Translate this page into:
Minimizing side effects of systemic corticosteroids in children
Correspondence Address:
C T Deshmukh
Baug-E-Sara, Ground Floor, 16 Nepean Sea Road, Mumbai - 400 036
India
| How to cite this article: Deshmukh C T. Minimizing side effects of systemic corticosteroids in children. Indian J Dermatol Venereol Leprol 2007;73:218-221 |
Abstract
Corticosteroids are potent drugs used in management of various inflammatory and autoimmune disorders. The antiinflammatory effects of corticosteroids cannot however be separated from their metabolic effects. Children are more vulnerable to their side effects, particularly the effects on growth, immunity and adrenal suppression. It is essential for the treating physician to be aware of the side effects and the measures to be taken to minimize them. A side effect that is unique to children is growth suppression, which is helped by alternate day treatment. Administration of small doses of prednisolone (10-15 mg/day or < 0.5 mg/kg/day single dose) on alternate days, does not slow growth velocity significantly. The potency of dexamethasone and betamethasone in suppressing growth is nearly 18 times higher than that of prednisolone. There is some evidence that the administration of growth hormone can reverse these changes.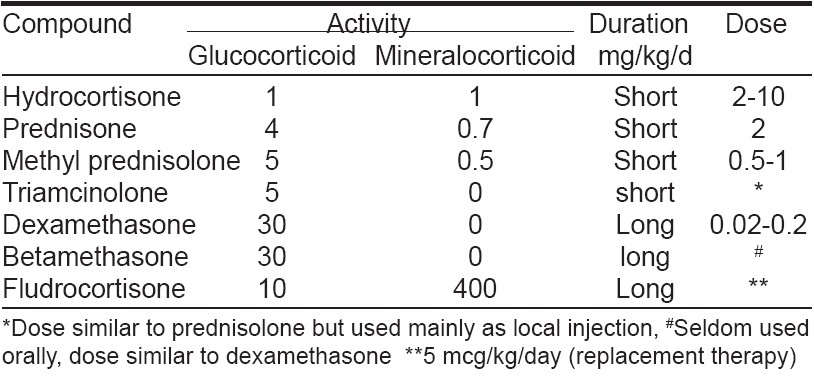
Corticosteroids are potent medications that have been extensively used to treat many inflammatory and autoimmune conditions. They have been used in a variety of life-threatening and disabling conditions and have saved or improved many lives. However, they cause numerous side effects on various body systems and are also one of the most misused medicines. In UK alone, it is estimated that more than 250,000 people are taking systemic steroids and at least 10% of all children require some form of glucocorticoids during their childhood. [1]
Some of the indications of systemic glucocorticoids in pediatrics include rheumatoid arthritis, ulcerative colitis, asthma and Crohn′s disease. In pediatric dermatology, long-term systemic steroids may be used for the treatment of erythroderma due to atopic eczema, pustular psoriasis, childhood pemphigus, chronic bullous dermatosis of childhood, systemic lupus erythematosus, pyoderma gangrenosum or complicated hemangiomas. The doses required in these situations are much higher than those given in replacement regimens used for Addison′s disease. Children taking such pharmacological doses of systemic steroids need to be carefully monitored to minimize the adverse effects. [2],[3]
Choice of Corticosteroid
Corticosteroids have two groups of actions: glucocorticoid effects (metabolic changes, antiinflammatory effects) and mineralocorticoid effects (retention of salt and water, loss of potassium and hydrogen). [4]
Hydrocortisone is short-acting and is used orally for replacement therapy in adrenal insufficiency (in combination with fludrocortisone). Hydrocortisone sodium succinate, the water-soluble derivative, is administered parenterally for a quicker effect in emergencies.
Prednisolone is widely used orally in the acute and long-term management of various disorders and for antiinflammatory and immunosuppressant effects. Prednisone is a prodrug, converted in normal circumstances in the body to prednisolone.
Methylprednisolone has even less mineralocorticoid activity than prednisone / prednisolone while having a similar duration of action and may be preferred when mineralocorticoid effect is particularly undesirable. An alternate day regimen should be considered during long-term therapy.
Dexamethasone is highly potent, long-acting, with minimal mineralocorticoid activity and is used most often in the management of acute disorders. It is not suitable for alternate day regimens where the aim is to maintain the responsiveness of the hypothalamic-pituitary-adrenal (HPA) axis. Prolonged treatment is associated with severe suppression of the HPA axis; hence, it should generally be reserved for short-term management of specific indications.
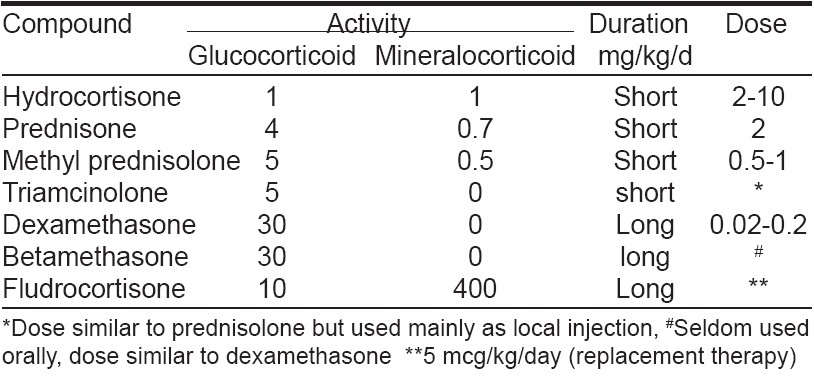
Betamethasone, similar to dexamethasone, is unsuitable for long-term alternate-day therapy due to its long duration of action [Table - 1].
Alternative forms of glucocorticoids such as deflazacort, an oxazolone derivative of prednisolone, appear to have fewer effects on growth and corticosteroid-induced osteoporosis, but are not used in common practice.
Physiological Dose of Steroids
Physiologic replacement dose for hydrocortisone is 10-20 mg/m 2 /day in three divided doses (0.5 mg/kg/day), which is approximately equivalent to 5-7 mg/day of prednisolone.
Risks of Steroid Side Effects
The risk of side effects depends on the
- Dose: low dose (< 10 mg/day of prednisone), medium dose (10-20 mg/day), high dose (> 20 mg/day).
- Type of steroid: (long-acting or short-acting)
- Length of treatment: (Long-term treatment > 3 months)
- Other medical problems.
Minimizing Corticosteroid Side Effects
The adverse effects of corticosteroids seen during short-term therapy include increased appetite, weight gain, fluid retention, gastritis, headache, mood swings, increase in blood sugar, hypertension and glaucoma. Adverse effects seen when therapy is given for longer duration include suppressed immunity, increased susceptibility to infections, increased cholesterol levels, weight gain, osteoporosis, deposition of body fat, thinning of skin, cataracts, stunting and hypothalamopituitary axis suppression.
Fluid and electrolyte balance
The effect of glucocorticosteroids on fluid and electrolytes is due to their mineralocorticoid effect. This causes salt and water retention leading to edema, weight gain and hypertension. The potassium loss leading to hypokalemia can cause severe weakness.
A diet low in sodium and rich in potassium should be followed and very rarely, potassium supplements may be required in children. Monitoring blood pressure at each visit is important, however, anti-hypertensives are rarely required in children. Fluid and electrolyte problems may be more dangerous in patients with associated cardiac illness.
Metabolic disturbances
Corticosteroids affect all metabolic pathways in the body. There is a 10-20% increase in blood sugar levels, mainly due to neoglucogenesis and reduced sensitivity to insulin. If the pancreatic function is normal, generally, diabetes does not develop. In children, it is essential to check blood sugar every six months or when there is development of persistent oral thrush. Frank diabetes is rare in children and is reversible and requires only slight modifications in diet. Hypoglycemic agents are not required in children.
Neoglucogenesis leads to protein breakdown in muscle, skin and bone leading to delayed wound healing, skin and muscle atrophy. Reduction of collagen in tissues makes them fragile. This particularly affects the skin, membranes, capillaries and bone.
Fat redistribution
Glucocorticoids increase lipid levels because of increased lipid production in liver and due to lipolysis from adipose tissue. Corticosteroid therapy causes redistribution of carbohydrate, fat and protein reserves. This along with the increase in appetite leads to the Cushingoid habitus (moon facies, buffalo hump and central obesity). Weight gain can be minimized by early calorie-controlled diet in patients who are on long-term steroid therapy.
Osteoporosis
Glucocorticoids have a suppressive effect on osteoblastogenesis in the bone marrow leading to decreased bone formation. They also promote calcium loss through the kidneys and gut and this negative calcium balance leads to increased bone remodeling. Moreover, there is increased osteoclastic activity due to secondary hyperparathyroidism.
Extent of bone loss and deterioration in short-term growth are dependent on the type and dose of the glucocorticosteroid and are greatest in the first six months of treatment. These changes are more in trabecular bone than in cortical bone. This manifests with severe backache and bone pains due to fractures and involvement of the vertebrae and the long bones. Avascular necrosis may be seen in some patients. There is usually no benefit in alternate day therapy; however the steroid-induced bone loss appears to be reversible. Bone mineral densitometry should be done before therapy, at six months after starting steroids and then annually. A lateral spine X-ray should be done to rule out a fracture if there is a persistent symptom of backache. Regular exercise, calcium and calcitriol (Vitamin D3) should be advised to prevent this complication. Thiazide diuretics decrease the urinary excretion of calcium and may be beneficial in severe cases. Antiresorptive agents like bisphosphonates (pamidronate, alendronate) have been used frequently in adults. Bisphosphonates decrease recruitment and function of osteoclasts and hence reduce bone turnover. Bisphosphonates are used routinely in children with osteogenesis imperfecta; they are also used in childhood and adolescence osteoporosis. It may be used to prevent steroid-induced bone resorption, particularly when symptomatic with severe pain or when bone mineral densitometry shows changes. [1]
Growth suppression
Corticosteroids inhibit linear growth. The mechanism of this effect is unknown but may involve a combination of reduced growth hormone production and a direct inhibitory effect on bone and connective tissue. Growth suppression is more likely if steroids are given for more than six months. Apparent slow growth may be more due to a delayed puberty than actual side effects of the corticosteroids.
It is important to monitor growth in children undergoing steroid therapy using growth charts. Unlike the other side effects of steroids, growth suppression is relieved by alternate day treatment. Doses of prednisolone ≤ 10-15 mg given on alternate days, do not slow down growth velocity significantly. However, this may not be effective in control of some of the inflammatory conditions. The potency of dexamethasone in suppressing growth is 18 times higher than that of prednisolone. There is some evidence that the administration of growth hormone can reverse these changes. Administration of deflazacort (oxazoline derivative of prednisolone), an alternative form of prednisolone, appears to have fewer effects on growth and corticosteroid-induced osteoporosis, but is not being commonly used. It is also important to rule out malnutrition as a cause of poor growth. [1],[5],[6],[7]
Myopathy
Corticosteroids cause muscle wasting and weakness due to decreased muscle protein synthesis and increased protein catabolism in more than 60% of the cases. Proximal muscles are affected to a greater extent and recovery is slow and sometimes incomplete. It is important to rule out hypokalemia in such cases, as it can be easily corrected.
Ophthalmic side effects
Long-term use of corticosteroids can cause cataract, which dose not regress even after stopping therapy; very rarely glaucoma can develop in children.
HPA axis suppression
Corticosteroids suppress the release of corticotrophin-releasing hormone and adrenocorticotropic hormone (ACTH) through a negative feedback cycle. Eventually the adrenals atrophy and do not produce corticosteroids in response to body stress. Adrenal suppression shows marked individual variations. A short course of steroid therapy (up to seven days) usually produces no significant suppression of the adrenals. However, a two-week therapy with steroids has the potential to cause suppression up to one year. The manifestations of steroid withdrawal after chronic therapy are mainly due to the failure of the body to produce endogenous steroids due to suppression of the HPA axis. The manifestations are varied and include weakness, fatigue, weight loss, nausea and vomiting, hypoglycemia, dehydration, electrolyte imbalance, hypotension, abdominal pain, joint pain, muscle pain, headache and even fever.
The most important aspect of prevention of this problem is the awareness of the dangers of stopping steroids suddenly. It is important to taper the dose gradually and even more important to increase the dose during stress, surgery or severe medical illness. [4]
Guidelines for Steroid Tapering
Long-term steroids should be tapered gradually to allow the adrenal glands to resume cortisol production. The first step is reduction from pharmacological to physiological doses. This depends on the disease activity and the level of control with steroids. The next step is to taper from physiological dose to complete withdrawal and this depends on the degree of HPA suppression.
Short courses of corticosteroids (less than a week) generally do not require any tapering of the dose. Courses of corticosteroids given for less than a month will need to be tapered over 7-14 days till a physiological dose is reached. Therapy for more than a month will require the dose to be tapered gradually every 15-30 days till the physiological dose is reached. Once the physiological dose is reached in patients taking long-term corticosteroids, the dose of steroids ideally needs to be increased during stress for the next 6-9 months or till a normal plasma cortisol level is reached and a normal adrenal response to exogenous ACTH is documented. [4]
Effects on Fetus and Breast -Fed Infants
Corticosteroids cross the placenta but there are no known significant teratogenic effects. It may cause growth retardation in the fetus. Corticosteroids taken in late pregnancy or lactation may cause adrenal suppression in the fetus and the neonates. However, corticosteroids may be used during pregnancy or lactation whenever indicated, e.g., herpes gestationis, but the newborn needs to be carefully monitored.
Immune Response
Corticosteroids inhibit the immune system and increase susceptibility to infections including those associated with live vaccines. Infection can spread rapidly, may have an atypical presentation and the severity may be masked. A regular dose of corticosteroids for 1-2 weeks can make the patient prone to infection. Prior to long-term steroid therapy, it is advisable to obtain a chest X-ray and tuberculin test to rule out tuberculosis in the child. If active tuberculosis is diagnosed on the basis of clinical features, chest X-ray and tuberculin test, steroid therapy can still be given along with antituberculosis therapy but the child needs close evaluation for tuberculosis. If only Mantoux is positive, then the child needs to be evaluated with his family for other evidence of tuberculosis and two-drug antituberculosis therapy may be given along with steroids. Varicella infection may cause fatal illness in patients taking long-term steroids and it is important to vaccinate susceptible children with the varicella vaccine. Infection prevention can be improved by hand washing, avoiding exposure to infectious diseases and use of appropriate vaccines.
Observations and Monitoring
On follow-up, each child should be clinically evaluated for vital parameters, peripheral perfusion, weight, height, waist measurements and assessment for infections. Investigations which may be needed include blood sugar, electrolytes and a complete hemogram. Ophthalmic evaluation and densitometry may be needed every 6-12 months.
Glucocorticoids, although potent and generally effective in many inflammatory and immunological conditions, are not without risks for producing serious side effects, especially when used in high doses for prolonged durations. The chance of significant side effects increases with the dose and duration of treatment and so only the minimum dose necessary to control the disease should be given. [8] Measures for prevention and early recognition of glucocorticoid-induced adverse effects are important for better patient outcome.
| 1. |
Mushtaq T, Ahmed SF. The impact of corticosteroids on growth and bone health. Arch Dis Child 2002;87:93-6.
[Google Scholar]
|
| 2. |
Silva IN, Kater CE, Cunha CF, Viana MB. Randomized controlled trial of growth effect of hydrocortisone in congenital adrenal hyperplasia. Arch Dis Child 1997;77:214-8.
[Google Scholar]
|
| 3. |
Boon LM, MacDonald DM, Mulliken JB. Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg 1999;104:1616-23.
[Google Scholar]
|
| 4. |
Disorders of Adrenal Glands. In: Behrman RE, Kliegman RM, Jenson HB, editors. Nelson Textbook of Pediatrics, 17th ed. Saunders: 1898 - 1913.
[Google Scholar]
|
| 5. |
Patel L, Clayton PE, Jenney ME, Ferguson JE, David TJ. Adult height in patients with childhood onset atopic dermatitis. Arch Dis Child 1997;76:505-8.
[Google Scholar]
|
| 6. |
Byron MA, Jackson J, Ansell BM. Effect of different corticosteroid regimens on hypothalamic-pituitary-adrenal axis and growth in juvenile chronic arthritis. J R Soc Med 1983;76:452-7.
[Google Scholar]
|
| 7. |
Lai HC, FitzSimmons SC, Allen DB, Kosorok MR, Rosenstein BJ, Campbell PW, et al. Risk of persistent growth impairment after alternate-day prednisone treatment in children with cystic fibrosis. N Engl J Med 2000;342:851-9.
[Google Scholar]
|
| 8. |
Wolthers OD, Pedersen S. Short-term growth in children with allergic rhinitis treated with oral antihistamine, depot and intranasal glucocorticosteroids. Acta Paediatr 1993;82:635-40.
[Google Scholar]
|
Fulltext Views
12,205
PDF downloads
3,230





