Translate this page into:
Multiple eruptive milia over both external ears
Correspondence Address:
Reena Sharma
C-304, Shri Sai Baba apartment, Sector 9, Rohini, Delhi 110 085
India
| How to cite this article: Sharma R, Singal A, Sonthalia S. Multiple eruptive milia over both external ears. Indian J Dermatol Venereol Leprol 2011;77:519-520 |
Sir,
A 13-year-old Indian girl presented with history of sudden eruption of asymptomatic white papules on both the external ears within a period of 1 month. She had no history of preceding trauma, insect bite, ear discharge, eczema, vesicular lesions, photosensitivity, or drug intake (oral or topical). There was no history of similar complaints in siblings or any other family members. Examination revealed multiple superficial, firm, discrete, white, dome shaped papules of size 1-3 mm present on both the external ears and a few scattered lesions over the pre auricular and postauricular areas, without any background scarring [Figure - 1]. Histopathology revealed a cyst within the superficial dermis lined by stratified squamous epithelium with a granular layer containing eosinophilic concentric lamellae of keratin, diagnostic of milium [Figure - 2]. There was no evidence of vellus hair cell in the cyst cavity.
 |
| Figure 1: Multiple milia present over both external ears |
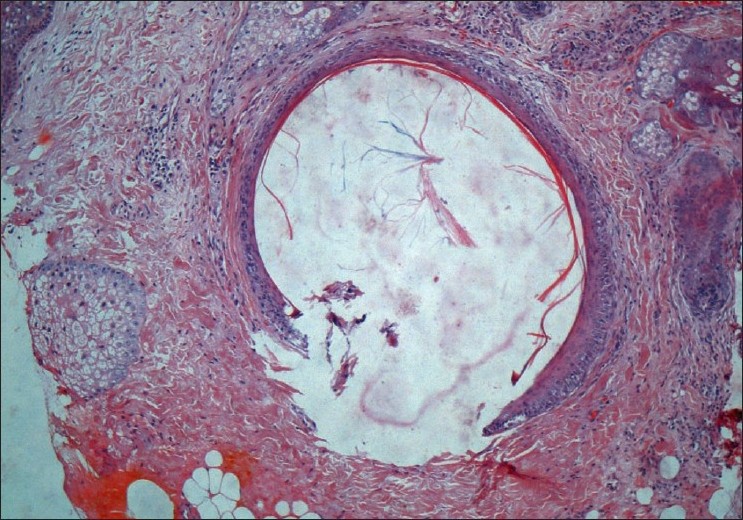 |
| Figure 2: Subepidermal cyst lined by stratified squamous epithelium containing eosinophilic concentric lamellae of keratin, suggestive of milium (H and E, ×100) |
Milia are common benign keratinous cysts that occur most commonly on the face, particularly over eyelids and the cheeks. [1] Milia may be primary or secondary. Primary milia arise spontaneously and may be present at birth. They occur as single or multiple, randomly arranged papules distributed over the face in adults; with occasional involvement of upper trunk and arms commonly seen in newborns. [1] Secondary milia arise as a cutaneous reaction to traumatic stimuli or pathologically altered integument and are localized to the involved body site, e.g., following dermabrasion, radiotherapy, second degree burns, autologous skin transplantation, allergic contact dermatitis, prolonged use of topical steroids, topical 5-flurouracil, anti-inflammatory drugs and acitretin therapy. [1] In addition, they have been reported after the clearance of bullous disorders, or in association with certain genodermatoses. Eruptive milia appear briskly, usually within 1 month, and are most frequently distributed on the head, neck, and trunk. The lesions are usually asymptomatic. Langley et al.[1] have proposed a classification to encompass the reported cases of multiple eruptive milia. [1] According to this classification, eruptive milia could either present spontaneously without a known cause, as part of an autosomal dominant familial condition, or as part of a genodermatoses, such as Rombo syndrome, basaloid follicular hamartoma syndrome, or Gardner syndrome. [1],[2] Milia may develop from the proliferation of pluripotent cells located in any epithelial structure. [3] In addition, subsequent retention of keratin debris plays a role in the formation of secondary milia. [3] The exact cause of formation of primary milia and multiple eruptive milia is unknown. On the face, both primary and multiple eruptive milia most commonly derive from the external root sheath of vellus hair follicles, [3] whereas in other locations secondary milia more often derive from eccrine ducts. [4] Milia should not be confused with eruptive vellus hair cyst which presents as multiple flesh colored, follicular papules ranging in size from 1 to 5 mm. Histopathology reveals a cystic structure usually seen in the mid-dermis lined by squamous epithelium. It contains laminated keratinous material and varying numbers of transversely and obliquely cut vellus hairs. [5] In contrast, histopathology of a milium reveals a cyst in superficial to mid dermis lined by stratified epithelium with granular layer, containing laminated keratin and no vellus hair in the cavity. [3]
To the best of our knowledge, till date ten cases of multiple eruptive milia have been described with only one case report of eruptive milia on the external ears from Korea. [6] None is reported from India. Our patient is the first case of spontaneous eruptive milia present over the external ear from India as no other underlying cause was elicited. Many modalities have been used to treat milia including excision, curettage, electrodessication, topical tretinoin, epilating needle, Er:YAG laser, and oral minocycline. [1]
| 1. |
Langley RG, Walsh NM, Ross JB. Multiple eruptive milia: Report of a case, review of the literature, and a classification. J Am Acad Dermatol 1997;37:353-6.
[Google Scholar]
|
| 2. |
Diba VC, Handfield-Jones S, Rytina E, Hall P, Burrows N. Multiple eruptive milia in a 9-year-old boy. Pediatr Dermatol 2008;25:474-6.
[Google Scholar]
|
| 3. |
Epstein W, Kligman AM. The pathogenesis of milia and benign tumors of the skin. J Invest Dermatol 1956;26:1-11.
[Google Scholar]
|
| 4. |
Tsuji T, Sugai T, Suzuki S. The mode of growth of eccrine duct milia. J Invest Dermatol 1975;65:388-93.
[Google Scholar]
|
| 5. |
Esterly NB, Fretzin DF, Pinkus H. Eruptive vellus hair cysts. Arch Dermatol 1977;113:500-3.
[Google Scholar]
|
| 6. |
Kim JY, Park SJ, Yi JA, Lee WJ. A case of multiple eruptive milia occurring on both external ears. Korean J Dermatol 2004;42:1212-4.
[Google Scholar]
|
Fulltext Views
6,646
PDF downloads
2,184





