Translate this page into:
Nevoid acanthosis nigricans: Report of four cases localized to the umbilicus
Corresponding author: Dr. Elizabeth Guevara-Gutiérrez, Monte Olimpo 1413, Colonia Independencia, CP 44340, Guadalajara, Jalisco, México. albtlacuilo@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Reyes-Meza SE, Guevara-Gutiérrez E, Villanueva-Quintero G, Hernández-Arana S, Tlacuilo-Parra A. Nevoid acanthosis nigricans: Report of four cases localized to the umbilicus. Indian J Dermatol Venereol Leprol 2021;87:660-5.
Abstract
Nevoid acanthosis nigricans is a rare, benign form of acanthosis nigricans. Of the 24 cases documented in the literature, only two are exclusively localized to the umbilicus. We present four cases of nevoid acanthosis nigricans localized to the umbilicus; in patients less than 25 years of age, with no known co-morbidities, three of whom were females. Two of the cases received, with good response, treatment based on topical calcipotriol, a medication not previously reported to be used for this indication. Contrary to other types of acanthosis nigricans, the nevoid acanthosis nigricans is not associated with any syndrome, endocrinopathy, obesity, medication, or neoplasia and it can be confused with other pathologies such as epidermal nevus or dermatosis neglecta.
Keywords
Acanthosis nigricans
nevoid
umbilicus
vitamin D analogs
Introduction
Acanthosis nigricans is a mucocutaneous disorder of keratinization that presents as hyperpigmented plaques with a keratotic surface and velvety appearance. Generally, it is distributed symmetrically in the folds of the neck, axillae, and/or groins and is considered a common dermatological manifestation of systemic illnesses or a reaction to certain medications.1,2 On the other hand, nevoid acanthosis nigricans is a rare and benign form of acanthosis nigricans with only 24 cases documented in indexed literature.3-21 Of these, only 2 are localized exclusively to the umbilicus.6,8
Case Reports
Four patients attended the Dermatology Institute of Jalisco, “Dr. José Barba Rubio.” Three of them were females, with a median age of 19 years. The condition was present a while before presentation, with a median evolution time of 2.5 years [Table 1]. All the patients presented with the characteristic features of well- defined hyperpigmented-brownish plaques with verrucous, scaly surface, localized to the umbilicus [Figures 1a, 1b, 1c, 1d (×40)]. In all cases, the lesions were vigorously rubbed with alcohol swab, to test if they could be removed by doing so, and none could be removed. Thereafter, skin biopsies were performed. The histopathology studies in all the four cases showed similar features characterized by the presence of hyperkeratosis, mild and irregular acanthosis and papillomatosis [Figures 2a, 2b, 2c, 2d]. None had any associated symptoms or had received previous treatments. There was no family history of similar dermatosis or other disturbances of keratinization. They were not overweight or obese, and did not have similar lesions elsewhere. A diagnosis of nevoid acanthosis nigricans was established through clinical and histopathological data. Two patients, whose fasting insulin and glucose levels were within normal limits, received treatment with calcipotriol cream (50 μg/g) two times per day for 3 weeks, with remission of the lesions and without relapse at 3 years of follow-up. The other two patients did not agree to having diagnostic tests performed and declined treatment when they were informed about the benign nature of their condition. Figures 3a and 3b illustrates the improvement observed in patient number 2.
| Patient | Sex | Age (years) | Evolution (years) | Treatment |
|---|---|---|---|---|
| 1 | Female | 20 | 5 | None |
| 2 | Female | 22 | 1 | Calcipotriol |
| 3 | Female | 17 | 3 | Calcipotriol |
| 4 | Male | 18 | 2 | None |

- Patient 1 showing a well defined hyperpigmented brownish plaque with verrucous, scaly surface

- Patient 2 showing a well defined brownish plaque with hyperkeratosis areas and exophytic appearance

- Patient 3 showing a verrucous brownish plaque with scaly surface and precise borders

- Patient 4 showing a verrucous brownish plaque with velvety appearance and precise borders
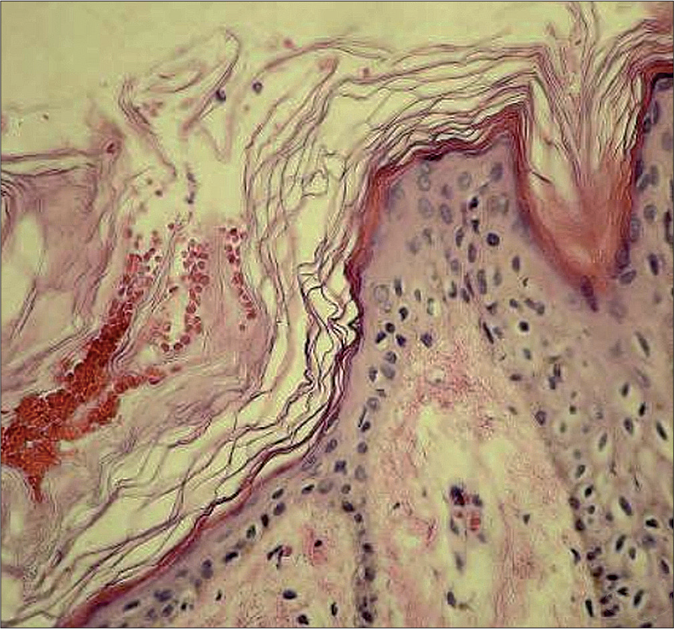
- Histopathology of patient 1 showing hyperkeratosis and papillomatosis (H and E, ×400)
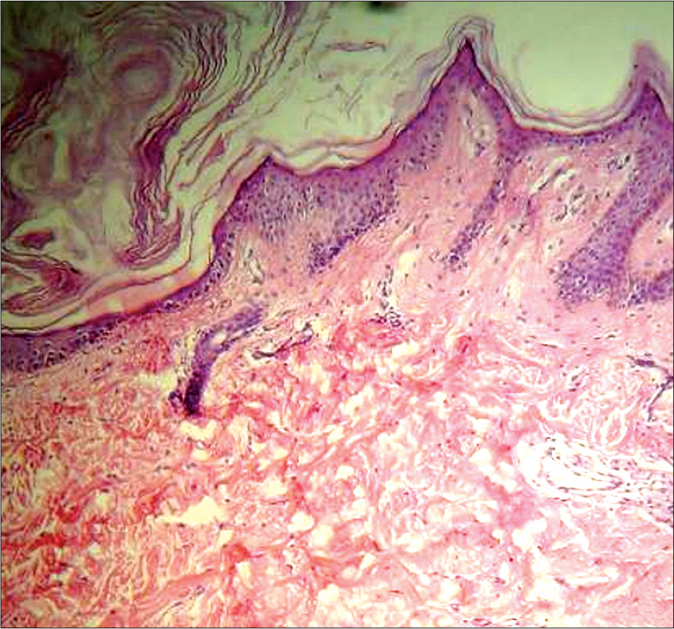
- Histopathology of patient 2 showing hyperkeratosis, mild and irregular acanthosis with papillomatosis (H and E, ×400)
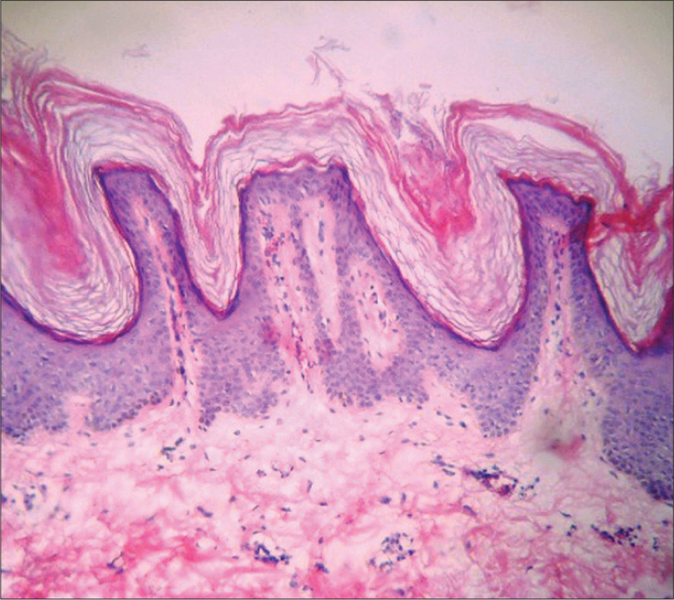
- Histopathology of patient 3 showing hyperkeratosis and papillomatosis alternating with moderate acanthosis, interpapillary valley filled with keratine (H and E, ×400)
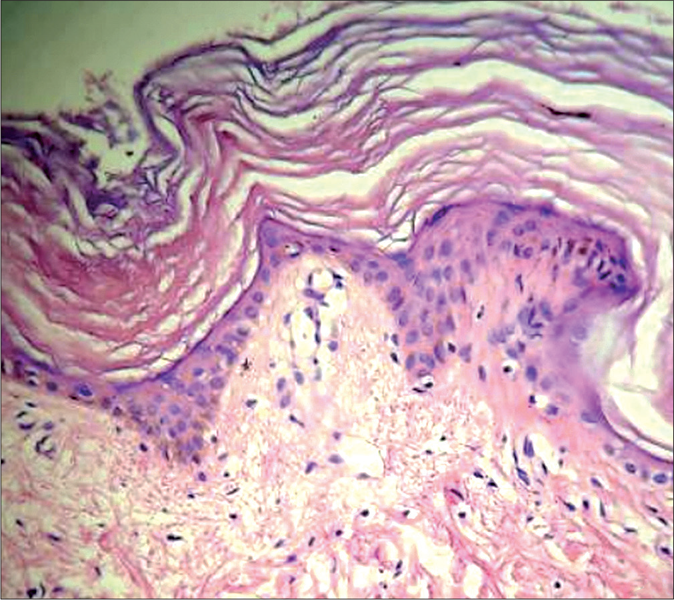
- Histopathology of patient 4 showing hyperkeratosis and mild papillomatosis of the epidermis with scarce lymphocytic infiltrate on the dermis (H and E, ×400)

- Brownish hyperkeratotic and exophytic plaque localized to the umbilicus of patient 2 (×40)

- Clinical image showing clearance of the lesion after three weeks of treatment with topical calcipotriol (×40)
Discussion
Nevoid acanthosis nigricans is a rare and benign form of acanthosis nigricans that can present during infancy or puberty.3-21 It was first described in 1976 by Curth.3 Since that description, there have been 23 cases published.4-21
Nevoid acanthosis nigricans presents slightly more often in males, is localized to bodily areas that differ from the classic acanthosis nigricans, is generally unilateral, and is distributed in segmental form or follow Blaschko’s lines. In published cases, the most frequent localization reported is in the trunk, in 79% cases, followed by extremities in 13%, and the head in 8% cases.3-21 Only two (8%) of the reported cases are localized exclusively to the umbilicus6,8 [Table 2].
| Case | Years | Sex age | Evolution (years) | Localization | Associations | Treatment | Result |
|---|---|---|---|---|---|---|---|
| 1 | 19763 | Male 32 | Puberty | Abdomen | Epidermal nevus Parotid cancer | Not specified | Not specified |
| 2 | 199114 | Male 17 | 4 | Abdomen and umbilicus | None | Not specified | Not specified |
| 3 | 20039 | Female 18 | 4 | Abdomen and umbilicus | None | Not specified | Not specified |
| 4 | 20058 | Female 18 | 2 | Umbilicus | None | Tretinoin 0.1% | Excellent |
| 5 | 20066 | Female 16 | 4 | Umbilicus | None | Minocycline and adapalene 0.1% | Improvement |
| 6 | 200612 | Female 18 | 12 | Clavicular region | Hashimoto thyroiditis | Topical tretinoin 0.025% | No improvement |
| 7 | 200612 | Female 16 | Childhood | Thigh | Amenorrhea, obesity, classical acanthosis nigricans | Not specified | Not specified |
| 8 | 200612 | Male 7 | 4 | Back | None | Not specified | Not specified |
| 9 | 200612 | Male 28 | 2 | Pectoral region | None | Not specified | Not specified |
| 10 | 200810 | Female 18 | 7 | Nape, retroauricular region | None | Not specified | Not specified |
| 11 | 200815 | Male 8 | 6 | Axillary region | None | Ammonium lactate 12% | Mild improvement |
| 12 | 201011 | Male 28 | 6 | Sternal and pectoral region | Neurofibromatosis | Not specified | Not specified |
| 13 | 20114 | Female 19 | 3 | Sternal and submammary region | None | Tretinoin 0.025% | Improvement |
| 14 | 20127 | Female 29 | 14 | Shoulder and arm | None | Tretinoin, corticosteroids, hydroquinone | No improvement |
| 15 | 20127 | Male 18 | 1.5 | Scapular region | None | Not specified | Not specified |
| 16 | 20127 | Male 6 | 2 | Auricular tragus | None | Not specified | Not specified |
| 17 | 201316 | Female 40 | 25 | Leg | None | Not specified | Not specified |
| 18 | 201417 | Male 25 | 8 | Pectoral region | None | Retinoids | Not specified |
| 19 | 201418 | Male 40 | 25 | Axillary and pectoral region | None | Keratolitic, retinoid, corticosteroid | No improvement |
| 20 | 201419 | Female 23 | 9 | Axillary region | None | Laser CO2 | Improvement |
| 21 | 201413 | Male 12 | 6 | Scapular region | None | Tretinoin | No improvement |
| 22 | 201520 | Male 18 | 3 | Axillary and pectoral region | None | Tretinoin 0.05% | Not specified |
| 23 | 20155 | Male 17 | 0.25 | Abdomen | None | Tretinoin 0.05% | Improvement |
| 24 | 201621 | Female 9 | 4 | Scapular region | None | Laser CO2 | Very satisfactory |
From the morphological point of view, though it presents as a hyperpigmented and well-defined velvety-surfaced plaque, its distribution is nevoid.8 The other names that it has been given are -rounded and velvety epidermal nevus,7,18,19 linear acanthosis nigricans,16 unilateral nevoid acanthosis nigricans,4,11,14,17,20,21 or acanthosis nigricans similar to epidermal nevus.3,12
Its clinical course is unpredictable as it can have a short period of activity, to later maintain stability, or it can regress.3,5 Contrary to classical acanthosis nigricans,1,2 nevoid acanthosis nigricans is not associated with insulin resistance, diabetes mellitus type 2, obesity; internal malignant neoplasia, or endocrine diseases.4-10,13-21 In 2006, Ersoy-Evans et al. published four cases of nevoid acanthosis nigricans where one was associated with obesity and amenorrhea, but since the patient also had classical and bilateral acanthosis nigricans lesions; we consider that the said associations were not related to nevoid acanthosis nigricans but rather to the classical acanthosis nigricans.12 Other associations include epidermal nevus,3 neurofibromatosis,11 and Hashimoto thyroiditis,12 although a causal relationship has not been demonstrated between them, and the majority of the published casesdo not refer to any association with systemic illnesses.4-10,13-21
The histopathological features of nevoid acanthosis nigricans do not vary from the classical form; characterized by hyperkeratosis, papillomatosis, mild and irregular acanthosis in the epidermis, with mild perivascular mononuclear inflammatory infiltrate in the superior dermis.3-21 In some cases, hyperpigmentation of the basal layer has been reported.10,13-15,17-19
The differential diagnoses that have been mentioned in published cases include the epidermal nevus,5,6,11,12,16-20 confluent and reticulated papillomatosis,6,12,17 Dowling– Degos disease,6 and seborrheic keratosis.17,18 To this list, we would add dermatosis neglecta and psoriasis [Table 3].22-26
| Diagnosis | Age | Localization | Morphology | Histopathology | Associations |
|---|---|---|---|---|---|
| Epidermal nevus22 | Birth or infancy | Any site including oral mucosa and ocular conjunctiva | Linear plaque yellow-brown velvety or verrucous, well-defined | Hyperkeratosis, acanthosis, papillomatosis. Can observe nests of nevoid cells. Increase in keratohyalin granules in the corneal stratum. Hyperpigmentation of the basal membrane. | One-third have involvement of other organ systems |
| Confluent and reticulated papillomatosis23 | 8-32 years | Bilateral superior trunk (primarily the submammary and intermammary region) | Hyperpigmented reticulated plaques, brown-colored, velvety appearance | Hyperkeratosis in wavy, web form, papillomatosis, focal acanthosis, increased melanin in the basal layer | None |
| Dowling-Degos disease24 | Adult onset (<24 years) but can occur in infancy | Areas of flexion: axillae, groin, submammary folds, and neck | Mottled and reticular pigmentation, lesions similar to comedones and pointed scars | Elongation of the interpapillary crests, thinning of the suprapapillary epithelium, hyperpigmentation of the basal layer in filiform pattern. In dermis, lymphohistocytic perivascular infiltrate. | Hydradenitis suppurativa; multiple keratoacanthomas, epidermal, cysts and seborrheic keratosis; and perianal squamous cell carcinoma |
| Seborrheic keratosis25 | Adults (>50 years) | Usually in areas exposed to sunlight (63.1%) | Brownish plaques slightly elevated, well-demarcated with follicular plugs | Hyperkeratosis, acanthosis, papillomatosis, corneo pseudocysts | Premalignant and malignant lesions (24.2%), primarily of seborrheic keratosis in light-exposed areas |
| Dermatosis neglecta26 | Any age (patients with some disability or chronic illness) | Any area, above all where there was hyperesthesia, previous trauma, pain, or immobility | Unique plaque, hyperpigmented, verrucous that disappears after cleaning or scrubbing the skin | Does not require histopathological study, but when performed can present yeast periodic acid-Schiff positives | None |
| Nevoid acanthosis nigricans3-21 | Infancy or puberty | Any localization, primarily trunk (79%) | Plaque nevoid in appearance, hyperpigmented, velvety surface | Hyperkeratosis, papillomatosis, mild acanthosis. In dermis, mild perivascular mononuclear inflammatory infiltrate. | None in the majority of cases (87.5%) |
Clinically, psoriasis could be ruled out on the basis of the following features: 1) patients do not present with lesions in other areas and 2) the lesions are not erythematous plaques with desquamation on the surface. It is well-known that the umbilicus is a habitual localization for psoriasis, but, being a cutaneous fold, the lesions tend to be more erythematous and less desquamative, or in fact do not present scales.27 In a Medline search using the key words “psoriasis,” “localised,” “nevoid,” and “special localisation,” we did not find descriptions of psoriasis with exclusive localization to the umbilicus.
Histological features, especially the lack of granular layer and regular papillomatosis could point toward psoriasis. However, these findings are non-specific and can also be present in nevoid acanthosis nigricans and other pathologies such as confluent and reticulated papillomatosis of Gougerot and Carteaud.23 Moreover, our cases lack findings that are observed in 90% of patients with psoriasis (parakeratosis, dermal perivascular lymphocytic inflammatory infiltrate) or in more than 50% of them (Kogoj’s spongiform pustules and Munro micro abscesses).28
Due to the rarity of nevoid acanthosis nigricans, there is no existing consensus for treatment and the results have been variable [Table 2]. We decided to initiate treatment with vitamin D analogs, specifically topical calcipotriol (22-ene-26,27-dehydro1α,25(OH) 2D3), for two reasons: a) for its mechanism of action on keratinocytes:in vitro studies have demonstrated that once vitamin D analogs bind to the intracellular receptor of vitamin D, they act as transcription factors modulating the expression of various genes involved in epidermal proliferation, inflammation, and keratinization.29 In other words, calcipotriol promotes the differentiation of keratinocytes through molecules such as involucrin and transglutaminase-1 and inhibits epidermal proliferation,30 b) For the favorable response observed in patients with nevoid hyperkeratosis of the nipple and areola when treated with calcipotriol31 or with another vitamin D analog, the calcitriol.32 These are the characteristics of the medication explaining the favorable response to treatment in two of the cases mentioned in the present case report, although this response needs to be confirmed in a greater number of cases.
We report these four patients with nevoid acanthosis nigricans localized to the umbilicus with the aim of familiarizing dermatologists with the clinical characteristics of nevoid acanthosis nigricans, help differentiate it from classical acanthosis nigricans and from other clinical and histopathological differential diagnoses and to consider it among the dermatoses localized to the umbilicus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Current treatment options for acanthosis nigricans. Clin Cosmet Investig Dermatol. 2018;11:407-13.
- [CrossRef] [Google Scholar]
- Acanthosis nigricans: A fold (intertriginous) dermatosis. Clin Dermatol. 2015;33:466-70.
- [CrossRef] [Google Scholar]
- Unilateral epidermal naevus resembling acanthosis nigricans. Br J Dermatol. 1976;95:433-6.
- [CrossRef] [Google Scholar]
- Unilateral nevoid acanthosis nigricans with a submammary location. Ann Dermatol. 2011;23:95-7.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans: A rare case with late onset. Our Dermatol Online. 2015;6:337-8.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans localized to the umbilicus. J Dermatol. 2006;33:433-4.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans or RAVEN (rounded and velvety epidermal nevus): Three cases. Ann Dermatol Venereol. 2012;139:183-8.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans localized to the umbilicus: Successful treatment with topical tretinoin. Ann Dermatol. 2005;17:24-6.
- [CrossRef] [Google Scholar]
- A case of nevoid acanthosis nigricans. Acta Derm Venereol. 2004;84:234-5.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans. Indian J Dermatol Venereol Leprol. 2008;74:279-80.
- [CrossRef] [Google Scholar]
- Unilateral nevoid acanthosis nigricans and neurofibromatosis 1: An unusual association. Indian J Dermatol Venereol Leprol. 2010;76:715-7.
- [CrossRef] [Google Scholar]
- The acanthosis nigricans form of epidermal nevus. J Am Acad Dermatol. 2006;55:696-8.
- [CrossRef] [Google Scholar]
- Nevoid acanthosis nigricans with subtle melanocyte hyperplasia. J Am Acad Dermatol. 2008;58:S102-3.
- [Google Scholar]
- Unilateral nevoid acanthosis nigricans: Uncommon variant of a common disease. Indian Dermatol Online J. 2014;5:S40-3.
- [Google Scholar]
- RAVEN: forma particular de nevo epidérmico, Primer caso argentino. Dermatol Argent. 2014;20:268-70.
- [Google Scholar]
- Rounded and velvety epidermal naevus, report of a verrucous form in axillary location. BMJ Case Rep. 2014;2014:bcr2014204611.
- [Google Scholar]
- Unilateral nevoid acanthosis nigricans treated with CO2 laser. BMJ Case Rep. 2016;2016:bcr2016216073.
- [Google Scholar]
- Confluent and reticulated papillomatosis: Diagnostic and treatment challenges. Clin Cosmet Investig Dermatol. 2016;9:217-23.
- [CrossRef] [Google Scholar]
- Clinical and histopathological investigation of seborrheic keratosis. Ann Dermatol. 2016;28:152-8.
- [CrossRef] [Google Scholar]
- Clinical analysis of 48 cases of inverse psoriasis: A hospital-based study. Eur J Dermatol. 2005;15:176-8.
- [Google Scholar]
- Histopathological findings are associated with the clinical types of psoriasis but not with the corresponding lesional psoriasis severity index. Ann Dermatol. 2015;27:26-31.
- [CrossRef] [Google Scholar]
- Effects of a novel vitamin D analogue MC903 on cell proliferation and differentiation in vitro and on calcium metabolism in vivo. Biochem Pharmacol. 1988;37:889-95.
- [CrossRef] [Google Scholar]
- Nevoid hyperkeratosis of the nipple and areola: Treatment of two patients with topical calcipotriol. J Am Acad Dermatol. 2002;46:131-3.
- [CrossRef] [Google Scholar]
- Unilateral nevoid hyperkeratosis of the nipple and areola treated with topical calcitriol. Actas Dermosifiliogr. 2008;99:500-1.
- [CrossRef] [Google Scholar]






