Translate this page into:
Nail dyschromias
Correspondence Address:
Vibhu Mendiratta
Department of Dermatology, Venereology and Leprosy, Lady Hardinge Medical College, Connaught Place, New Delhi - 110 001
India
| How to cite this article: Mendiratta V, Jain A. Nail dyschromias. Indian J Dermatol Venereol Leprol 2011;77:652-658 |
Abstract
Nail dyschromias have a wide variety of presentation. There are numerous causes of discoloration of the nail affecting the nail plate, nail attachments, or the substance of the nail. The chromonychia may also be caused due to the exogenous deposition of pigments over the nail plate. Careful examination of the nail and few bed side tests may help in identifying the root cause of the nail dyschromia and many a times unravels some underlying systemic disorder too.Introduction
Nail dyschromia or chromonychia is defined as an abnormality in the color of the substance or the surface of the nail plate or subungual tissue. [1] The discoloration specifically due to the deposition of melanin is labeled as nail pigmentation. [2]
Discoloration of the otherwise transparent nail may be due to a large number of factors affecting the nail plate, nail attachments, or the underlying substance. [3] The pigments responsible for nail color alteration may be deposited either exogenously (occupational exposure, henna) or may be a result of over production or storage of some endogenously derived pigments. There are innumerable causes of nail dyschromias, but a fair idea about its anatomical origin and involvement of the concerned part of the nail apparatus can be made by a good history taking and examination of the nail. Nails should always be examined under natural light with the hands in relaxed position. A slight pressure over the tip of the nail plate usually blanches the discoloration which is a result of altered vasculature of the nail bed, whereas if the abnormality is in the nail plate, the discoloration persists as such. Transillumination using a pen torch placed against the pulp of the finger helps in pointing out the abnormalities in the nail plate especially markings on the plate, pitting, subungual thickness, onycolysis, to name a few. These are readily differentiated from the diffuse homogenous reddish glow of the normal nail plate. [4]
When the dyschromia is due to the external agents, the discoloration follows the shape of the proximal nail fold whereas if the cause is internal, the discoloration corresponds to the shape of the lunula. Successful use of acetone to remove nail discoloration points towards an application of topical agent. Sometimes a potassium hydroxide mount of the cut sample or special stain of the biopsy sample is needed to reach the exact cause of nail dyschromia.
All the nails, including finger and toe nails, should be always examined in totality apart from the affected nail. It should be kept in mind that any systemic disorder will affect many or all the nails simultaneously, whereas a localized factor like infection or localized tumor causes nail changes in a single or limited number of nails. In addition, a quick but thorough cutaneous and mucosal examination is desired as these may many a times provide an important clue to an underlying disease. Few morphological changes might occur otherwise in an apparently normal healthy individual. An idea of this may help avert unnecessary work up in these individuals.
The common patterns of abnormal nail coloration or dyschromia includes:
- White chromonychia - leukonychia
- Black chromonychia - melanonychia
- Yellow chromonychia
- Blue chromonychia
- Red chromonychia
- Dyschromia due to exogenous causes.
White chromonychia (Leukonychia)
Opaque white discoloration of nail or leukonychia is the most common form of nail dyschromia. Leukonychia has been classified into three different types: true leukonychia, apparent leukonychia, and pseudoleukonychia.
True leukonychia
A defect in nail matrix giving rise to white discoloration of nail plate is called true leukonychia. It arises due to disorganization of the keratin fibrils and diffraction of light, hence the white opaque appearance. [1] True leukonychia is further divided into subtypes depending on the extent and pattern of involvement.
-
Total or complete leukonychia is a rare form of true leukonychia where the whole nail appears opaque, milky, chalky, or porcelain white [Figure - 1]. It can either be congenital or acquired, the latter form being much more common.
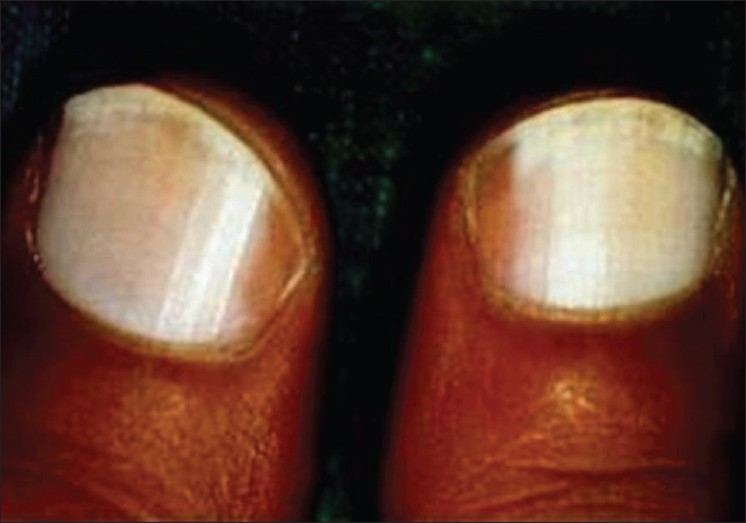
Figure 1: Total leukonychia - Subtotal or incomplete leukonychia represents involvement of only some part of the nail. Some believe it to be the initial stage of total leukonychia. [5]
- Punctate leukonychia presents as small white spots, occurring singularly or in groups, in few or all nails, finger nail being more commonly involved. This occurs commonly due to microtrauma to the nail matrix. The white spots may either start near lunulae or sometimes distally. It grows distally with the nail and many a times disappear in their course.
- Transverse leukonychia presents as small white transverse band on one or many nails, most commonly due to repeated micro trauma to un-cut nails, small shoe size or frequent manicures. Development of transverse leukonychia has also been reported after the use of cytotoxic agents, steroids and retinoids. [1] Mee′s line due to acute arsenic poisoning or thallium poisoning represents a form of transverse leukonychia. Leukonychia variegata is a variant of transverse leukonychia where the nails present with irregular white transverse thread like streaks. [1]
- Longitudinal leukonychia presents as a permanent longitudinal white band on the nail plate. Though usually considered a disorder of nail matrix keratin organization, few authors consider it to be due to parakeratotic hyperplasia of the nail bed epidermis, with normal kertainization of the nail. [6]
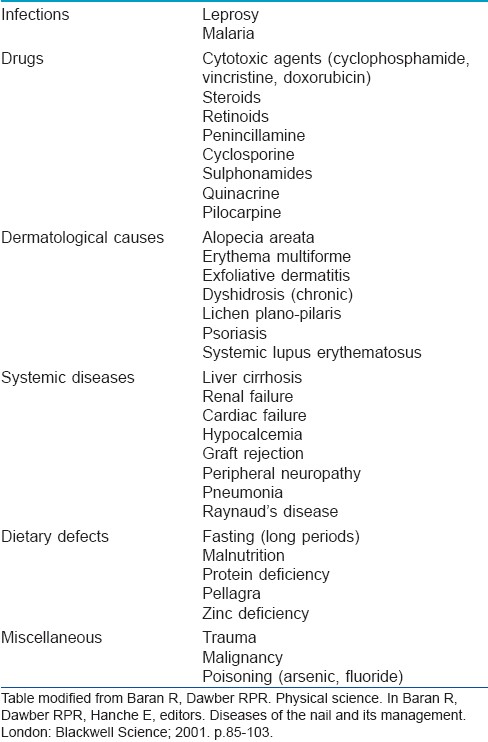
The complete and incomplete forms of true leukonychia more commonly denotes a systemic disorder [Table - 1], whereas the transverse and punctate forms are more commonly due to localized trauma. [1],[7],[8],[9]
Apparent leukonychia
The white appearance of the nail plate may at times be due to the changes in the nail bed vasculature or substance which alters the translucency of the nail plate. Apparent leukonychia is also known as leukopathia. [1]
- Half and half nail is also known as Lindsay nail. In this the proximal part of the nail is dull white and opaque, obscuring the lunula. The distal 20%-60% area of the nail is normal pink in appearance. There is a sharp demarcation between both these bands. This is most commonly seen in chronic renal failure, especially those with uremia, though the levels of urea are not the deciding factor. [10] Chemotherapy, zinc deficiency, liver cirrhosis, Kawasaki disease and recently described reports with Crohn′s disease are the other causes of half and half nails. [11],[12]
-
Terry′s nail: This is seen commonly in patients with cirrhosis where a large part of the nail is opaque white, obscuring the lunula, leaving only a thin band of pink -brown distal nail [Figure - 2]. This can also be present in patients with congestive heart failure, diabetes mellitus and old age.

Figure 2: Terry's nail - Muehrcke′s nail: The nails show paired white opaque bands, parallel to the lunula separated from each other by narrow strips of pink nail in between. Seen characteristically in patients with low albumin, it disappears when the albumin levels are normalized. Being a nail bed disorder, it vanishes on application of pressure to the nail plate. Other causes of paired white Muehrcke′s band are chemotherapy, heart transplant, and trauma. [13]
- Anemia can produce pallor and thereby apparent leukonychia. [1]
Pseudoleukonychia
Pseudoleukonychia is the term used to describe the white discoloration of the nail where neither the matrix nor the nail bed is the culprit, e.g. white discoloration of the nail due to onychomycosis or keratin deposits due to nail varnish.
Black chromonychia (Melanonychia)
Melanonychia is the black-brown discoloration of the nail due to the deposition of melanin [Figure - 3]. Melanin in the nail plate most commonly has the appearance of longitudinal pigmented band, known as longitudinal melanonychia. This term is reserved for the band appearing in the matrix region and extending to the tip of the finger. [2] Total or transverse melanonychia have a much rarer presentation.
 |
| Figure 3: Drug induced melanonychia involving all finger nails |
Melanonychia develops either due to the melanocyte activation or melanocyte hyperplasia. The various causes of melanonychia are mentioned in [Table - 2]. The black pigmented striations on the nail are a common finding among skin types V and VI affecting nearly 15-20% Asians and as high as 70% African-Americans above the age of 20 seen more frequently in the digits used for grasping or in those prone to trauma. [2]
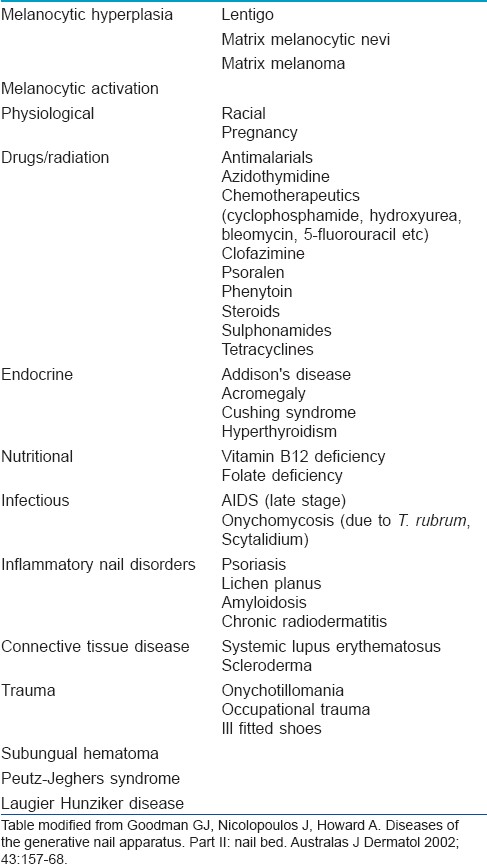
A presentation with longitudinal melanonychia should raise an alarm in the direction of subungual melanoma. A proper history and complete cutaneous examination is essential in cases of melanonychia to differentiate subungual melanoma from many other commoner benign cause of melanonychia. Hutchinsons′ sign, an indicator of subungual melanoma, is defined by the presence of periungual extension of pigmentation from nail bed and matrix to the proximal and lateral nail folds and cuticle. Pseudo Hutchinson′s sign may arise in three types of settings. Firstly, periungual pigmentation may be present in benign conditions like racial predisposition, malnutrition, congenital nevus, Peutz-Jeghers syndrome etc. Secondly non melanoma tumor like Bowen′s disease may present with periungual pigmentation. Lastly, at times pigments in matrix and nail bed are visible through the translucent and uninvolved cuticle, creating Pseudo-Hutchinson sign.
Dermatoscopy can be helpful in differentiating melanocytic from non melanocytic causes of melanonychia. The pigmentation in non melanocytic origin will always appear homogenous whereas those with melanocytic origin will show pigmentation in cellular inclusions as small granules. [14] When in any suspicion, a nail matrix biopsy is advisable to rule out melanoma as a cause of melanonychia.
Yellow chromonychia
Yellow discoloration of the nail could be a normal finding in elderly or develop secondary to jaundice, carotenemia, ochronosis or systemic drugs like hydroxyurea (yellow-brown discoloration), tetracycline, penicillamine, antimalarials, gold. [15] [Figure - 4] Few dermatological conditions which may give rise to yellow discoloration of nails include onychomycosis, psoriasis, and alopecia areata.
 |
| Figure 4: Yellow discoloration of nails due to exogenous pigment deposition |
Yellow nail syndrome (YNS) is a rare condition of uncertain aetiology characterized by slow growing nail, yellow-green discoloration obscuring the lunula, and increased lateral curvature. Other characteristic nail findings in YNS include absence of cuticle, thickened nail plate and subungual hyperkeratosis, increased incidence of paronychia, and eventual nail loss. Yellow nail with few of these nail changes are a must to qualify as YNS. Patients present with dirty yellow nail with difficulty in fine object manipulation. The yellow discoloration is due to the deposition of lipofuscin. [16] Few authors suggest a clinical triad of yellow nail, lymphedema and pleural effusion, with at least two of these to be present, as a prerequisite to label as YNS, [17] whereas few others disagree. [18] Many other cardio pulmonary abnormalities have also been found to be associated with YNS. These include bronchiectasis, chronic bronchitis, cystic lung disease, rhinitis, sinunitis, pericardial effusion, and chylous ascites. Impaired lymphatic flow is considered the pathogenic factor responsible for both pulmonary and nail abnormalities. [19] Few suggest that YNS is related to protein leakage from increased micro vascular permeability which also accounts for its association with hypoalbuminemia. Other reported associations of YNS include rheumatoid arthritis, immunodeficiency states including AIDS, mycosis fungoides, carcinoma breast and gall bladder, nephrotic syndrome, and thyroid disease. [15]
Spontaneous recovery in nail changes have been reported to vary between 5% to 30% in various studies, though this is often incomplete and relapse are common. [20],[21] Various treatments have been described for nail changes in YNS with varying efficacy. Proximal matrix intralesional triamcinolone have shown partial response. [22] Topical and oral vitamin E 800 U for 12-18 months is thought to be effective due to its antioxidant role thereby reducing lipofuscin deposition and by increasing the nail growth rate. [15],[23] Oral zinc 300 mg has shown result in one case report. [24]
Blue chromonychia
Blue discoloration of nails is most commonly drug induced. Minocycline causes bluish discoloration of the nail bed with sparing of lunulae in association with cutaneous and mucosal discoloration. This is said to be caused due to dermal deposition of iron chelates. [25] Antimalarials cause blue brown discoloration probably due to the deposition of melanin and hemosiderin. [26] Chemotherapeutics like cyclophosphamide, doxorubicin, and bleomycin cocktail therapy causes blue chromonychia due to matrix melanocyte activation. Similar discoloration is also reported with the use of azidothymidine for AIDS. [15]
Beside drugs, other causes of blue nails include exposure to silver salts either occupationally or as medications, Wilsons disease (causing Azure lunula), glomus tumor of nail, digital arterio-venous malformation, hereditary acrolabial telangiectasia, and advanced AIDS infection [15] [Figure - 5].
 |
| Figure 5: Bluish discoloration due to underlying glomus tumor |
Transient bluish discoloration may indicate a cyanotic nail or methemoglobinemia
Red chromonychia
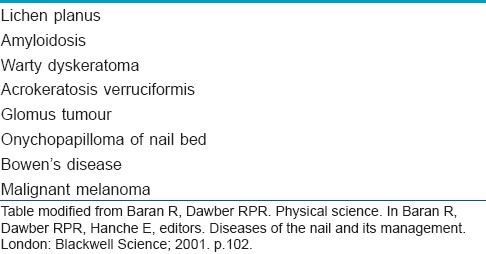
Red discoloration of the nail may be limited to lunulae or involve nail bed either longitudinally or diffusely. Red lunula is seen in psoriasis, alopecia areata, systemic lupus erythematosus and trachyonychia, apart from many other endocrine, gastrointestinal, cardiovascular, neurological, rheumatic, and infectious disorders. Longitudinal erythronychia is characteristically present in Dariers′s disease, but many other disorders may at times present with longitudinal erythronychia. [1] Various causes of the same is mentioned in [Table - 3]. Psoriatic ′oil spots′, lichen planus, glomus tumour, hematomas and carbon monoxide poisoning may present as red discoloration of the nail bed. Splinter hemorrhages may present as red-brown lines running along the length of nail.
Green chromonychia
Nail or periungual infection by Pseudomonas aeruginosa may give rise to a green-yellow discoloration of the nail apparatus due to the deposition of pyocyanin or fluorescein [Figure - 6]. The diagnosis can be made by soaking the fragments of nail in water or chloroform. If these turn green, it reflects that the discoloration is most likely due to pseudomonal infection. [1]
 |
| Figure 6: Pseudomonal infection induced green discoloration of nail |
Miscellaneous dyschromia
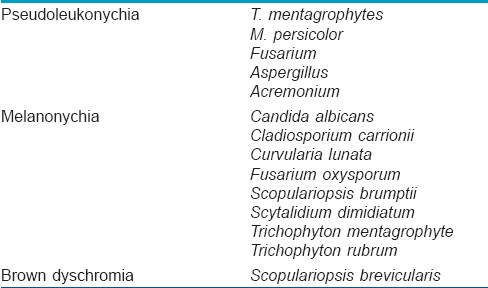
Fungal chromonychia: Fungal infection of the nail apparatus or onychomycosis may lead to various types of discoloration depending on the species of fungus involved [1] [Table - 4]. Superficial white onychomycosis gives rise to pseudo leukonychia.
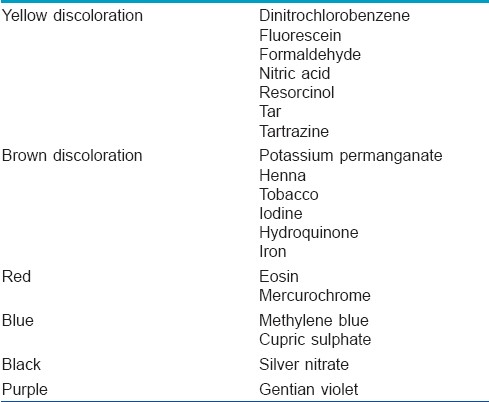
Exogenous agents: Exposure of the nail plate to various topical agents, either accidently, occupationally or as a cosmetic procedure may give rise to discoloration of the nail plate. Various commonly encountered agents and the type of discoloration caused by them is tabulated in [Table - 5].
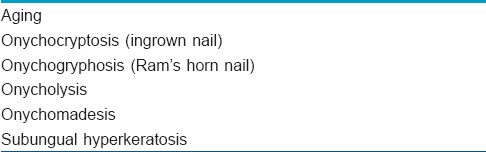
Morphological changes: Certain morphological changes of the nail may also simulate dyschromia of the nail due to their dirty yellow-brown discoloration, but are not examples of true nail dyschromia. A list of such morphological nail changes are enumerated in [Table - 6].
Thus, we see that a small apparatus like nail can help unravel a large number of systemic and local disorders and be a pointer towards many disease processes which may not otherwise be apparent. Therefore, examination of nail should always be a part of routine cutaneous examination and presentation with nail dyschromias should be worked up with the help of a good history and examination and few easy bed side tests which may help in reaching the diagnosis with relative ease and little invasion.
| 1. |
Baran R, Dawber RP. Physical science. In: Baran R, Dawber RP, Hanche E, editors. Diseases of the nail and its management. London: Blackwell Science; 2001. p. 85-103.
[Google Scholar]
|
| 2. |
André J, Lateur N. Pigmented nail disorders. Dermatol Clin 2006;24:329-40.
[Google Scholar]
|
| 3. |
Jeanmougin M, Civatte J. Nail dyschromias. Int J Dermatol 1983;22:279-90.
[Google Scholar]
|
| 4. |
Goldman L. Transillumination of fingertips as aid in examination of nail changes. Arch Dermatol 1962;85:644.
[Google Scholar]
|
| 5. |
Butterworth T. Leukonychia partialis leukonychia totalis. Cutis 1982;29:363-7.
[Google Scholar]
|
| 6. |
Higashi N, Sugai T, Yamamoto T. Leukonychia striata longitudinalis. Arch Dermatol 1971;104:192-6.
[Google Scholar]
|
| 7. |
Tosti A, De Padova MP, Fanti P. Nail involvement in lichen plano pilaris. Cutis 1988;42:213-4.
[Google Scholar]
|
| 8. |
Conn RD, Smith RH. Malnutrition, myxoedema and Muehrcke's lines. Arch Intern Med 1965;116:875-8.
[Google Scholar]
|
| 9. |
Donald GF, Hunter GA, Gillam BD. Transverse leukonychia due to pellagra. Arch Dermatol 1962;85:530.
[Google Scholar]
|
| 10. |
Robinson-Bostom L, DiGiovanna JJ. Cutaneous manifestations of end-stage renal disease. J Am Acad Dermatol 2000;43:975-86.
[Google Scholar]
|
| 11. |
Ramos-e-Silva M, Azevedo-e-Silva M, Carneiro SC. Hair, nail and pigment changes in major systemic disease. Clin Dermatol 2008;26:296-305.
[Google Scholar]
|
| 12. |
Zágoni T, Sipos F, Tarján Z, Péter Z. The half-and-half nail: A new sign of Crohn's disease? Report of four cases. Dis Colon Rectum 2006;49:1071-3.
[Google Scholar]
|
| 13. |
Silva P, Vera C, Kolbach M, Fernández F. Suspicion of systemic diseases through nails abnormalities. Rev Med Chil 2006;134:231-8.
[Google Scholar]
|
| 14. |
Braun RP, Baran R, Le Gal FA, Dalle S, Ronger S, Pandolfi R, et al. Diagnosis and management of nail pigmentation. J Am Acad Dermatol 2007;56:835-47.
[Google Scholar]
|
| 15. |
Goodman GJ, Nicolopoulos J, Howard A. Diseases of the generative nail apparatus. Part II: Nail bed. Australas J Dermatol 2002;43:157-68.
[Google Scholar]
|
| 16. |
Ohkuma M. Studies on yellow nail syndrome. In: Kukita A, Seji M, editors. Proceedings of the 16 th International Congress on Dermatology. Tokyo: Tokyo University Press; 1982.
[Google Scholar]
|
| 17. |
Emerson PA. Yellow nails, lymphedema and pleural effusion. Thorax 1966;21:247-53.
[Google Scholar]
|
| 18. |
Hiller E, Rosenow EC 3rd, Olsen AM. Pulmonary manifestations of the yellow nail syndrome. Chest 1972;61:452-8.
[Google Scholar]
|
| 19. |
Verdejo C, Marín-Hernández G, Villacastín BP, Renedo G, Largacha MG, Medina ML, et al. Yellow nail syndrome: Presentation of case and review of literature. Rev Clin Esp 1992;191:152-5.
[Google Scholar]
|
| 20. |
Samman PD. Nail disorders associated with general medical conditions. In: Samman PD, editor. The nails in disease. London: William Heinemann; 1986. p. 102-20.
[Google Scholar]
|
| 21. |
Norton L. Further observations on the yellow nail syndrome and therapeutic effects of oral alpha tocopherol. Cutis 1985;36:157-62.
[Google Scholar]
|
| 22. |
Abell F, Samman PD. Yellow nail syndrome treated by intralesional triamcinolone acetonide. Br J Dermatol 1991;88:200-1.
[Google Scholar]
|
| 23. |
Williams HC, Buffham R, Du Vivier A. Successful treatment of topical vitamin E solution in the treatment of nail changes in yellow nail syndrome. Arch Dermatol 1991;127:1023-8.
[Google Scholar]
|
| 24. |
Arroyo JF, Cohen ML. Improvement of yellow nail syndrome with oral zinc supplementation. Clin Exp Dermatol 1993;18:62-4.
[Google Scholar]
|
| 25. |
Eisen D, Hakim MD. Minocycline induced pigmentation. Incidence, prevention and management. Drug Saf 1998;18:4431-40.
[Google Scholar]
|
| 26. |
Fenton DA. Nail changes due to drugs. In: Samman PD, editor. The Nails in Disease. London: William Heinemann; 1986. p. 121-5.
[Google Scholar]
|
Fulltext Views
25,865
PDF downloads
4,608





