Translate this page into:
Multiple pigmented nodulo-ulcerative lesions in a middle-aged man
Corresponding author: Dr. Neetu Bhari, Department of Dermatology & Venereology, All India Institute of Medical Sciences, New Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Choudhary R, Imran S, Sahni K, Surya V, Arava S, Bhari N. Multiple pigmented nodulo-ulcerative lesions in a middle-aged man. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1524_2024
A 69-year-old man presented with gradually progressive, asymptomatic, nodulo-ulcerative lesions over the face [Figure 1a], chest, and retro-auricular areas [Figure 1b] for the last 15-years. He did not have any systemic complaints. His medical and family history were unremarkable. He was a goldsmith by profession for the past 40 years and did not report the occurrence of similar lesions in his co-workers. On mucocutaneous examination, discrete to confluent, skin-coloured, translucent nodules of size 1-2 cm were seen over his bilateral infra-orbital areas, many of which were pigmented and showed a beaded border. Similar but larger pigmented ulcerated plaques (1-3 cm in size) were also noted over his forehead, supraorbital and retroauricular areas, dorsum of the nose, upper lip, and chest. Examination of palms revealed a few pits. Histopathologic findings of skin biopsy from lesions over the face are shown in Figure 2. His orthopantomogram showed multiple well-defined round-to-oval radiolucent lesions [Figure 3].

- Multiple pigmented nodulo-ulcerated lesions over the face. a) Multiple pigmented nodulo-ulcerated lesions over face, b) Pigmented ulcerated plaque over retroauricular area.
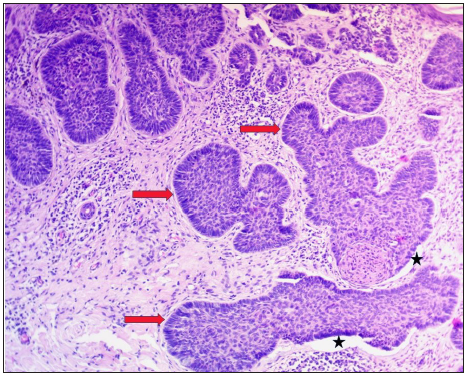
- Multiple nests of basaloid cells with peripheral palisading (marked with red arrow) and retraction artifacts between nest and stroma (marked with black asterisk) (Haematoxylin & eosin, 100x)
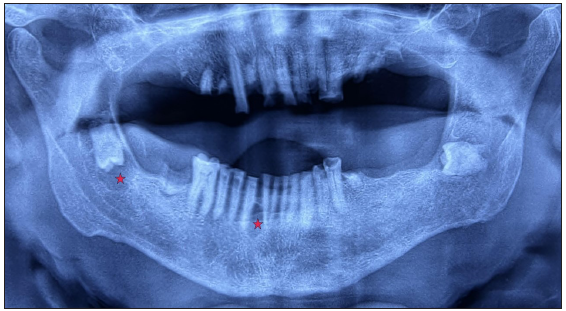
- Orthopantomogram showing multiple well-defined radiolucencies in the jaw (marked with a red asterisk).
Question
What is your diagnosis?
Answer
Diagnosis: Naevoid basal cell carcinoma syndrome (NBCCS)
Discussion
Histopathology showed nests of basaloid cells with peripheral palisading and retraction artifacts, suggestive of nodular basal cell carcinoma (BCC) [Figure 2]. Histopathology of cystic lesions from retromolar trigone showed an inflamed cyst capsule lined by non-keratinised stratified squamous epithelium, suggestive of inflamed dentigerous cysts. A skeletal survey for other bony abnormalities was non-contributory. For molecular diagnosis, whole exome sequencing was performed using DNA isolated from the patient’s blood. Sequencing results revealed a novel heterozygous mutation in exon 18 of the PTCH1 gene (NM_000264:c.T3107A:p.L1036X), which resulted in the incorporation of a stop codon at position 1036. This stop-gain mutation results in the truncation of proteins and is hence classified as pathogenic according to American College of Medical Genetics and Genomics (ACMG) guidelines. The functional effect of the variant scored by MutationTaster and Sorting Intolerant from Tolerant (SIFT) score revealed that this variant is highly deleterious. Most BCCs were excised completely by Mohs micrographic surgery and the patient was advised for photoprotection and regular follow-up.
NBCCS, also known as Gorlin-Goltz syndrome, occurs due to a mutation in the PTCH gene.1 It is transmitted in an autosomal dominant pattern with high penetrance and variable expressivity. Around 60% of patients do not have any affected family members.1 PTCH gene is associated with the Hedgehog signaling pathway, and loss of heterozygosity leads to the formation of various hamartomas such as BCCs, odontogenic keratocysts, meningiomas, and ovarian fibromas.2 Diagnostic criteria for NBCCS have been developed by Kimonis et al. [Table 1], and diagnosis requires two major criteria or one major with two minor criteria.3
| Major criterion | Minor criteria |
|---|---|
| 1. Multiple (>2) BCCs or one under 20 years | 1. Macrocephaly: determined after adjustment for height |
| 2. Odontogenic keratocyst of the jaws proven by histopathology | 2. Congenital malformation: cleft lip or palate, frontal bossing, “coarse face”, moderate or severe hypertelorism |
| 3. Palmar or plantar pits (3 or more) | 3. Other skeletal abnormalities: sprengel deformity, marked pectus deformity, marked syndactyly of the digits |
| 4. Bilamellar calcification of the falx cerebri]’ | 4. Radiological abnormalities: bridging of the sella turcica, vertebral anomalies such as hemivertebrae, fusion or elongation of the vertebral bodies, modeling defects of the hands and feet, or flame-shaped lucencies of the hands or feet |
| 5. Bifid, fused, or markedly splayed ribs | 5. Ovarian fibroma |
| 6. First-degree relatives with Naevoid basal cell carcinoma | 6. Medulloblastoma |
Our patient had multiple BCC and three palmar pits, fulfilling the clinical criterion of NBCCS, which was later confirmed by whole exome sequencing. International colloquium on NBCCS recommended that molecular confirmation can be substituted by one of the major criteria, such as the addition of medulloblastoma to the major criteria and the addition of numerous ocular abnormalities (such as strabismus, nystagmus, congenital cataracts, glaucoma, etc.) to the minor criteria.4 BCCs are one of the earliest noticed lesions in this syndrome, and incidence ranges from 40% in African-Americans to 90% in whites.2 In contrast to most other reported cases, our patient developed BCC at a later age. This difference could be due to our patient’s darker skin phototype in contrast to the white population. Dental lesions most often reported in NBCCS are odontogenic keratocysts (in about 65% of patients)4 and usually present in the first to second decade of life. However, there are few case reports also of dentigerous cysts in these patients, like ours.5 Screening for other associated tumours is recommended in all suspected and confirmed cases of NBCCS.
First-line treatment of NBCCs includes wide local excision, regular follow-up, and photoprotection. Mohs micrographic surgery is helpful in conserving normal tissues in lesions located near important structures such as the eyes. In patients with unresectable tumours, Vismodegib, a hedgehog inhibitor, is recommended, although it is not yet available in our country.
Thus, inspite of its rare occurrence, the correct diagnosis of NBCCS helps in screening for associated anomalies and proper counselling of the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Nevoid basal cell carcinoma syndrome: A case report and review. J Maxillofac Oral Surg. 2015;14:11-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nevoid basal cell carcinoma (Gorlin) syndrome. Genet Med. 2004;6:530-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet.. 1997;69:299-308.
- [CrossRef] [PubMed] [Google Scholar]
- Nevoid basal cell carcinoma syndrome: A case report and literature review. Ophthalmic Genet. 2022;43:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple dentigerous cysts in a patient showing features of gorlin-Goltz syndrome: A case report. Int J Surg Case Rep. 2024;114:109156.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





