Translate this page into:
Multifocal dermatofibrosarcoma protuberans
Correspondence Address:
Kirti S Deo
G 11, Gokhale Vrindavan, Near Chapekar Chowk, Chinchwad, Pune 411 033, Maharashtra
India
| How to cite this article: Deo KS, Sharma YK, Virmani NC, Dash KN, Chaudhari ND. Multifocal dermatofibrosarcoma protuberans. Indian J Dermatol Venereol Leprol 2012;78:385-387 |
Sir,
Dermatofibrosarcoma protuberans (DFSP) is a relatively uncommon soft tissue neoplasm with low to intermediate grade malignancy. [1],[2] It is a clinically distinctive, raised/atrophic or sclerotic cutaneous fibrous tumor that exhibits a pattern of slow, infiltrative growth. It has a marked tendency to recur locally after surgical excision [3] with rare cases metastasizing to regional lymph nodes or distant sites. [2] It constitutes less than 0.1% of all cutaneous malignancies and 1% of all soft tissue sarcomas. [3] Most lesions occur over the trunk or proximal extremities and are focal in nature. [1],[2],[3] Early diagnosis, wide excision and regular follow up are essential components of management of DFSP. Herein we report a case of multifocal DFSP.
A 59-year-old male presented with history of having concurrently developed 6 years back two asymptomatic swellings; a protuberant mass over left lumbar region and an ulcerated one on right mandible. The abdominal swelling, stated to be pea-sized at the onset, progressed gradually over the initial 5 years and relatively rapidly over the month preceding his presentation to us. Likewise the facial swelling too progressed from a millet-sized papule to a palm-sized plaque and ulcerated in the preceding month following the application of a caustic agent. Examination of the abdominal wall revealed a firm 5 × 5 cm, yellow to brown plaque with a central protuberance surmounted by an ulceration. The surrounding skin appeared retracted, shrivelled and hyperpigmented [Figure - 1]a. The second-firm, erythematous, blanchable centrally encrusted 5 × 3-cm-sized plaque- seen over the right mandibular region [Figure - 1]b was biopsied and revealed a pattern of uniform "storiform" spindle cells with elongated nuclei showing little pleomorphism and scanty pale cytoplasm with little mitotic activity in the dermis [Figure - 2] consistent with DFSP. CT scan of the chest appeared normal. Both the masses were subjected to wide local excisions and their histopathology evaluation was diagnostic of DFSP. Immunohistochemical staining being positive for CD34 [Figure - 3], was corroborative.
DFSP is a relatively uncommon spindle cell sarcoma of fibroblastic/myofibroblastic differentiation. [1],[2],[3] Although first described by Taylor in 1890, it was Hoffman who coined the current nomenclature when he reported three cases in 1925. [4] Other terms used to describe the neoplasm are: Progressive and recurrent dermatofibroma (Darier and Ferrand), hypertrophic morphea (Sherwell), sarcomatous tumors resembling keloid (Taylor), fibrosarcoma of the skin (Stout). [4] Chromosomes 17 and 22 have been incriminated in its pathogenesis with translocation t (17:22) involving COL1A1 (collagen type 1α 1 gene) and platelet-derived growth factor β (PDGF β) genes. [3] DFSP is commoner in men than in women with a peak incidence during the third decade. [2],[4] Local recurrences occur in 20-55% of cases. The trunk is the most common anatomical site affected (42-72%) followed by proximal extremities (16-30%) and head and neck (10-16%). It may occur at sites of previous trauma. [1]
 |
| Figure 1: (a) Protuberant mass with central ulceration over left side of abdominal wall. (b) Erythematous, ulcerated plaque over right mandibular region |
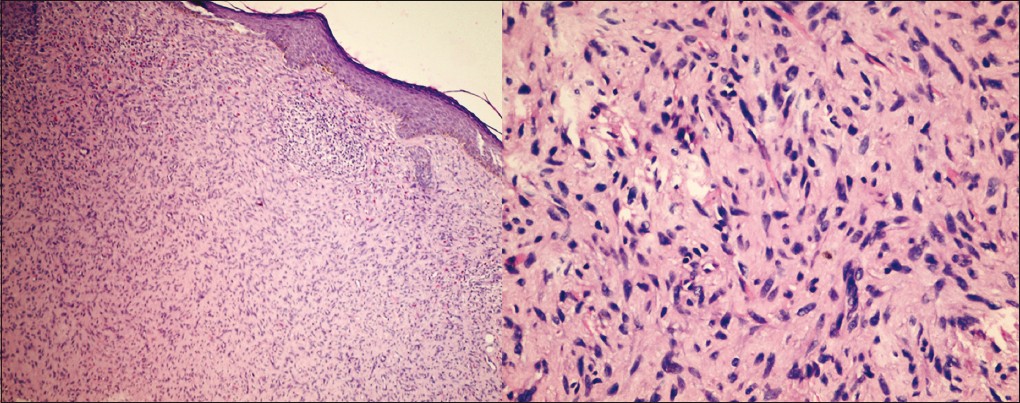 |
| Figure 2: Histopathological view showing a pattern of uniform storiform spindle cells in the dermis (H and E, ×100 and ×400) |
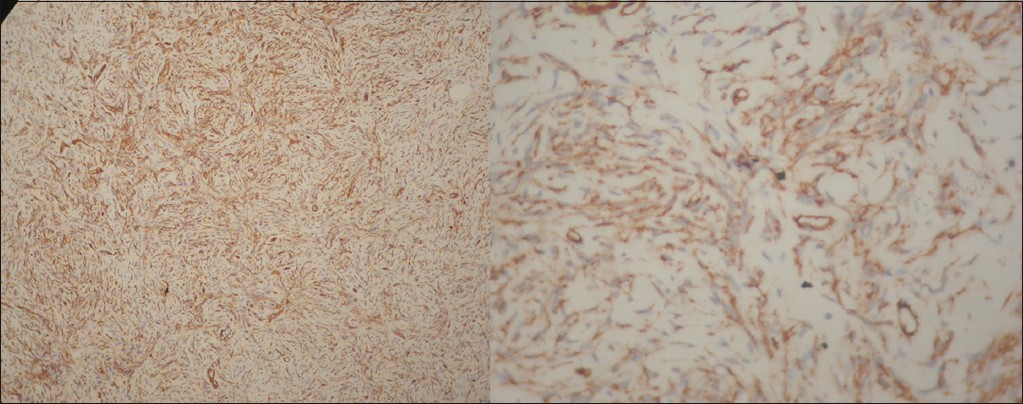 |
| Figure 3: Tumor cells strongly positive for CD34 (Immunohistochemical stain, ×100 and ×400) |
Most of these tumors are focal in origin. However, the simultaneous occurrence of the two masses over face and abdomen in our case probably represents multifocal origin rather than cutaneous metastases. To the best of our knowledge cases of DFSP having multifocal origin as was our case, have rarely been documented in the literature. [4],[5]
The tumor first appears as a single, red to bluish, blanchable, firm, cutaneous nodule. Its surface enlarges by expansile growth while the periphery of the tumor invades the adjacent skin and subcutaneous tissue. During the late stage, rate of growth accelerates, producing the characteristic protrusion from the skin. The overlying skin is stretched and undergoes, atrophic changes which lead to heightened susceptibility to trauma resulting in superficial ulceration and bleeding. The growth rate is usually variable. [4] Lesions may remain stable for many years or grow slowly with occasional periods of accelerated growth. [4],[5] Histologically DFSP is characterised by irregular, interwoven dermal fibrocellular fascicles composed of uniform spindle-shaped cells having a storiform appearance. [1],[3],[4],[5] Immunohistochemically these tumors stain positively for CD34 and mostly negative for factor XIIIa. Apolipoprotein D, a 33-kD glycoprotein component of high-density lipoprotein, has recently been proposed as a novel marker for DFSP. [3]
Wide surgical excision with a safety margin of 3 cm including the underlying fascia remains the mainstay of treatment. Mohs micrographic surgery having the advantages of high oncologic effectiveness and maximal tissue conservation, is increasingly being accepted as the treatment of choice. [1],[2],[3] Radiation therapy and imatinib are alternative treatments for unresectable tumors or additional adjuncts. [1]
To conclude, this histopathologically proven case of DFSP is being reported for its rare occurrence with multicentric origin. To the best of our knowledge only two such cases with multicentric origin of DFSP have earlier been reported in the literature. [4],[5]
| 1. |
Kim GK. Status report on the management of dermatofibrosarcoma protuberans: Is there a viable role for the use of imatinib mesylate? In which cases may it be therapeutically helpful and in which cases not? J Clin Aesthet Dermatol 2011;4:17-26.
[Google Scholar]
|
| 2. |
Asuquo ME, Umoh MS, Ebughe G. Dermatofibrosarcoma protuberance: Case reports. Ann Afr Med 2007;6:80-3.
[Google Scholar]
|
| 3. |
McArthur G. Dermatofibrosarcoma protuberans: Recent clinical progress. Ann Surg Oncol 2007;14:2876-86.
[Google Scholar]
|
| 4. |
McPeak CJ, Cruz T, Nicastri AD. Dermatofibrosarcoma protuberans: An analysis of 86 cases-five with metastasis. Ann Surg 1967;166:803-16.
[Google Scholar]
|
| 5. |
Taylor HB, Helwig EB. Dermatofibrosarcoma protuberans. A study of 115 cases. Cancer 1962;15:717-25.
[Google Scholar]
|
Fulltext Views
2,729
PDF downloads
1,884





