Translate this page into:
Neutrophil-to-lymphocyte Ratio: A Biomarker for Predicting Systemic Involvement in Henoch–Schonlein Purpura
Corresponding author: Prof. Xu Ai-E, Department of Dermatology, Third People’s Hospital of Hangzhou, Hangzhou, China. shitoujiandaobuw@sina.com
-
Received: ,
Accepted: ,
How to cite this article: Lei W, Yun-Yun S, Ai-E X. Neutrophil-to-lymphocyte ratio: A biomarker for predicting systemic involvement in Henoch-Schonlein purpura. Indian J Dermatol Venereol Leprol 2022;88:132.
Abstract
Background:
Henoch–Schonlein purpura (HSP) is one of the commonest entities included within the category of cutaneous vasculitis (CV). Our work is purposed to explore the predictive value of neutrophil-to-lymphocyte ratio (NLR) for systemic involvement in Henoch– Schonlein purpura patients. This ratio is known as an inflammatory marker, and is used to assess the systemic inflammation associated with various diseases. Our objective is to establish whether it can be applied for the prediction of renal and gastrointestinal (GI) or purely renal involvement in Henoch–Schonlein purpura.
Aim:
To determine the relationship between neutrophil-to-lymphocyte ratio and systemic involvement in Henoch–Schonlein purpura
Methods:
This is a retrospective review of the patients who were diagnosed with Henoch–Schonlein purpura in our hospital between 2012 and 2018.
Results:
A total of 57 patients met our inclusion criteria. Pre-treatment neutrophil-to-lymphocyte ratio was significantly associated with renal and/or GI manifestations of the disease (p<0.001). The optimal cut-off value of this ratio for predicting systemic involvement was 2.48, with a 95% specificity and a 94% sensitivity. In addition, pretreatment ratio was also found to be significantly correlated with the severity of relevant systemic manifestations of Henoch–Schonlein purpura (r=0.831; p<0.01).
Limitations:
The small number of patients recruited for our research, its retrospective design, and the inclusion of patients attending the same hospital.
Conclusion:
This study suggests that neutrophil-to-lymphocyte ratio is suitable as a potential indicator for predicting the systemic involvement in Henoch–Schonlein purpura.
Keywords
Henoch–Schonlein purpura
neutrophil-to-lymphocyte ratio
kidney
gastrointestinal
Introduction
Henoch–Schonlein purpura (HSP) is one of the commonest entities included within the category of cutaneous vasculitis (CV). It most commonly presents as palpable purpura on the lower extremities, arthritis or arthralgia and systemic manifestations, such as gastrointestina (GI) or renal involvement.1-5 Prognosis depends on the severity of organ involvement, which highlights the importance and necessity to find the right prognostic markers that can help identify Henoch–Schonlein purpura patients at risk of developing unfavorable extracutaneous manifestations.
As an easily obtainable and inexpensive laboratory marker for quantifying systemic inflammation, blood neutrophilto-lymphocyte ratio (NLR) has been used to predict clinical outcomes in the patients with various internal malignancies, liver cirrhosis and cardiovascular diseases.6-10 As this ratio integrates information on two immune pathways, it may provide a means of prediction that outweighs other inflammatory parameters. Our report is related to the neutrophil-to-lymphocyte ratio in patients with Henoch–Schonlein purpura. The aim of this study is to evaluate the utility of this ratio in predicting renal and GI involvement in Henoch–Schonlein purpura patients.
Materials and Methods
All of the patients diagnosed with Henoch–Schonlein purpura in our hospital between April 2012 and November 2018 were reviewed [Figure 1]. The European League against Rheumatism/Paediatric Rheumatology European Society (EULAR/PRES) diagnostic criteria developed for HSP11 were applied to define the disease as palpable purpura (a mandatory criterion) with at least one of the following conditions met: (1) diffuse abdominal pain; (2) any biopsy showing predominant IgA deposition; (3) arthritis or arthralgia; and (4) renal involvement (hematuria and/or proteinuria). The patients would be excluded if they had an immunologic comorbidity, coexisting internal malignancy, hematological disorder, cryoglobulinemia or any chronic renal or GI diseases. Additionally, the patients who had manifested hematuria, hematochezia, melena or hematemesis two days before or after blood sampling were also excluded due to the possibility of neutrophilia being the secondary effect of an acute hemorrhage.The study was granted approval from the local ethics review committee.

- Typical palpable purpura on the legs of a patient with Henoch-Schonlein purpura
The demographic data, signs and symptoms of disease as well as laboratory data obtained at the time of diagnosis were recorded by the computerized patient database, for example, erythrocyte sedimentation rate (ESR), c-reactive protein (CRP), hemoglobin level, white blood cell count (WBC), platelet count, mean platelet volume and neutrophil-to-lymphocyte ratio.
GI involvement was defined as the clinical signs of hematochezia, melena or hematemesis. Alternatively, it was referred to as a positive test result for fecal hemoglobin. Renal involvement was determined through hematuria (>5 red blood cells per high-power microscopic field in a centrifuged specimen; in the absence of urolithiasis, anticoagulant therapy, absence of and concurrent urinary tract infections) or proteinuria (>150 mg/24h),
Statistical analysis
All data was analyzed using statistical package for social sciences 16.0 (SPSS, Inc., Chicago, Illinois, USA) for windows. Quantitative variables were denoted as mean ±SD for normally distributed data and as medians (25th and 75th percentiles) for non-normally distributed data. The quantitative data on dual groups was compared by means of the mann–whitney U test when appropriate. The correlations between parameters were computed through the Pearson’s correlation analysis. Besides, backward stepwise logistic regression analysis was conducted to determine the variables associated with GI and/or renal manifestations in the patients with Henoch–Schonlein purpura. The correlations between different parameters were examined via spearman’s rank correlation coefficient test. Receiver operating characteristic (ROC) curves were adopted to evaluate the potential indicators of GI and/or renal manifestations in Henoch–Schonlein purpura. p value ≤0.05 was treated as significant. The correlations between different parameters were examined by means of the rank correlation coefficient test proposed by Spearman.
Results
There were 57 patients diagnosed with Henoch–Schonlein purpura recruited for the study. Among them, 31 patients were female and the remaining 26 patients were male. On average, the age of the Henoch–Schonlein purpura patients was 49 ± 22 years. They were divided into two groups. Group 1 included the patients who showed only cutaneous symptoms, while group 2 consisted of the patients with GI and/or renal manifestations, in addition to the cutaneous symptoms. The laboratory parameters of these two groups are listed in Table 1. Of the registered inflammatory markers, WBC (p=0.002), CRP (p=0.006), neutrophil-to-lymphocyte ratio (p<0.001) and erythrocyte sedimentation rate (ESR, p=0.023) were significantly higher in group 2, whereas the other laboratory parameters, plate; et count and mean platelet volume, were not statistically associated with systemic involvement.
| Parameter | Group 1 (n=36) | Group 2 (n=21) | p value** |
|---|---|---|---|
| Hb (g/dL) | 132.0 (121.3-142.7) | 135.3 (122.5-148.2) | 0.446 |
| WBC (×103/μL) | 6.1 (5,5-7.2) | 8.0 (6.8-8.9) | 0.002 |
| PLT (×103/μL) | 255.0 (219.7-317.5) | 240.0 (199.0-285.5) | 0.209 |
| MPV (fL) | 9.9 (9.0-11.0) | 10.0 (9.4-10.9) | 0.649 |
| Neutrophil (×103/μL) | 3.4 (2.8-4.3) | 5.6 (4.7-6.6) | 0.000 |
| Lymphocyte (×103/μL) | 2.2 (1.8-2.5) | 1.3 (0.9-1.5) | 0.000 |
| NLR (%) | 1.7 (1.2-2.1) | 4.3 (3.5-6.5) | 0.000 |
| CRP (mg/L) | 6.0 (2.6-10.4) | 12.0 (4.3-41.4) | 0.006 |
| ESR mm/h | 7.9 (5.0-18.5) | 20.0 (6.5-31.0) | 0.023 |
Data were presented as median (25th and 75th percentile)
WBC counts, CRP levels, neutrophil-to-lymphocyte ratio and ESR were subjected to logistic regression analysis as potential indicators of systemic involvement in Henoch–Schonlein purpura. Only neutrophil-to-lymphocyte ratio was associated with systemic manifestations in Henoch–Schonlein purpura (p values are 0.016), as shown in Table 2.
| B | SE | Wald | P value | Exp (B) | 95%CI | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| WBC (×103/μL) | 0.706 | 0.534 | 1.744 | 0.187 | 2.025 | 0.711 | 5.772 |
| NLR (%) | 5.433 | 2.256 | 5.799 | 0.016 | 228.920 | 2.749 | 19063.914 |
| CRP (mg/L) | -0.027 | 0.074 | 0.135 | 0.713 | 0.973 | 0.842 | 1.125 |
| ESR (mm/h) | -0.033 | 0.098 | 0.114 | 0.735 | 0.967 | 0.797 | 1.173 |
NLR: Neutrophil-to-lymphocyte ratio, ESR: erythrocyte sedimentation rate, WBC: White blood cell count
The ROC curves of neutrophil-to-lymphocyte ratio and other inflammatory markers related to systemic involvement are shown in Figure 2. The area under the curve (AUC) for neutrophil-to-lymphocyte ratio, CRP, ESR and WBC was 0.987 (95% CI: 0.966-1; p<0.001), 0.650(95% CI: 0.485-0.815; p=0.060), 0.023 (95% CI: 0.530-0.834; p=0.068) and 0.745 (95% CI 0.609-0.881; p=0.023), respectively. Among the considered laboratory data, neutrophil-to-lymphocyte ratio demonstrated the highest diagnostic value, as indicated by the highest AUC value. The optimal cut-off value of neutrophil-tolymphocyte ratio for predicting systemic involvement was 2.48, with a specificity of 95% and a sensitivity of 94%.
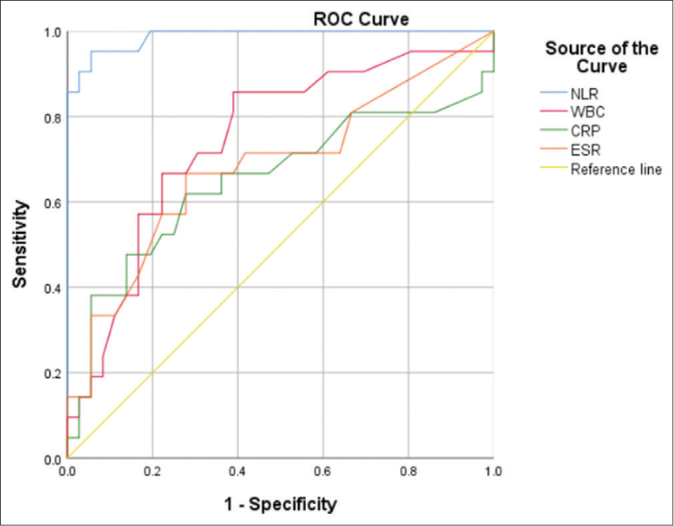
- Receiver operating characteristic curve of admission neutrophil-tolymphocyte ratio and other inflammatory markers in relation to the systemic involvement
A further examination was conducted on the correlation between neutrophil-to-lymphocyte ratio and the severity of disease in the patients with renal and/or gastrointestinal involvement. In this regard, a simple seven-point scoring system was constructed considering the clinical manifestations and course of the disease, as observed among the involved cases. The patients received one point for the presence of each of the following features: hematuria, renal impairment, proteinuria, fecal hemoglobin positivity, macroscopic bleeding from the GI tract, the necessity of intensive care unit(ICU)/surgery/ blood transfusion/and death. neutrophil-to-lymphocyte ratio was found to be significantly associated with the score for the severity of disease (r=0.831; p<0.001) [Figure 3]. No patient in our study required surgery and there were no deaths, in the patients who were included in group 2, as shown in Table 3.

- The correlation of neutrophil-tolymphocyte ratio and disease severity in patients with renal and/or gastrointestinal involvement
| Group 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hematuria | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||
| Renal impairment | 1 | 1 | 1 | ||||||||||||||||||
| Proteinuria | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| Fecal hemoglobin positivity | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||
| Macroscopic bleeding | 1 | 1 | |||||||||||||||||||
| ICU/surgery/blood transfusion | 1 | ||||||||||||||||||||
| NLR | 2.93 | 4.7 | 3.6 | 3.56 | 5.19 | 2.13 | 7.22 | 2.5 | 7.93 | 4.27 | 6.48 | 3.4 | 8.3 | 3.66 | 4.9 | 5.89 | 9 | 3.4 | 6.7 | 3.9 | 3.91 |
Discussion
Henoch–Schonlein purpura is a small vasculitis and is mediated by the deposition of immune complexes. It can cause severe complications in some of the patients, including renal impairment and serious GI bleeding that may require intensive care or surgery.
In previous studies, it has been suggested that neutrophil-tolymphocyte ratio was not only more significantly increased in the Henoch–Schonlein purpura patients with GI bleeding when compared to the patients without GI bleeding, but also influenced prognosis.12-14 Our work is purposed to explore the predictive value of neutrophil-to-lymphocyte ratio for the systemic involvement in Henoch–Schonlein purpura patients.
Despite the fact that neutrophil-to-lymphocyte ratio cannot completely capture the complexity of inflammation and immune responses in Henoch–Schonlein purpura, this disease is shown to be neutrophil-dependent. Besides, it may be sensible to consider that a high ratio might be partially related to more severe immune response in those small vessel vasculitis of the skin. Neutrophil-to-lymphocyte ratio is measured by dividing neutrophil count to lymphocyte count. An increase in neutrophil count accompanied by a fall in lymphocyte count is commonly seen in various infectious and noninfectious causes of systemic inflammation and stress. Besides, lymphopenia may occur in some inflammatory conditions, such as sepsis, due to the increased lymphocyte apoptosis. So far, neutrophilto-lymphocyte ratio has been demonstrated as a potentially useful indicator of clinical outcome in disease states with an inflammatory component.15-18 For example, it is associated with poor outcomes in the patients with cardiovascular diseases, malignancies, cystic fibrosis, and familial mediterranean fever.
As expected, it was found that neutrophil counts were significantly higher in group 2 than in group 1, and that the patients with GI and/or renal manifestations had significantly lower lymphocyte counts than those without GI and/or renal manifestations. Our results demonstrated that among the considered inflammatory parameters, neutrophilto-lymphocyte ratio had the highest diagnostic value. The optimal cut-off point for predicting systemic involvement was 2.48 with a specificity of 94% and a sensitivity of 95%. None of the patients in our cohort with a lower neutrophil-tolymphocyte ratio value than 2.48 displayed any clinical signs suggestive of renal and GI involvement, during admission or follow-up, which further confirms the prognostic value of neutrophil-to-lymphocyte ratio. It is worth noting that when neutrophil-to-lymphocyte ratio was greater than 2.48 but the patient showed no organ involvement, close observation of the clinical condition and repeated urine/stool examination revealed renal or GI involvement in the following few days.
A seven-point scoring system was used to assess the organ involvement in HSP. It was also found out that the pre-treatment neutrophil-to-lymphocyte ratio values were significantly correlated with the severity of the disease in the patients developing systemic involvement. The most severe case in our follow-up had gastrointestinal or renal involvement, which required transfer to the ICU because of unstable vital signs. The neutrophil-to-lymphocyte ratio value of this patient was the highest in this study. However it is worth noting that, when the scoring system was used to evaluate this correlation in our study, we considered solely the presence or absence of certain clinical manifestations, rather than assessing the extent of renal or GI symptoms on a spectrum.
The major limitations on this study include the small number of recruited patients, its retrospective design, and the inclusion of patients who all attended the same Hospital. Therefore, multicenter prospective studies including a larger number of patients are necessary to confirm and generalize our results.
In conclusion, our results have suggested that neutrophilto-lymphocyte ratio is a potential prognostic marker for the systemic involvement in Henoch–Schonlein purpura and can be used to identify the patients at risk of developing extracutaneous manifestations. In addition, it was also found out that increased pretreatment neutrophil-to-lymphocyte ratio was correlated with the severity of the systemic involvement.
References
- The differential diagnosis of purpura from a morphologic perspective. Adv Dermatol. 1994;9:3-23.
- [Google Scholar]
- Small vessel vasculitis of the skin. Rheum Dis Clin North Am. 2015;41:21-32.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic significance of neutrophil to lymphocyte ratio in patients with gallbladder carcinoma. HPB (Oxford). 2016;18:600-7.
- [CrossRef] [PubMed] [Google Scholar]
- IgM in lesional skin of adults with Henoch-Schönlein purpura is an indication of renal involvement. J Am Acad Dermatol. 2010;63:1026-9.
- [CrossRef] [PubMed] [Google Scholar]
- Correlates of systemic disease in adult Henoch-Schönlein purpura: a retrospective study of direct immunofluorescence and skin lesion distribution in 87 patients at Mayo Clinic. J Am Acad Dermatol. 2012;67:612-6.
- [CrossRef] [PubMed] [Google Scholar]
- Henoch-Schönlein purpura in adulthood and childhood: two different expressions of the same syndrome. Arthritis Rheum. 1997;40:859-64.
- [CrossRef] [PubMed] [Google Scholar]
- Schönlein-Henoch purpura in adult patients. Predictive factors for IgA glomerulonephritis in a retrospective study of 57 cases. Arch Dermatol. 1997;133:438-42.
- [CrossRef] [PubMed] [Google Scholar]
- The blood neutrophil to lymphocyte ratio correlates with clinical status in children with cystic fibrosis: a retrospective study. PLoS One. 2013;8:e77420.
- [CrossRef] [PubMed] [Google Scholar]
- EULAR/PReS endorsed consensus criteria for the classification of childhood vasculitides. Ann Rheum Dis. 2006;65:936-41.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil-to-lymphocyte ratio to predict gastrointestinal bleeding in Henoch: Schönlein purpura. Pediatr Int. 2018;60:791-5.
- [CrossRef] [PubMed] [Google Scholar]
- Predictive role of neutrophil to lymphocyte ratio in Henoch-Schonlein purpura related gastrointestinal bleeding. Rheumatol Int. 2014;34:1331-2.
- [CrossRef] [PubMed] [Google Scholar]
- The Optimal Cut-Off Value of Neutrophil-to-Lymphocyte Ratio for Predicting Prognosis in Adult Patients with Henoch-Schönlein Purpura. PLoS One. 2016;11:e0153238.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic importance of baseline neutrophil to lymphocyte ratio in patients with advanced papillary thyroid carcinomas. Endocrine. 2014;46:526-31.
- [CrossRef] [PubMed] [Google Scholar]
- Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;15:653-7.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction. Am J Cardiol. 2008;101:747-52.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005;91:181-4.
- [CrossRef] [PubMed] [Google Scholar]






