Translate this page into:
Neutrophilic figurate erythema recurring on the same site in a middle-aged healthy woman
2 Department of Dermatology, Calcutta Skin Institute, 169, VI M CIT Scheme, Kolkata, India
Correspondence Address:
Sudip Kumar Ghosh
Department of Dermatology, Venereology, and Leprosy, R.G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata-700004
India
| How to cite this article: Ghosh SK, Bandyopadhyay D, Haldar S. Neutrophilic figurate erythema recurring on the same site in a middle-aged healthy woman. Indian J Dermatol Venereol Leprol 2012;78:505-508 |
Sir,
Figurate erythemas (FE) constitute a cluster of inflammatory cutaneous disorders, clinically characterized by annular, arcuate, serpiginous, or polycyclic lesions, widespread or localized distribution, and transient or persistent behavior. [1] Neutrophilic figurate erythema (NFE) is a rare inflammatory dermatosis, characterized by annular erythematous lesions, sometimes with polycyclic configurations with histological feature of neutrophic infiltration with nuclear dusts in the dermis. [2] ′NFE in infancy′ is a very rare disorder, [1],[3] and the disease is still rarer in adults.
A 47- year-old Hindu woman came with a gradually expanding oval red elevated skin lesion on her left forearm that was present for the preceding 4 days. She had occasional itching and mild pain over the lesion. There was neither any systemic complaint nor any history of intermittent or continuous drug intake prior to an eruption. She had a history of similar eruption over the same site a few months ago. She had no history of an insect bite. Cutaneous examination revealed a well-defined erythematous, shiny, firm, non-tender plaque (measuring 3 cm × 4 cm) on the extensor surface of the lower third of her left forearm. The surface of the lesion was wrinkled at places. [Figure - 1]a No sensory anomaly or peripheral nerve thickening was found. Examination of hair, nails and other systems was non-contributory. Histopathological examination could not be performed as the patient did not give consent for the same. However, the skin lesion resolved completely with an application of emollient only within 6 weeks. Twelve weeks later, the patient returned to us with a similar complaint. Examination showed a well-defined erythematous, firm, shiny, non-tender plaque (7 × 5 cm) on the extensor surface of her left forearm. There was relative clearing and fine scaling at the center of the lesion. The margins of the scales were attached peripherally [Figure - 1]b. A lesion with similar morphology was also present on her right shoulder (2 × 3 cm) [Figure - 1]c.
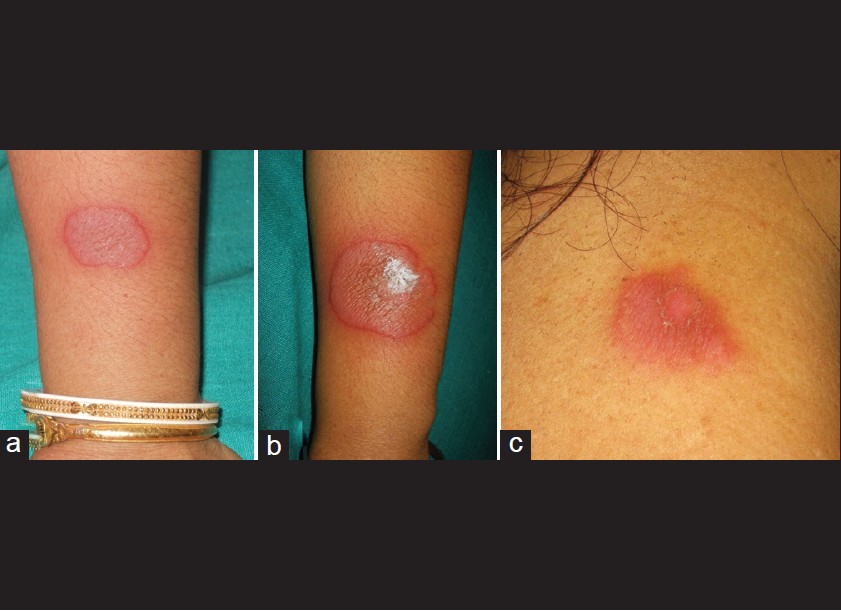 |
| Figure 1: (a) A well-delineated erythematous shiny plaque with wrinkled surface. (b) Erythematous glistening plaque with relative clearing and fine scaling at the center of the lesion. The margins of the scales were attached at the periphery. (c) Erythematous scaly plaque on the right shoulder |
There was no regional lymphadenopathy. There was gradual central clearing and peripheral expansion with fine trailing scales [Figure - 2].
 |
| Figure 2: Gradual central healing and peripheral expansion with fine trailing scales at (a) 4th day, (b) 3rd week, and at (c) 8th week of presentation |
The complete hemogram of the patient was normal, except for the raised ESR (63 mm/hr). Biochemical panel was normal. Skin scrapings for dermatophytes did not reveal any fungal element. Mantoux test (5 TU) showed an induration of 12 mm × 14 mm. ANA (by immunofluorescence; Hep2 cell line) was negative. Chest X-ray, ultrasonography of the abdomen, and gastrointestinal endoscopy was non-contributory. Histopathological examination (from both forearm and shoulder lesions) showed normal epidermis without any spongiosis or parakeratosis. There was papillary dermal edema with slightly dilated blood vessels, and dense perivascular infiltrate, mainly comprising of neutrophils, mononuclear cells and histiocytes. There were extravasations of RBCs, leukocytoclasis, and nuclear dusts formation without any evidence of vasculitis [Figure - 3]. The subcutaneous tissue was normal. Direct immunofluorescence was negative.
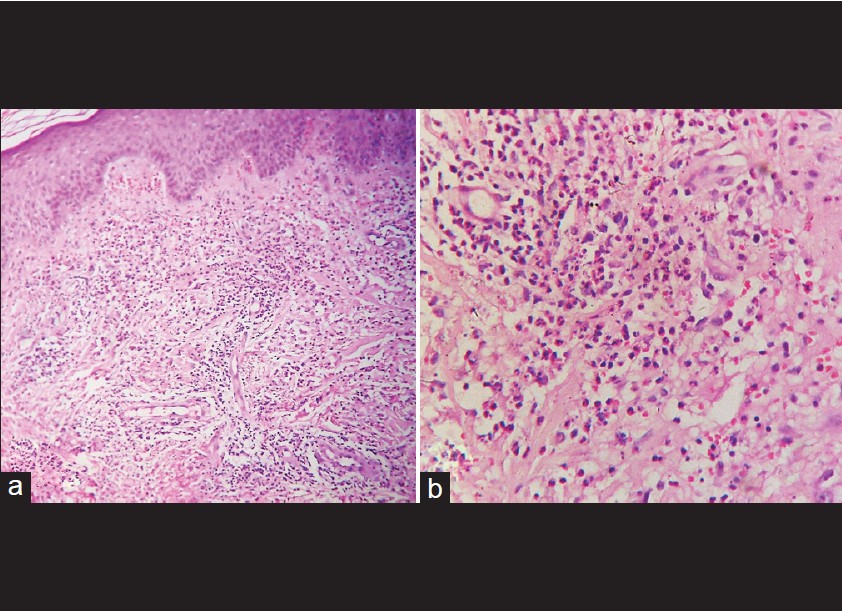 |
| Figure 3: (a) Papillary dermal edema dilated dermal blood vessels, and perivascular and interstitial infiltrate of neutrophils, mononuclear cells and histiocytes. (H and E, ×100) (b) Extravasations of erythrocytes and neutrophilic infiltrate with leukocytoclasia. (H and E, ×400) |
Based on the clinical and histopathological picture, a diagnosis of recurrent neutrophilic figurate erythema was made. The patient was treated with emollients, topical fluticasone propionate ointment (0.005%) for 2 weeks, and dapsone (100 mg/ day). The lesions completely resolved uneventfully within 8 weeks. The dose of dapsone was gradually tapered and stopped at 12 th week. There was no recurrence of lesions during a follow-up period of 1 year.
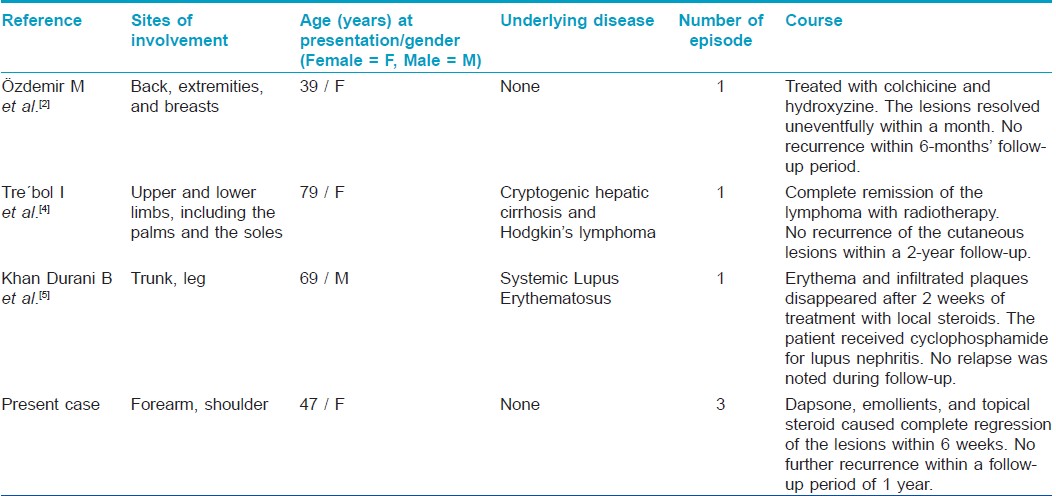
Only a few cases of NFE have been described in adults. [Table - 1] summarizes reported cases of NFE in adults in the English language literature as revealed by a PubMed database search. [2],[4],[5]
The lesions of NFE are asymptomatic or mildly pruritic and are characterized by arciform plaques, which may have a raised, firm erythematous border and trailing scale. Histologically, the lesions show superficial and deep perivascular and interstitial infiltrate of neutrophils and nuclear debris, [2] as seen in our patient. Other clinical differential diagnoses that were considered in the present case were, erythema annulare centrifugum (EAC), erythema chronicum migrans (ECM), erythema gyratum repens (EGR), annular variant of subacute cutaneous lupus erythematosus (SCLE) and Sweet syndrome. These differentials were ruled out on clinical and histopathological grounds.
Other histological differential diagnoses that present with neutrophilic dermatosis, like, pyoderma gangrenosum, rheumatoid neutrophilic dermatosis, Behcet′s syndrome, urticarial vasculitis, and acute generalized pustulosis, could easily be ruled out by the absence of the distinctive clinical features characteristic of these conditions.
NFE may be present with some underlying disease or in otherwise healthy individuals. [2] One case of NFE was described in an old man as a paraneoplastic manifestation of underlying malignancy. [4] Another case of neutrophilic figurate erythema with the morphology of erythema gyratum repens was reported in a patient with S.L.E. [5] However, our patient did not have any such association.
History of recurrence of lesions on more or less the same site within a span of a few months was an interesting feature in our patient. We seek to emphasize by this report that in spite of its rarity, a diagnosis of NFE should be considered in the differential diagnosis of erythematous scaly annular plaques in adults. Furthermore, while dealing with an annular or figurate inflammatory dermatosis in an adult, the treating physician should exclude any underlying disease including malignancy.
| 1. |
Annessi G, Signoretti S, Angelo C, Paradisi M, Puddu P. Neutrophilic figurate erythema of infancy. Am J Dermatopathol 1997;19:403-6.
[Google Scholar]
|
| 2. |
Ozdemir M, Engin B, Toy H, Demirkesen C. Neutrophilic figurate erythema. Int J Dermatol 2008;47:262-4.
[Google Scholar]
|
| 3. |
Patrizi A, Savoia F, Varotti E, Gaspari V, Passarini B, Neri I. Neutrophilic figurate erythema of infancy. Pediatr Dermatol 2008;25:255-60.
[Google Scholar]
|
| 4. |
Trébol I, González-Pérez R, García-Rio I, Arregui MA, Saracibar N, Carnero L, et al. Paraneoplastic neutrophilic figurate erythema. Br J Dermatol 2007; 156:396-8.
[Google Scholar]
|
| 5. |
Khan Durani B, Andrassy K, Hartschuh W. Neutrophilic dermatosis with an erythema gyratum repens-like pattern in systemic lupus erythematosus. Acta Derm Venereol 2005;85:455-6.
[Google Scholar]
|
Fulltext Views
4,931
PDF downloads
1,457





