Translate this page into:
Neonatal herpes simplex infection acquired from herpes mastitis: An unusual mode of transmission
2 Department of Dermatology, Virk Hospital Private Limited, Karnal, Haryana, India
Correspondence Address:
Simin Muhammed Kutty
Kushboo, Golf Link Road, Chevayur, Kozhikode - 673 017, Kerala
India
| How to cite this article: Kutty SM, Nagesh M, Mann P. Neonatal herpes simplex infection acquired from herpes mastitis: An unusual mode of transmission. Indian J Dermatol Venereol Leprol 2020;86:559-561 |
Sir,
Neonatal herpes is usually transmitted vertically by herpes simplex virus-2 during the peripartum period. As only 10% of infected neonates acquire the virus postnatally, neonatal herpes simplex virus infection acquired from maternal breast lesions during lactation is rather uncommon.[1]
A 7-day-old, exclusively breastfed baby boy (birth weight of 2.9 kg) born via vaginal delivery presented with a high-grade fever of 2 day duration and fluid-filled lesions on the right thumb and right arm of 1 day duration. His mother gave a history of painful erosions on the left breast associated with a swelling that had appeared 2 days prior to delivery. She had oral/hand nipple contact with her partner 1 week before delivery. Neither she nor her partner gave any history of genital or oral lesions.
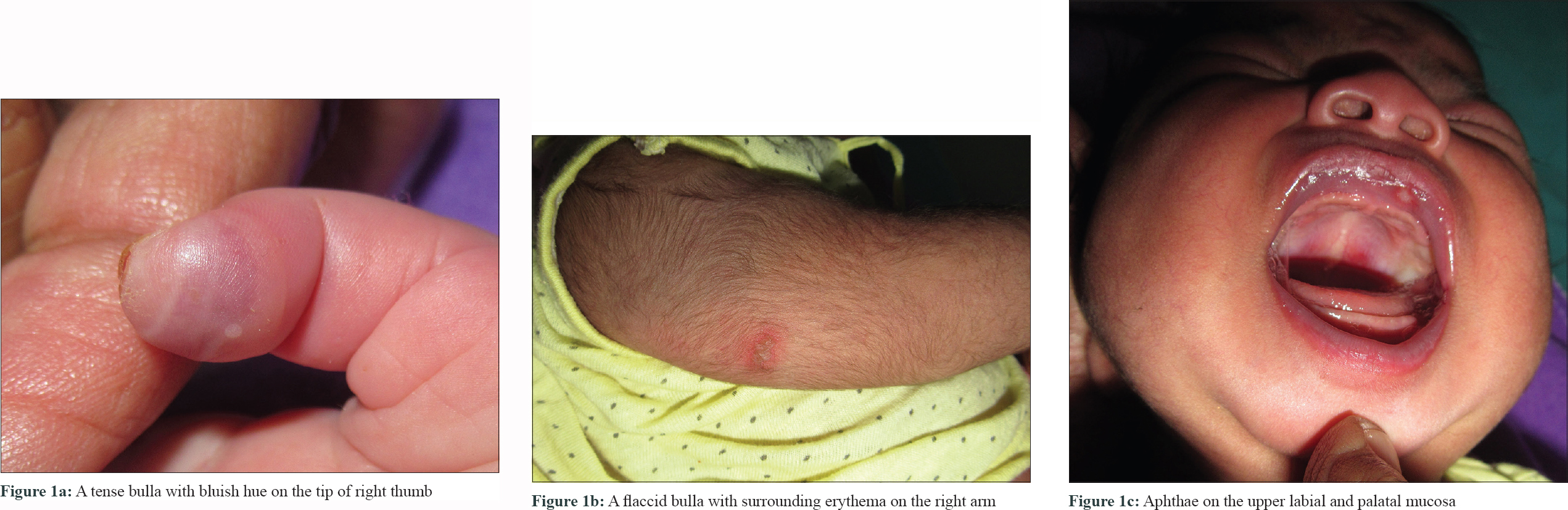
Examination of the febrile neonate (102 °F) revealed a tense bulla on the tip of his right thumb [Figure - 1]a associated with paronychia and onycholysis, a flaccid bulla of size 2 cm x 1 cm with surrounding erythema on the right arm [Figure - 1]b and aphthae of 0.5 cm x 0.5 cm size over upper labial and palatal mucosa [Figure - 1]c. Ophthalmic and systemic examination of the baby was normal. The mother had an ulcer sized 3 cm x 0.5 cm, with an irregular margin and scanty serosanguinous discharge around the left nipple and small healed erosions over the areola [Figure - 2]. An otherwise healthy neonate presenting with fever and vesicular lesions 1 week post delivery and an irregular painful ulcer with small round healed erosions around it on the mother's breast led to the suspicion of herpes simplex infection clinically in this case.
 |
 |
| Figure 2: An ulcer with an irregular margin around the left nipple and small, healed erosions on the areola |
Complete hemogram, hepatic parameters, cerebrospinal fluid study including bacterial culture, herpes simplex virus deoxyribonucleic acid polymerase chain reaction, chest X-ray and abdominal ultrasound of the baby were normal. Tzanck smear from the neonate's vesicle showed multinucleated giant cells [Figure - 3] but from the maternal ulcer revealed only neutrophils. Whole blood examination and swabs from the base of vesicles, mucous membrane lesions, conjunctiva and nasopharynx of the neonate, mother's ulcer and vagina were sent for deoxyribonucleic acid polymerase chain reaction study.
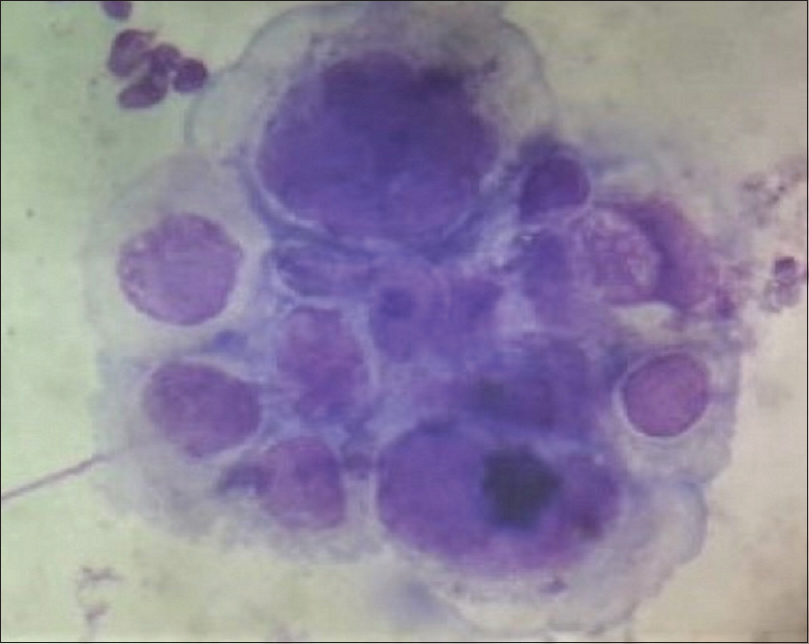 |
| Figure 3: Tzanck smear showing multinucleated giant cell (Leishman stain, ×400) |
A provisional diagnosis of neonatal herpes with skin, eyes and/or mouth involvement acquired from maternal herpes mastitis was made and the neonate was immediately started on intravenous acyclovir 20 mg/kg/day 8 hourly with other supportive measures. The mother was successfully treated with oral acyclovir 400 mg three times daily for 1 week. Lesional swabs taken from both mother and child and whole blood from the neonate later confirmed herpes simplex virus-1 infection by deoxyribonucleic acid polymerase chain reaction study while the swab taken from the mother's genital tract gave a negative result. The baby was discharged in a clinically stable condition after completion of the 14-day acyclovir course.
Postnatally acquired herpes simplex virus infection occurs as a result of direct contact with herpes simplex virus-infected person, usually from an orolabial or a cutaneous source. Reports of neonatal herpes acquired from maternal breast lesions during lactation are scarce. Herpes simplex virus mastitis is rather uncommon with an estimated frequency of about 2% of all extragenital herpes simplex virus lesions[2] and is predominately transmitted from a herpes simplex virus-infected neonate to the mother during breastfeeding.[3] Breast lesion in our patient started 2 days before delivery ruling out the above possibility. Other possible modes of acquiring herpes simplex virus mastitis include either by contact with an asymptomatic carrier (as a person can carry the virus in the saliva without any clinical manifestation and infect another person during a close contact) or through autoinoculation, especially in a patient with a history of recurrent herpes labialis or genitalis.[3]
The definitive method of diagnosing neonatal herpes simplex virus is by isolation in viral tissue culture (gold standard) or by herpes simplex virus deoxyribonucleic acid polymerase chain reaction (particularly to diagnose central nervous system disease).[1] A bedside test like the Tzanck test, direct fluorescent-antibody test or an enzyme immunoassay for herpes simplex virus antigens from skin lesions can be useful for an initial diagnosis.[4] Before starting empiric intravenous acyclovir therapy in a neonate, it is recommended that the following samples be obtained- cerebrospinal fluid for indices and herpes simplex virus deoxyribonucleic acid polymerase chain reaction, swabs from the base of the vesicle and mucous membrane lesions for viral culture or polymerase chain reaction, swabs from the mouth, conjunctiva, nasopharynx for viral culture or polymerase chain reaction, whole blood for a polymerase chain reaction and blood for alanine aminotransferase level.[1] Likelihood of transplacentally acquired maternal IgG confounding neonatal antibody status (given the high seroprevalence of herpes simplex virus antibodies in the general population) coupled with lack of reliable type-specific IgM herpes simplex virus antibody assays were the main reasons for not doing serology in our patient for diagnosing neonatal herpes infection.[4] Moreover, IgM antibodies may take up to 10 days to develop and the ability to produce antibodies can be impaired in some severely affected neonates.[4],[5]
Neonatal herpes infection though uncommon, is associated with significant morbidity and mortality. Hence, to prevent infants from being exposed to the herpes virus, women with a negative personal history of herpes simplex virus (especially those with a positive history in the male partner) should be counselled to abstain from sexual activity, especially during the third trimester of pregnancy even if the male partner has no active lesions.[6] Mothers with active lesions on the breast should temporarily stop breastfeeding from the affected breast and should discard expressed milk from the affected side until the lesions have healed completely.[7] She may breastfeed from the unaffected breast but should ensure that the lesions on the affected breast are completely covered. These simple measures could have prevented the transmission of infection in our case if herpes mastitis was diagnosed at the earliest. However, it remains rather an underdiagnosed or misdiagnosed entity.
Our case highlights the need for healthcare providers to be aware of the various modes of transmission of neonatal herpes especially from herpes infection of maternal breast and the importance of taking necessary precautionary measures. Furthermore, the case underscores the importance of maintaining a high index of suspicion while managing a febrile neonate with vesicular lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pinninti SG, Kimberlin DW. Neonatal herpes simplex virus infections. Semin Perinatol 2018;42:168-75.
[Google Scholar]
|
| 2. |
Corey L, Adams HG, Brown ZA, Holmes KK. Genital herpes simplex virus infections: Clinical manifestations, course, and complications. Ann Intern Med 1983;98:958-72.
[Google Scholar]
|
| 3. |
Toussaint A, Simonson C, Valla C. Herpes mastitis: Diagnosis and management. Breast J 2016;22:335-8.
[Google Scholar]
|
| 4. |
Allen UD, Robinson JL; Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Prevention and management of neonatal herpes simplex virus infections. Paediatr Child Health 2014;19:201-12.
[Google Scholar]
|
| 5. |
Page J, Taylor J, Tideman RL, Seifert C, Marks C, Cunningham A, et al. Is HSV serology useful for the management of first episode genital herpes? Sex Transm Infect 2003;79:276-9.
[Google Scholar]
|
| 6. |
Brown ZA, Gardella C, Wald A, Morrow RA, Corey L. Genital herpes complicating pregnancy. Obstet Gynecol 2005;106:845-56.
[Google Scholar]
|
| 7. |
Lawrence RA, Lawrence RM, editors. Transmission of infectious disease through breast milk and breast feeding. In: Breastfeeding: A Guide for the Medical Profession. 8th ed.. Philadelphia, PA: Elsevier; 2016. p. 440.
[Google Scholar]
|
Fulltext Views
7,893
PDF downloads
2,160





