Translate this page into:
Mucosal and peri-orificial involvement in Post-Kala-Azar dermal leishmaniasis
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Sanjay K Rathi
143, Hill Cart Road, Siliguri - 734 401
India
| How to cite this article: Rathi SK, Pandhi R K, Khanna N, Chopra P. Mucosal and peri-orificial involvement in Post-Kala-Azar dermal leishmaniasis. Indian J Dermatol Venereol Leprol 2004;70:280-282 |
Abstract
BACKGROUND AND AIMS: Lesions of post-kala-azar dermal leishmaniasis (PKDL) usually affect the skin. Uncommonly, the involvement of oral and genital mucosae has been reported. METHODS: Twenty five patients clinically diagnosed as post-kala-azar dermal leishmaniasis were studied for periorificial and mucosal lesions. Clinical examination, skin smears and biopsy were done for the patients with periorificial or mucosal lesions. RESULTS: Out of 25 patients of PKDL, seven patients had lesions on the oral and/or genital mucosa. Three cases had oral lesions; two had only genital lesions and three patients had both sites involved. All the patients were having skin lesions elsewhere too either as nodules and/or plaque or macules. Conclusion: While examining a case of PKDL, mucosal involvement must also be examined carefully.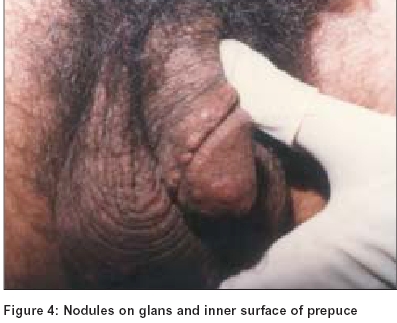 |
 |
 |
 |
 |
 |
 |
 |
INTRODUCTION
Post-kala-azar dermal leishmaniasis (PKDL), usually occurring 6 months to 5 years, after an attack of visceral leishmaniasis is caused by Leishmania donovani.[1] It was first described in 1922 as a distinct clinical entity.[2] Three main types of skin lesions have been described in PKDL. They are: i) hypopigmented macules ii) butterfly erythema of the face and iii) nodular lesions.[3],[4] Mucosal involvement, one of the rare types, has been described by a few workers.[4],[5],[6] We studied the mucosal and periorificial lesions in PKDL.
METHODS
Twenty-five patients clinically suggestive of PKDL were included for this study. The diagnosis was made clinically. Tissue smear for Leishmania donovani bodies (LDBs) and histopathological examination were done in an attempt to establish the diagnosis. Slit-skin smear for acid fast bacilli was done to rule out leprosy.
The patients were examined for various clinical lesions and for better understanding they were divided into 3 groups:
Group A: skin lesions with oral involvement
Group B: skin lesions with genital involvement
Group C: skin lesions with both oral and genital involvement
RESULTS
Out of the 25 patients, 22 were males and three were females. Their age ranged from 6 years to 55 years. Seven patients, all male, had mucosal lesions in the present study. They all demonstrated LDBs in their tissue smears. Two main types of lesions were seen; infiltrated nodules and/or plaques and hypopigmented macules. Eighteen cases presented with both types of lesions, while two cases had only macules and five presented with only nodules and/or plaque lesions.
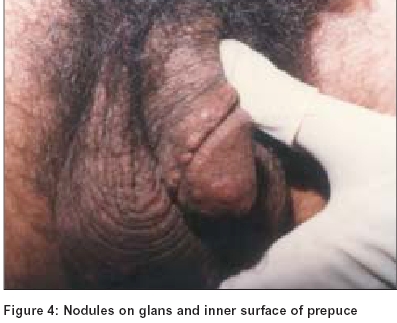
Group A: Three patients presented with only oral mucosa involvement along with skin lesions. The tongue, lips [Figure - 1], and the hard palate were the sites affected. Two of them had lesions on the tongue and lips; the third case also showed a lesion on the hard palate [Figure - 2]. They all had infiltrated nodules.
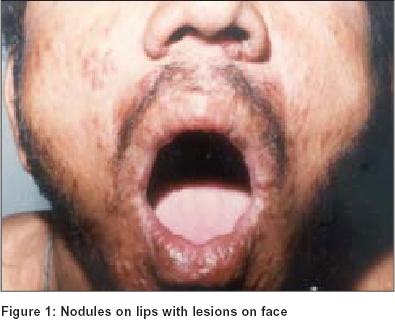
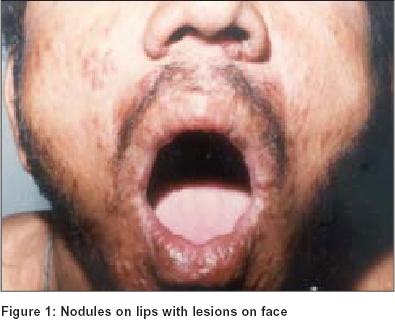
Group B: Two cases had genital lesions only, without the involvement of oral mucosa. The sites commonly affected were the shaft of the penis [Figure - 3], and the inner surface of prepuce and glans [Figure - 4]. Erythematous plaques were observed in the shaft of the penis, while at other sites, nodules were the predominant lesions.
Group C: In two PKDL patients, both the genital and oral mucosae were involved. The lesions were distributed on the penile shaft, glans penis, lips and tongue.
DISCUSSION
Various rare morphological forms of PKDL have been documented from regions endemic for PKDL.[7],[8],[9],[10] They include mucosal, xanthomatous, verrucous, papillomatous, hypertrophic, fibroid, atrophic, extensive hypopigmentation, etc. Amongst the mucosae, lesions of PKDL usually affect the oral mucosa which shows granulomatous nodules at the angles of mouth, over the dorsum of the tongue, buccal mucosa or the soft palate.[4],[5],[6],[11] Nodules on the tongue were observed by Panja[12] and Ghosh Dastidar.[13] Ramesh, et al[6] in their 18 cases of PKDL found mucosal lesions in five patients, on the lips, tongue and palate. The inner surface of the prepuce and the glans were also involved.[6]
In our observation mucosal lesions were noted in seven (28%) patients; the lips, tongue, hard palate, inner surface of prepuce, glans and the shaft of penis were affected. All the mucosal lesions subsided after anti-leishmanial treatment.
To the best of our knowledge there is no separate study on the mucosal involvement in PKDL in the literature. The mucosa must also be looked for while examining a patient of PKDL.
| 1. |
Das Gupta BM. A note on the parasite of dermal leishmanoid. Indian Med Gaz 1927;62:11-2.
[Google Scholar]
|
| 2. |
Brahmachari UN. A new form of cutaneous leishmaniasis-dermal leishmanoid. Indian Med Gaz 1922;57:125-7.
[Google Scholar]
|
| 3. |
Napier LE, Das Gupta CR. A clinical study of post-kala-azar dermal leishmaniasis. Indian Med Gaz 1930;65:249-57.
[Google Scholar]
|
| 4. |
Munro DD, Du Vivier A, Jopling WH. Post-kala-azar dermal leishmaniasis. Br J Dermatol 1972;87:374-8.
[Google Scholar]
|
| 5. |
Singh RP. Observations on dermal leishmanoid in Bihar. Indian J Dermatol 1968;13:59-63.
[Google Scholar]
|
| 6. |
Ramesh V, Misra RS, Saxena U, Mukherjee A. Post-kala-azar dermal leishmaniasis: A clinical and therapeutic study. Int J Dermatol 1993;32:272-5.
[Google Scholar]
|
| 7. |
Anonymous. Control of the leishmaniasis. Report of a WHO Expert Committee, Tech Rep Ser, WHO, Geneva, No. 793, 1990.
[Google Scholar]
|
| 8. |
Ramesh V, Mukherjee A. Post-kala-azar dermal leishmaniasis. Int J Dermatol 1995;34:85-91.
[Google Scholar]
|
| 9. |
Rathi S, Khanna N, Pandhi RK. Post-kala-azar dermal leishmaniasis with atypical presentation. Indian J Dermatol Venereol Leprol 1995;61:323.
[Google Scholar]
|
| 10. |
Rathi S. Post-kala-azar dermal leishmaniasis with an atypical presentation. J Dermatol 2001;28:341-2.
[Google Scholar]
|
| 11. |
Dey NC, Kuar BK. Dermal leishmanoid in Assam. J Indian Med Assoc 1953;22:456-61.
[Google Scholar]
|
| 12. |
Panja G. An unusual case of dermal leishmaniasis of the tongue. J Indian Med Assoc 1938;7:368-9.
[Google Scholar]
|
| 13. |
Ghosh Dastidar SK. A rare tumour of tongue. A manifestation of post-kala-azar dermal leishmaniasis. Br Med J 1939;2:14-5.
[Google Scholar]
|
Fulltext Views
2,259
PDF downloads
1,239





