition of sebum, and immunological deficiency.
Griseofulvin has been the gold standard for the treatment of tinea capitis. Little data is available about the efficacy of fluconazole in tinea capitis. [6] Terbinafine has been licensed since 1996 for the treatment of mycotic infections of the scalp in children and adults. [7] However, the cure rates with terbinafine are poorer when the causative organism is M. canis than when it is T. tonsurans and T. violaceum. [8] Itraconazole is probably the ideal alternative to griseofulvin for fungal infections of the scalp. [3]
Our patient responded very well to the oral pulse therapy regimen of itraconazole. Itraconazole represents a good therapeutic choice for ectothrix fungal infections of the scalp. In such cases, concomitant use of ketoconazole shampoo 2-3 times a week is also recommended to prevent fomite transmission.
| 1. |
Devliotou-Panagiotidou D, Koussidou-Eremondi T, Chaidemenos GC, Theodoridou M, Minas A. Tinea capitis in adults during 1981-95 in northern Greece. Mycoses 2001;44:398-400.
[Google Scholar]
|
| 2. |
Koussidou-Eremondi T, Devliotou-Panagiotidou D, Mourellou-Tsatsou O, Minas A. Epidemiology of dermatomycoses in children living in Northern Greece 1996-2000. Mycoses 2005;48:11-6.
[Google Scholar]
|
| 3. |
Koumantaki-Mathioudaki E, Devliotou-Panagiotidou D, Rallis E, Athanassopoulou V, Koussidou-Eremondi T, Katsambas A , 0 et al . Is itraconazole the treatment of choice in Microsporum canis tinea capitis? Drugs Exp Clin Res 2005;31(Suppl):11-5.
[Google Scholar]
|
| 4. |
Cremer G, Bournerias I, Vandemeleubroucke E, Houin R, Revuz J. Tinea capitis in adults: Misdiagnosis or reappearance? Dermatology 1997;194:8-11.
[Google Scholar]
|
| 5. |
Aste N, Pau M, Biggio P. Tinea capitis in adults. Mycoses 1996;39:299-301.
[Google Scholar]
|
| 6. |
Elewski BE. Tinea capitis: A current perspective. J Am Acad Dermatol 2000;42:1-20.
[Google Scholar]
|
| 7. |
Ginter-Hanselmayer G, Smolle J, Gupta A. Itraconazole in the treatment of tinea capitis caused by Microsporum canis: Experience in a large cohort. Pediatr Dermatol 2004;21:499-502.
[Google Scholar]
|
| 8. |
Koumantaki E, Kakourou T, Rallis E, Riga P, Georgalla S. Doubled dose of oral terbinafine is required for Microsporum canis tinea capitis. Pediatr Dermatol 2001;18:339-42.
[Google Scholar]
|
Fulltext Views
3,191
PDF downloads
2,551





