Translate this page into:
Newer and upcoming therapies for melasma
Correspondence Address:
Rashmi Sarkar
Department of Dermatology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi-110002
India
| How to cite this article: Sarkar R, Chugh S, Garg VK. Newer and upcoming therapies for melasma. Indian J Dermatol Venereol Leprol 2012;78:417-428 |
Abstract
Melasma is one of the most common and distressing pigmentary disorders presenting to dermatology clinics. The precise cause of melasma remains unknown; however, there are many possible contributing factors. It is notably difficult to treat and has a tendency to relapse. The existing and most tried topical therapy is hydroquinone and the triple combination with tretinoin and corticosteroids, which is considered the gold standard for melasma. Besides that, azelaic acid, kojic acid, arbutin, ascorbic acid, glycolic acid and salicylic peels have also been tried with limited success. However, multiple novel topical agents are being investigated for their potential as hypopigmenting agents with unique mode of action. But, further trials are required to study their efficacy and safety before they can be further recommended. The article highlights these newer formulations and also briefly mentions about the newer chemical peels and the much hyped lasers in treating this difficult and frustrating condition.Introduction
Melasma is the most common pigmentary disorder among Asians. It is commoner in women, especially in their reproductive years, but about 10% cases occur in men. In an Indian study by Sarkar et al, melasma in men was seen in 20.5% patients and was clinically and histopathologically similar to melasma in females. [1] Different therapeutic modalities, especially the gold standard hydroquinone have been used in the treatment of melasma. However, the disorder is difficult to treat, particularly in dark-skinned individuals. The existing modalities which are used include hydroquinone, retinoic acid, kojic acid, azelaic acid, and peeling agents like glycolic, trichloroacetic acid, salicylic and lactic acid. Physical agents like lasers and dermabrasion have also been tried with limited success.
These modalities have their inherent side effects, especially on prolonged usage, have limited efficacy and more often than not, the condition relapses on discontinuation of therapy. As there is no perfectly satisfactory agent for melasma, research is ongoing to develop newer, safer and innovative treatment for treating this psychosocial disorder, causing profound cosmetic disfigurement, significant stress and embarrassment to the patient. [2],[3]
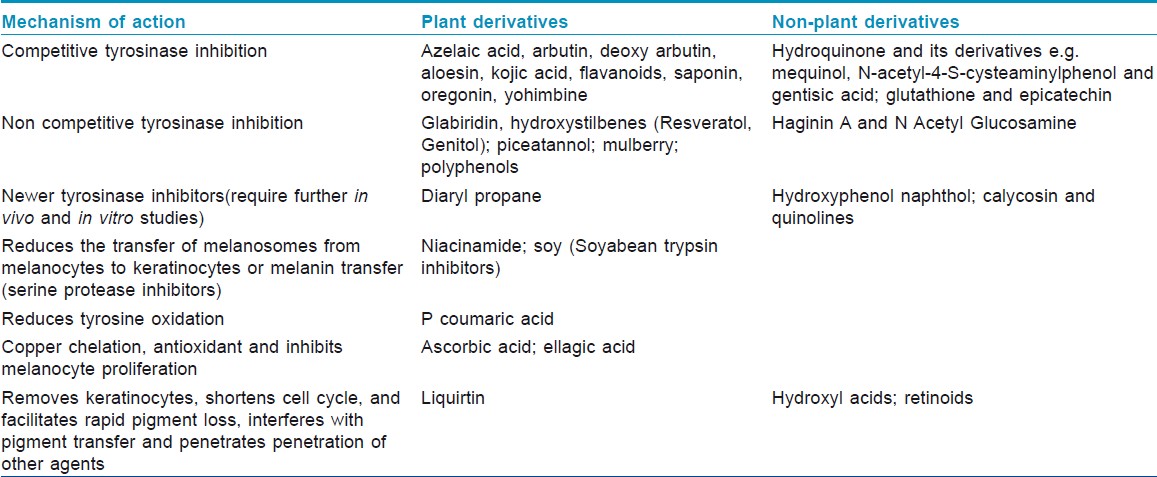
This article focuses on newer and experimental agents, which could potentially be used as treatment for melasma. Although many of them are still in the experimental /research trial phase, they are being discussed because they could offer a ray of hope in the future. These agents have been classified according to the basis of the origin of the pharmacological compounds [Table - 1]. However, for the purpose of discussion, they can be clubbed based on their mechanism of action as tyrosinase inhibitors, those which inhibit transfer of melanosomes, melanocytotoxic agents and antioxidants [Table - 1].
A number of synthetic and botanical compounds derived from natural sources, which are being investigated for their potential role in reducing melanin production and pigmentation, are also discussed in the article. Although experimental evidence suggests their possible benefits, dependable controlled trials are mostly lacking. Some of the compounds are formulated in combination products and marketed by pharmaceutical companies while others are available as ingredients of over-the-counter preparations. The therapies currently used for melasma are mainly topical; however, supplemental role of systemic agents is also highlighted in this article. The article ends with the discussion of newer physical modalities, especially useful in patients, resistant or intolerant to topical therapy. The newer peels and lasers albeit costly may prove to be efficacious even in dark-skinned patients besides having the merit of avoiding regular and long term application, and thereby avoid the side effects of long term continuous topical therapy. There has been enormous ongoing research for deciphering newer therapeutic modalities for melasma, but there is still a long way to go.
Newer and Experimental Agents
Aloesin is a C glycosylated chromone, derived from aloe vera and has been proven to competitively inhibit hydroxylation of tyrosinase to DOPA and oxidation of DOPA to dopachrome. Although there are no human studies on melasma, it has been demonstrated that aloesin modulates melanogenesis in dose-dependent manner via competitive inhibition of tyrosinase in vitro[4] and in pigmented skin equivalents [5] using enzyme kinetics on human melanocyte cell lysates. Choi et al studied the inhibitory effect of aloesin on human volunteers in a randomized comparative trial where the subjects were UV irradiated (210 mJ) on volar forearm and were divided into 4 groups: vehicle control, aloesin-treated, arbutin-treated and aloesin and arbutin-treated. Aloesin and/or arbutin were administered 4 times a day for 15 days. The results revealed that aloesin suppressed pigmentation by 34%, arbutin by 43.5%, and the co-treatment by 63.3%, compared with the control (N = 15; P < 0.05) and in a dose-dependent manner. [6] Hence, aloesin is a potential therapeutic agent in melasma and is being currently used in several over-the-counter cosmeceutical combinations.
Flavanoids: These are benzopyrene derivatives, which can be classified into flavones, flavanols, isoflavones, flavanones and anthocyanidins. They have the advantage of formulation into nanocapsules so that they are protected until they reach an active site of melanin synthesis where they exert a powerful reducing action, have antiradical activity, and act as a substrate competitor for the tyrosinases. An in vitro comparative study of this bioflavonoid factor on skin implants incubated for 15 hours with L-dopa and 0.1% bioflavonoids, control explants, and reference (1% hydroquinone) explants showed that bioflavonoids totally inhibit pigment induced by DOPA oxidation. [7] The depigmentation action of bioflavonoids was supported histopathologically too, and the depigmentation factor of bioflavonoids appeared relatively free from side effects. The citroflavonoids also have antiinflammatory, antiirritant and antiallergic properties.
Ellagic acid: It′s a naturally occurring polyphenol isolated from strawberries, green tea and geranium and acts by dose dependant inhibition of tyrosinase activity in B16 melanoma cells comparable to arbutin. [8] In a study on guinea pigs, ellagic acid prevented UV-induced pigmentation similar to hydroquinone. [9] In a study on guinea pigs, 6 weeks oral intake of ellagic acid was found to produce similar whitening effect as L ascorbic acid. [8] The skin-whitening effect of ellagic acid is probably due to inhibition of the proliferation of melanocytes and melanin synthesis by tyrosinase in melanocytes, without injuring cells. Thus, ellagic acid may be used as an effective whitening agent for the skin without undesirable side effects.
Gentisic acid: It is derived from Gentian roots and is a safe and effective topical skin lightening agent. Its alkyl ester, especially methyl gentisate is highly effective and less cytotoxic than hydroquinone. In a comparative in vitro study by Curto et al, 4 depigmenting agents, namely hydroquinone, kojic acid, arbutin, magnesium ascorbyl phosphate and synthetic esters of gentisic acid were studied for their tyrosinase inhibitory effects where mammalian melanocyte cell cultures and cell-free extracts were used. The study demonstrated that the smaller esters of gentisic acid shared an ability to inhibit melanogenesis without cytotoxicity and mutagenesis. [10]
Hydroxycoumarins: Coumarins are lactones of phenyl propanoic acid with benzopyranone nucleus. The natural derivatives of coumarins include aloesin, which has been proven to have tyrosinase inhibitory properties. The hydroxycoumarins are novel antioxidants, which have alpha tocopherol like structure and strongly inhibit tyrosinase in cultured human melanocytes and cell homogenates, besides having scavenging and quenching activities. [11]
Natural derived botanical extracts: A recent trend is to develop newer natural derived extracts for the purpose of skin lightening. A number of plant-derived products are being studied for their depigmenting role in melasma and other pigmentary disorders. In an in vitro study by Hwang et al, 101 plant extracts were studied for inhibitory effect against tyrosinase, L-dopa oxidation and melanin synthesis in B16 melanoma cells. Of these extracts, Broussonetia kazwoki, B. papyrifera, Cornus officinalis, Rhus javanica and Pinus densiflora inhibited tyrosinase and DOPA oxidation in dose-dependent manner. [12] These botanicals have the advantage of being efficacious, and most importantly, they would be the drugs of choice in future being free from any complications.
Rucinol (4-n butyl resorcinol): It is a phenolic derivative, which inhibits both tyrosinase and tyrosinase related protein. In a prospective, double-blind, randomized, vehicle-controlled, split-face comparative trial, 32 female patients with melasma were treated with rucinol serum 0.3% or vehicle, which was applied twice daily for 12 weeks followed by a 12 week follow-up. After 12 weeks, clinical pigmentation scores were lower than the vehicle-treated site, and the difference was statistically significant (P < 0.027). This preliminary study demonstrated the tolerability and efficacy of rucinol in melasma. [13]
A recent modification of 0.3% serum into 0.1% liposomal cream, which leads to an improved stabilization and enhanced penetration, has been studied to be effective in melasma. In a study by Huh et al, 23 patients with melasma were included in a randomized, double-blind, vehicle-controlled, split-face study with rucinol cream compared to vehicle-applied twice daily for 8 weeks, and significant (P value 0.043) improvement was seen in melanin index with more than 60% patients reporting subjective improvement. [14]
Soy: It is a plant derivative found in tofu products as well as in soyabeans and soy milk. Its primary metabolites genistein and diadzein have the active ingredients STI (Soy Trypsin Inhibitor) and Bowman Birk Inhibitor (BBI), which act by inhibiting melanosome transfer to keratinocytes and also have antioxidant properties. Wall et al conducted a parallel, randomized, double-blind, vehicle-controlled study with 65 female patients with mottled pigmentation where the preparation was applied twice daily for 12 weeks. There was a significant improvement (P < 0.005) in pigmentation, skin tone and texture in the treated group. [15] Hence, although not used in melasma, it could be a promising agent.
Silymarin: It′s a naturally occurring polyphenol flavanoid compound or flavolignans, derived from thistle plant Silybium marinum, which has been found to have inhibitory effects on melanogenesis in mouse melanocyte cell lines. [16] However, the human studies for role in melasma are lacking.
Alphalipoic acid / thioctic acid / dihydrolipoic acid: It′s a disulphide derivative of octanoic acid and is known as a universal antioxidant for it is both fat and water-soluble, and thus acts in both lipid cell membrane and aqueous compartment of melanocytes. The newer combination product with zinc that is sodium zinc dihydrolipoyl histidinate has been studied by Tsuji Naito et al on B16 melanoma cells and found to inhibit dopachrome formation. [17] It may thus act as a novel skin lightening agent for melasma, provided human trials are undertaken.
Dioic acid: It belongs to the dicarboxylic acid group, which have 2 carboxylic acid with carbon atoms ranging from 2 to 24. Octadenedioic acid, a monounsaturated dicarboxylic acid, derived from oleic acid, acts as agonist to nuclear PPAR, which regulates tyrosinase transcription and melanosome transfer. A study by Tirado-Sanchez et al on 96 Mexican female patients with melasma showed that dioic acid is an effective and highly tolerated skin product for melasma. It was an open, comparative, 12 week trial in which Melasma Activity Scoring Index (MASI) scores were compared between patients applying dioic acid twice and 2% hydroquinone cream twice daily. Although the difference in efficacy or side effects was not found to be significant (P value 0.287) between the 2 groups, the pre and post-treatment (after 12 weeks) difference in MASI scoring was significant (P value 0.001). [18]
Green tea: This most popular beverage has green tea phenols (EGCG, epigallocatechin, catechin, gallocatechin gallate and epicatechin gallate) of which, the most important and pharmacologically most potent is epigallocatechin gallate (EGCG), which has been demonstrated to modulate melanin production in dose-dependent manner and also posses antiinflammatory properties. [19] Dong et al studied the mechanism of action of EGCG on Mel Ab cells in vitro and found that it downregulates MITF and tyrosinase production. [20] However, the studies of green tea phenols in human beings are limited because of stability and penetration issues.
Octadecenedioic acid ( oda0 ): is a dicarboxylic acid with structural similarity to azelaic acid. Its skin whitening effects are mediated not by inhibition of tyrosinase but by the stimulation of PPARs, which are nuclear receptors modulating synthesis of tyrosinase mRNA. [21] ODAs have been studied in vivo in a clinical comparative study on 21 Chinese volunteers where 1% ODA cream was applied on forearm for 8 weeks with a further follow-up of 4 weeks and compared to an application of 2% arbutin applied on the other forearm. [22] The assessment was done by chromometric and mexametric analysis at baseline and every 2 weeks for 12 weeks where the melanin index decreased by 21.2% in 76% volunteers, and there was lightening effect in 90% individuals by upto 11%. Thus, ODAs are a future ray of hope for cosmetic formulations for melasma. Its main advantages are its flexibility in formulations over a broad pH range.
Orchid extracts: Tadokoro et al conducted a double-blind, comparative, split-face, prospective trial on 48 female patients with melasma and/ or lentigines to assess an in vivo efficacy of a cosmetic formulation containing orchid extracts, compared to 3% vitamin C derivative. The patients applied the orchid extracts cream formulation and 3% vitamin C formulation on either side of the face for 8 weeks, and the efficacy was evaluated clinically by colorimetric measurements and subjectively using a questionnaire, which showed improvement with both modalities. [23] Thus, the study highlighted that the orchid-rich plant extracts possess efficacy, similar to vitamin C derivative in whitening melasma and lentigines.
Mequinol / 4 hydroxy anisole: It is a derivative of hydroquinone, which is a more effective competitor of tyrosinase and has lesser side effects. In a pilot, small case series of 5 men with melasma by Keeling et al, the topical solution of 2% mequinol and 0.01% tretinoin was applied twice daily for 12 weeks and patients followed for 16 weeks. Complete clearance was noted in 4 patients, and moderate improvement was noted in single patient, and the results were maintained at follow-up 4 weeks after discontinuation of drug. The drug was well-tolerated however, the study size was small. [24]
Linoleic acid: It is an unsaturated, 18 carbon fatty acid, derived from hydroxylated botanical oils e.g. safflower. It is known to accelerate tyrosinase degradation and accelerates turnover of stratum corneum. Lincomycin is a lincosamide antibiotic, produced by actinomycete streptomyces lincolensis, which inhibits melanogenesis post-transcriptionally. The efficacy of these drugs is proven in in vitro studies. In a study by Lee et al, it was observed that 2% lincomycin mixed with 0.05% betamethasone valerate and 2% linoleic acid caused significant improvement in pigmentation (P < 0.05) in 47 patients with melasma in a 6 week, double-blind, randomized-controlled trial as compared to vehicle or lincomycin with betamethasone, with the formulations to be applied every night for 6 weeks. MASI scoring and objective assessment was done every 2 weeks. [25] Newer liposomal formulation of linoleic acid (0.1%) ensures more solubility in an aqueous solution, and thereby, enhanced efficacy at lower concentration possibly by enhanced penetration of linoleic acid into melanocytes. [26]
Magnolignan (2,2`-Dihyroxy 5,5` dipropyl biphenyl): It is a phenolic derivative, which decreases maturation of tyrosinase and accelerates its degradation as revealed by Western Blot assays, pulse labeling and immunoprecipitation studies. [27] Its cream formulation (0.5%) was studied by Takeda et al on 51 female patients with melasma in an open study for 6 months, which showed significant subjective improvement and improvement in MASI scores in pigmented areas (P value < 0.05) without any side effects. [28] A double-blind, randomized, comparative, clinical trial was conducted on 43 subjects to assess the effect of magnolignan on UV- induced pigmentation, which showed significant decrease in the pigmentation scores after 3 weeks of application of 0.5% magnolignan cream versus placebo and no serious side effects. [29]
Tranexamic acid: (Trans-4 (aminomethyl) cyclohexane carboxylic acid): It is a lysine analogue, known to have antiplasmin activity and hence decreases alpha-MSH, which stimulates melanin synthesis. In an open study by Lee et al on 100 Korean women with melasma, tranexamic acid given intradermally (4 mg/ml) every week for 12 weeks caused significant decrease in MASI score (P value < 0.05), and 76.5% subjects reported lightening of melasma with minimal side effects. [30] Tranexamic acid is temperature-stable, not UV sensitive and does not get oxidized easily. Thus, it acts as an ideal choice for composition in skin lightening creams. The newer topical preparation of tranexamic acid cetyl ester HCl is available in cosmetic formulations. Fox did a clinical trial on 25 melasma patients in which tranexamic acid emulsion was applied for 5 to 18 weeks, and 80% subjects reported marked subjective improvement within 8 weeks without any significant side effects. [31]
Cinnamic acid: It is a phenylpropanoid derivative, occurring in plants of cassia and ginseng, which inhibits tyrosinase activity as studied on human and guinea pig melanocytes. [32] In an in vitro study on human and guinea pig melanocytes (Melan A), treatment with 100 ppm of cinnamic acid resulted in significant reduction in melanin production by an inhibitory effect on tyrosinase activity and reduced tyrosinase expression in Melan A cells. [32] In a study by Tan et al, cinnamic acid (2 mmol/L; 0.5 mmol/L) showed tyrosinase inhibitory activity, which was significantly higher than hydroquinone (0.5 mmol/L). [33]
A novel formulation pyronyl acrylic acid esters 3a-i, which shares the structural features of kojic acid and hydroxylated cinnamic acid, was studied in an in vitro study by Kang et al for its inhibitory action on tyrosinase enzyme and was found to be more efficacious than kojic acid. [34]
Pidobenzone /k5 lipogel/ L- proline 5-oxo-4-hydroxyphenyl ester: It is a proline analogue with a benzene ring structure. In a prospective trial by Zanieri et al. on melasma patients, topical treatment with pidobenzone 4% applied twice daily for 16 weeks caused reduction in MASI scores by at least 50% in as many as 70% patients. [35] The side effects were also minimal. Thus, pidobenzone may serve as a useful, reliable and safe treatment for this relapsing resistant condition.
Novel Combination Topical Preparations
A combination, which has been studied in a randomized, double-blind, comparative trial with 80 patients of mixed ethnicities with facial dyschromias, was that of kojic acid, emblica extract and glycolic acid. This formulation and 4% hydroquinone cream were applied in 2 groups of patients twice daily for 12 weeks. The study revealed no statistical difference between both sides (P value < 0.05) though the side effect profile was better with the novel formulation. [36]
Another combination formulation containing hydroquinone, hyaluronic acid and glycolic acid was studied by Guevara et al in an open trial in 15 Latin American women with melasma, with twice daily application of the cream for 12 weeks. [37] The results revealed significant decrease in MASI scores of 64% patients, and mexametry showed an improvement in 93% patients. Mild irritation was recorded in 53% patients.
Agents Acting At Molecular And Dna Levels
The quest of finding newer depigmenting agents for melasma has shifted to the molecular and DNA level. Antisense oligonucleotides (ASOs), which modulate the synthesis of key enzymes of melanogenesis, namely tyrosinase, TRP1 and TRP2 by interacting with targeted mRNA at translational level, have also been investigated for their in vivo and in vitro depigmenting effects. [38] A study conducted by Lazou et al demonstrated that ASOs, which modulate the synthesis of TRP1/Phosphokinase C Beta, lead to skin whitening effect. In vitro, there was a reduction in the reaction rate and decreased enzyme activity of DOPA oxidase. A randomized-controlled trial was conducted on 30 Asian women with pigmented spots, and the formulation was applied twice daily for 8 weeks on pigmented and non-pigmented skin, which showed the lightening effect produced by the formulation to be significant (P < 0.05) in both the pigmented and non-pigmented skin as assessed by objective parameters. [38] Thus, these antisense nucleotides are a new generation of active cosmetic ingredients with safety and stability, which can be utilized in melasma.
Oral Agents
Oral antioxidants
In a randomized, double bind, placebo-controlled trial, a combination of oral proanthocyanidin plus vitamin A, C, and E was assessed in 60 Phillipino females with bilateral epidermal melasma. The antioxidants were taken twice daily for 8 weeks and were compared with placebo intake by mexametric and MASI score analysis. [39] There was significant reduction in MASI scores (P = 0.001)) and pigmentation by mexametry (P value < 0.0001) in malar regions. The combination was also well-tolerated.
Pycnogenol, a standardized plant extract, obtained from the bark of the French maritime pine Pinus pinaster, has evoked great interest in the management of melasma. Between 65% and 75% of pycnogenol are procyanidins, comprising of catechin and epicatechin subunits with varying chain lengths. It also has polyphenolic monomers, phenolic or cinnamic acids and their glycosides. Its main advantage lies in the high bioavailability, synergistic action of its constituents and low incidence of side effects on oral intake. It also has antioxidant and antiinflammatory properties as it doubles the intracellular synthesis of anti-oxidative enzymes and scavenges free radicals due to the aromatic rings bearing one or more hydroxyl groups. It also causes regeneration and protection of vitamin C and E.
A clinical study on efficacy of pycnogenol in 30 melasma patients by Ni et al showed a decrease in pigmentary intensity (P < 0.001) and melasma area index (P < 0.001) with 75 mg daily oral intake (25 mg 3 times a day) of pycnogenol for a total of 30 days in 80% of the patients. [40] No side effect was observed, and blood and urinary parameters were within normal range. Moreover, several other associated symptoms such as fatigue, constipation, pains in the body and anxiety also improved.
Oral agents used topically
Among the oral antioxidants, ascorbic acid is well-known for its efficacy as depigmenting agent. However, due to the unstable nature of vitamin C (rapid oxidation in aqueous solutions on topical application), a formulation containing 25% L ascorbic acid and chemical penetration enhancer was evaluated for efficacy and stability in melasma patients. [41] 40 patients were treated in an open, uncontrolled trial with a commercial preparation applied topically for 16 weeks, and patients were assessed every 4 weeks using MASI and mexameter scoring There was significant decrease (P < 0.05) in the degree of pigmentation by both parameters, and also an improved quality of life was noted with decrease in melasQOL scores.
Zinc is another oral antioxidant, antiinflammatory agent, which has been extensively studied in pigmentary disorders, which has peeling and exfoliating properties and reduces melanin production. Sharquie et al conducted an open clinical trial with 28 patients of melasma who applied Zn SO4 cream twice daily for 8 weeks and were followed for MASI scoring every 2 weeks till 3 months after stopping the treatment. There was 49.78% improvement in the mean MASI scores (P < 0.005), which was maintained at even 3 month follow-up visit. No side effects were noted, except mild burning sensation in few patients. [42] Thus, zinc might serve as a new, effective, safe, non-costly formulation for melasma with long-lasting effects.
Chemical Peels
The main advantage of chemical peels lies in the fact that they can be tailored for use according to the needs of the patient and can be used synergistically with other in-office procedures and topical creams to achieve synergistic effects.
Chemical peels for treating melasma may be superficial or medium depth peels.
Alpha and beta hydroxy peels like glycolic, salicylic, Jessner′s, TCA, azelaic acid peels have been studied extensively for their therapeutic benefits in resistant melasma. Deeper peels are generally not used for melasma as they are associated with complications e.g. hypopigmentation and hyperpigmentation, scarring, keloid formation, secondary infection, allergic reaction, acneiform eruption, persistent erythema, milia formation and improper healing. The newer peels are being reviewed for their use in resistant cases of melasma.
In a study by Sharquie et al, 12 patients (Fitzpatrick IV) with epidermal melasma were treated with 92% (full strength) lactic acid as a peeling agent, applied every 3 weeks for a total of 2 - 6 sessions and were followed every 3 weeks for a total of 6 months. There was a mean decrease in MASI and photographic assessment, the difference being statistically significant (P < 0.05). No relapse or major side effects were seen at 6 month follow-up. [43]
Lactic acid peels have also been compared with Jessner′s as therapeutic modality on 30 patients with epidermal melasma (Fitzpatrick IV). In a split-face comparative trial, peeling was done on either side with 92% pure lactic acid (full strength) and Jessner′s solution every 3 weeks for 2 - 5 sessions and followed till 6 months after last treatment session. All patients showed marked clinical improvement with significant decrease in MASI on both sides (P < 0.05), but no statistically significant difference in pigmentation between the 2 sides. [44] Thus, lactic acid can be a safe, effective and less costly peeling alternative for melasma.
Pyruvic acid: It is a naturally-derived alpha keto acid, formulated in hydroethanolic vehicle, used in concentration of 40% - 70% as a superficial peeling agent. 20 patients of melasma, photodamage and scarring were treated for 4 sessions of 50% pyruvic acid in an erythemogenic base at 2 weeks intervals. It appeared to be well tolerated when assessed clinically and by noninvasive methods. Further studies would be required with this chemical peel in dark skinned subjects. [45]
Tretinoin peels: In an Indian study, on 10 patients with melasma, 1% tretinoin and 70% glycolic acid peels were applied in a split-spaced study, weekly for 12 weeks, and the patients were assessed by MASI scoring. There was statistically significant difference (P < 0.001) in pre and post MASI scoring on both sides; however, the difference between the 2 sides was not significant. Both the peels were well-tolerated. [46] A recent study by Ghersetich et al, using a modification i.e. 10% tretinoin peel mask on 20 melasma patients, has shown that there was significant improvement (P<0.05) after the peels. [47]
Another new peeling agent is acidified amino acid peels, which are carboxylated acidic amino acids, created by dissolution and acidification of natural amino acids due to their potent antioxidants, tyrosinase inhibitory and exfoliant action and are, therefore, effective against melasma. [48] As they have an alkaline pH (close to physiological pH), they are well-tolerated, especially in patients with dry and sensitive skin. They also offer hydration benefits by virtue of their amino acid group and are well-tolerated by patients. In a single-blind, randomized study, 31 patients with melasma were treated with 12 serial peels every 2 weeks for 6 months. There was significant decrease in MASI scoring (P < 0.05) at 3 and 6 months on both the sides, but the difference between the 2 sides was not significant. The side effect profile of amino acid peels was better than glycolic acid as they were less irritating. [49] In a case report of resistant melasma, amino acid peels used in combination with triple combination topical therapy resulted insatisfactory lightening after single application without any side effects. [48]
Another potential peeling agent, which has been successfully tried in post-acne hyperpigmentation and can be used for melasma in future, is mandelic acid, an aromatic alpha hydroxy acid. Chemically, it is alpha hydroxy benzene acetic acid. It is extracted from bitter almonds and has an advantage of causing less irritation as its large molecular weight causes slow penetration into the skin. [50] It is available in algae extract gel or lotion base in concentration of 2% - 10% in isolation and also in combination with other topical vitamins C and E. Its use as a skincare modality was pioneered by Dr James E. Fulton, and its efficacy, studied in 1100 patients in an open uncontrolled study over 3 years, has shown promising results. It was applied as peeling agent in concentration of 30% - 50% weekly or biweekly and used as a face wash (2%) in patients with melasma. In some patients, a 50% improvement on weekly application of 10% lotion has been reported after a period of 1 month. [51] There was significant sustained effect even in dermal melasma, and no post peel hyperpigmentation was recorded. Its advantage lies in its synergistic effects with lasers and lesser side effects like erythema, crusting thus ensuring better compliance.
Another chemical peel on the horizon is lipohydroxy acid. It is a salicylic acid derivative with an additional fatty acid chain, thereby imparting increased lipophilicity and greater keratolytic effect. It has good penetration throughout the epidermis but less deeply than salicylic acid or glycolic acid. It targets corneosomes and detaches them in the stratum corneum without modifying keratin, resembling normal turn over. Its pH is same as that of skin, hence tolerability is better, and it does not require any neutralization. [52]
Chemical peels have been used alone as well as in combination with lasers and topical therapy to achieve desired synergistic effects in a shorter duration of time even in resistant cases. [53],[54] Lee et al treated 25 patients with recalcitrant facial pigmentation with combination of Jessner′s / TCA peels and Q switched Alexandrite / Pulsed Dye Laser at same session achieving good to excellent results in 63% patients. [54] The peels have also been used in combination with topical ascorbic acid and triple combination in dark-skinned patients to achieve better results and patient satisfaction. [55],[56]
Lasers
They may be the recent treatment of choice only for resistant melasma, especially in fair-skinned patients. Although conventionally lasers were incapacitated because of limited efficacy, higher rates of recurrence and side effects e.g. post inflammatory hyperpigmentation, recently the lasers (especially fractional) have found to be useful even in dark-skinned patients. Of course, cost of therapy is still a big deterrent in routine use of lasers in all cases of melasma, therefore, its use is still reserved only for resistant, recalcitrant cases.
Fractional photothermolysis are the most debated topic regarding therapeutic role of lasers in melasma. Rokhsar conducted a pilot study to assess the efficacy of fractional photothermolysis (1535,1550 nm) on 10 patients with resistant melasma. [57] After 4 - 6 sessions, 60% patients achieved 75% - 100% clearance of pigmentation, and only single patient reported post inflammatory pigmentation (PIH). Since there is no downtime or complications, this modality was further evaluated for treating melasma.
Another clinicohistopathological study by Goldberg et al on 10 patients with epidermal melasma treated with 1550-nm fractional erbium: glass laser every 2 weeks for a total of 4 sessions showed that clinically good improvement occurred in 6 (skin type III) and fair (skin type IV) in rest of 4 subjects. [58] The mechanism of clinical improvement was histopathologically proven to be due to decreased number of melanocytes and relative absence of melanin in surrounding keratinocytes consistent with elimination process.
However, a recent, open interventional prospective study by Lee et al on 25 Asian patients with melasma showed that after receiving 4 monthly sessions of fractional 1550 nm laser, there was significant improvement in mean MASI in 60% patients after 4 weeks of treatment. However, there was relapse in melanin index and MASI scores at 24 week follow-up visit, and 13% patients reported post-inflammatory hyperpigmentation. [59] Thus, fractional lasers although showing initial promise, could not produce sustained results and produced side effects warranting judicious use of laser therapy, hence the results have to be interpreted cautiously.
Resurfacing Lasers
Even fractional CO2 and Q switch Nd Yag laser has been shown to produce improvement in melasma patients. [60],[61] Q switch Nd Yag laser has been compared with topical hydroquinone in a randomized, split-face comparative study, comparing Q switched Nd Yag in combination with hydroquinone (5 sessions at weekly interval) versus hydroquinone alone in 22 Asian patients, with dermal or mixed melasma. Both by colorimetric and MASI scoring (75.9% vs. 24%), there was significant improvement (P < 0.001) on the laser-treated site. But, recurrence occurred in all the patients, and 3 of them even developed mottled hypopigmentation. [62]
The combination of lasers can also be beneficial for enhancing the efficacy and patient satisfaction. Another pilot study showing the efficacy of combination of lasers by Nouri et al showed that in an open trial on 4 patients of pulsed CO 2 followed by Alexandrite laser, all had complete resolution without hyperpigmentation or scarring. [63] This may be explained by destruction of melanocytes by pulsed CO2 and then elimination of dermal melanin by Alexandrite laser.
In an open interventional trial by Wang and Liu, 66% of the 32 patients, treated with combination of Q switched Nd Yag and alexandrite laser, showed more than 90% improvement after 4 - 15 sessions, and none of the patients reported any complications. [64] This study also highlighted that duration (>2 years being more resistant) and color (light brown responding more favorably) of melasma affect the response to therapy.
Not only combination of lasers but also topical therapy in combination with lasers leads to an improved efficacy and sustained effects, as shown by Trelles et al in a randomized, comparative trial on 30 melasma patients who were allocated into 3 groups; first and second group receiving either of the 2 and third group receiving both. The satisfaction index and reduction in MASI was 100% in all the 3 groups at the end of 1 month, but, only in the third group, the results were maintained and MASI scoring at 6 and 12 months was significantly better than either of the 2 groups (P<0.001). [65]
The use of newer antiangiogenic lasers may be explained by the recent etiopathogenetic theory of melasma which emphasizes that melasma occurs due to interaction between cutaneous vasculature and melanocytes. A study by Kim et al has shown raised erythema index, vascular endothelial growth factor levels and histopathologically an increase in number and size of dermal vessels in melasma. [66] In an open study by Lee et al on Asian patients with melasma, clinicopathological efficacy of copper bromide laser was assessed using good objective measurements and immunohistopathological parameters. There was a significant improvement in MASI scores post-treatment, decrease in erythema intensity and reduction in the pre-treatment raised levels of markers of vascularity. [67] Thus, this study has opened new horizons for the potential use of these lasers in patients of melasma with pronounced telengiectasia.
Lastly, a comparative analysis between the 3 modalities for melasma i.e. 4% hydroquinone, 30% TCA peels and frequency doubled Q switched Nd Yag laser was undertaken by Salem et al on 45 female melasma patients with moderate to severe melasma. It was a randomized, comparative study in which the patients (Fitzpatrick IV, V) were treated with either of the modalities for an average of 6 months. The improvement was significantly (P < 0.001) higher in the topically-treated group as compared to the other 2 therapies (peels and lasers, which were not significantly different from each other in terms of efficacy). There was no significant difference in the side effect profile in between the 3. [68] Thus, this study re-emphasizes that conventional hydroquinone therapy or triple combination therapy still remains the most efficacious and cost effective treatment for melasma, especially in dark-skinned patients.
Thus, resurfacing procedures, including chemical peels and lasers, are best used in combination with topical therapy. They should be used with care and caution as they can lead to post-inflammatory hyperpigmentation, esp. in dark-skinned patients. Maximal results are achieved with repetitive, superficial, resurfacing modalities. [69]
The process of pigmentation in melasma is very complex, and more research is required to elucidate the intricacies of pathogenesis, and thereby target newer therapies against this psychologically distressing disorder. The ongoing studies have shown that molecules acting at nuclear or DNA/RNA levels and with unique novel mechanisms (PPARs) can also serve as a new ray of hope for melasma. Newer drugs, which may have better properties like stability in formulations, lesser irritation, fewer side effects, better skin penetration and enhanced potency, will be the answer for the future. They may further be investigated to provide an appropriate therapeutic tool for this frustrating disorder.
| 1. |
Sarkar R, Puri P, Jain RK, Singh A, Desai A. Melasma in men: Aclinical, etiological and histological study. J Eur Acad Dermatol Venereol 2010;24:768-72.
[Google Scholar]
|
| 2. |
Picardo R, Vallejos Q, Feldman SR, Schultz MR, Verma A, Quandt SA, et al. The prevalence of melasma and its association with quality of life among male migrant latino workers. Int J Dermatol 2009;48:22-6.
[Google Scholar]
|
| 3. |
Pawaskar MD, Parikh P, Markowski T, Mc Michael AJ, Feldman SR, Balkrishan R. Melasma and its impact on health related QOL in Hispanic women. J Dermatolog Treat 2007; 18:5-9.
[Google Scholar]
|
| 4. |
Jones K, Hughes J, Hong M, Jia Q, Orndorff S. Modulation of melanogenesis by aloesin: A competitive inhibitor of tyrosinase. Pigment Cell Res 2002;15:335-40.
[Google Scholar]
|
| 5. |
Wang Z, Li X, Yang Z, He X, Tu J, Zhang T. Effects of aloesin on melanogenesis in pigmented skin equivalents. Int J Cosmet Sci 2008;30:121-30.
[Google Scholar]
|
| 6. |
Choi S, Lee SK, Kim JE, Chung MH, Park YI. Aloesin inhibits hyperpigmentation induced by UV radiation. Clin Exp Dermatol 2002;27:513-5.
[Google Scholar]
|
| 7. |
Tiedtke J, Morel J, Marks O. Depigmentation Factor Bioflavonoids - A safe and effective skin lightener based on encapsulated citrus bioflavonoids. Cosmetochem. Available at: http://www.cosmetochem.com. Accessed September 24, 2011.
[Google Scholar]
|
| 8. |
Yoshimura M, Watanabe Y, Kasai K, Yamakoshi J, Koga T. Inhibitory effect of an ellagic acid-rich pomegranate extract on tyrosinase activity and ultraviolet-induced pigmentation. Biosci Biotechnol Biochem 2005;69:2368-73.
[Google Scholar]
|
| 9. |
Shimogaki H, Tanaka Y, Tamai H, Masuda M. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci 2000;22:291-303.
[Google Scholar]
|
| 10. |
Curto EV, Kwong C, Hemersdorfer H, Glatt H, Santis C, Virador V, et al. Inhibitors of mammalian melanocyte tyrosinase: In vitro comparisons of alkyl esters of gentisic acid with other putative inhibitors. Biochem Pharmacol 1999;57:663-72.
[Google Scholar]
|
| 11. |
Yamamura T, Onishi J, Nishiyama T. Antimelanogenic activity of hydrocoumarins in cultured normal human melanocytes by stimulating intracellular glutathione synthesis. Arch Dermatol Res 2002;294:349-54.
[Google Scholar]
|
| 12. |
Hwang JH, Lee BM. Inhibitory effects of plant extracts on tyrosinase, L-DOPA oxidation, and melanin synthesis. J Toxicol Environ Health A 2007;70:393-407.
[Google Scholar]
|
| 13. |
Khemis A, Kaiafa A, Queille Roussel C, Duteil L, Ortonne JP. Evaluation of efficacy and safety of rucinol in patients with melasma: A randomized controlled trial. Br J Dermatol 2007;156:997-1004.
[Google Scholar]
|
| 14. |
Huh SY, Shin JW, Na JI, Huh CH, Yow SW, Park KC. Efficacy and safety of liposomal encapsulated 4-butyl resorcinol 0.1% cream for treatment of melasma: A randomized controlled split face trial. J Dermatol 2010;37:311-5.
[Google Scholar]
|
| 15. |
Wall W, Nebus J, Leyder JJ. Efficacy of soy moisturizer in photoaging: A double blind vehicle controlled 12 week study. J Drugs Dermatol 2007;6:917-22.
[Google Scholar]
|
| 16. |
Choo SJ, Ryoo IJ, Kim YH, Xu GH, Kim WG, Kim KH, et al. Silymarin inhibits melanin synthesis in melanocyte cells. J Pharm Pharmacol 2009;61:663-7.
[Google Scholar]
|
| 17. |
Tsuji Naito K, Hatani K, Okada K. Modulating effects of a novel skin-lightening agent, alpha-lipoic acid derivative, on melanin production by the formation of DOPA conjugate products. Bioorg Med Chem 2007;15:1965-75.
[Google Scholar]
|
| 18. |
Tirado-Sanchez A, Santamaria Roman A, Ponce Olivera RM. Efficacy of dioic acid compared with hydroquinone in treatment of melasma. Int J Dermatol 2009;48:893-5.
[Google Scholar]
|
| 19. |
Sato K, Toriyama M. Depigmenting effect of catechins. molecules 2009;14:4425-32.
[Google Scholar]
|
| 20. |
Kim DS, Park SH, Kwon SB, Li K, Youn SW, Park KC. Epigallocatechin-3-gallate and Hinokitiol reduce melanin synthesis via decreased MITF Production. Arch Pharm Res 2004;27:334-9.
[Google Scholar]
|
| 21. |
Wiechers JW, Rawlings AV, Gracia C, Chesne C, Balaguer P, Nicholas JC, et al. A new mechanism of action for skin whitening agents: Binding to the peroxisome proliferator-activated receptor. Int J Cosmet Sci 2005;27:123-32.
[Google Scholar]
|
| 22. |
Wiechers JW, Groenhof FJ, Wortel VAL, Miller RM, Hindle NA, Drewitt Barlow A, et al. Octadecenedioic Acid for a more even skin tone. Cosmetics & Toiletries. Available at http:// www.cosmetics and toiletries.com. Accessed September 25, 2011.
[Google Scholar]
|
| 23. |
Tadokoro T, Bonte F, Archambault JC, Cauchard JH, Neveu M, Ozawa K, et al. Whitening efficacy of plant extracts including orchid extracts on Japanese female skin with melasma and lentigo senilis. J Dermatol 2010;37:522-30.
[Google Scholar]
|
| 24. |
Keeling J, Cardona L, Beniezer A, Epstein R, Rendon M. Mequinol 2% / treinoin 0.01% topical solution for the treatment of melasma in men: A case series and review of literature. Cutis 2008;81:179-83.
[Google Scholar]
|
| 25. |
Lee MH, Kim HJ, Ha DJ, Paik JH, Kim HY. Therapeutic Effect of Topical Application of Linoleic Acid and Lincomycin in Combination with Betamethasone Valerate in Melasma Patients Therapeutic Effect of Topical Application of Linoleic Acid and Lincomycin in Combination with Betamethasone Valerate in Melasma Patients. J Korean Med Sci 2002;17:518-23.
[Google Scholar]
|
| 26. |
Shigeta Y, Imanaka H, Ando H, Ryu A, Oku N, Baba N, et al. Skin Whitening Effect of Linoleic Acid Is Enhanced by Liposomal Formulation. Biol Pharm Bull 2004;27:591-4.
[Google Scholar]
|
| 27. |
Nakamura K, Yoshida M, Uchiva H, Kawa Y, Mizoguchi M. Down-regulation of melanin synthesis by a biphenyl derivative and its mechanism. Pigment Cell Res 2003;16:494-500.
[Google Scholar]
|
| 28. |
Takeda K, Arase S, Sagawa Y, Shikata Y, Okada H, Watanabe S, et al. Clinical Evaluation of the Topical Application of Magnolignan (5,5`-dipropyl-biphenyl-2,2`-diol) for hyperpigmentation on the face. Nishinihon J Dermatol 2006;68:293-8.
[Google Scholar]
|
| 29. |
Takeda K, Yokota T, IkemotoT, Kakishima H, Matsau T. Inhibitory Effect of a Formulation Containing 0.5% Magnolignan (5,5`-dipropyl-biphenyl-2,2`-diol) on UV-induced Skin Pigmentation. Nishinihon J Dermatol 2006;68:288-92.
[Google Scholar]
|
| 30. |
Lee JH, Park JG, Lim SH, Kim JY, Ahn KY, Kim MY, et al. Localized intradermal microinjection of tranexemic acid for treatment of melasma in Asian patients: A preliminary clinical report. Dermatol Surg 2006;32:626-31.
[Google Scholar]
|
| 31. |
Fox C. From Tranexemic acid on freckles to non animal fillers: Patent, Literature finding. Cosmetics and Toiletries. Available at: http: //www.cosmeticsandtoiletries.com. Accessed September 25,2011.
[Google Scholar]
|
| 32. |
Kong YH, Jo YO, Cho CW, Son D, Park S, Rho J, et al. Inhibitory effects of cinnamic acid on melanin biosynthesis in skin. Biol Pharm Bull 2008;31:946-8.
[Google Scholar]
|
| 33. |
Tan C, Zhu W, Lu Y. Aloin, cinnamic acid and sophorcarpidine are potent inhibitors of tyrosinase. Chin Med J (Engl) 2002;115:1859-62.
[Google Scholar]
|
| 34. |
Kang SS, Kim HJ, Jin C, Lee YS. Synthesis of tyrosinase inhibitory (4-oxo-4-H- pyran-2-yl)acrylic acid derivative. Bioorg Med Chem Lett 2009;19:188-91.
[Google Scholar]
|
| 35. |
Zanieri F, Assad GB, Campolini P, Lotti T. Melasma: Successful treatment with 4% Pidobenzone. Dermatol Ther 2008;21:s18-9.
[Google Scholar]
|
| 36. |
Draelos ZD, Yatskayu M, Bhushan P, Pillai S, Oresago C. A Novel combination formulation of kojic acid, emblica extract and glycolic acid compared with hydroquinone 4%. Cutis 2010;86:153-8.
[Google Scholar]
|
| 37. |
Guevara IL, Werllinger KD, Pandya AG. Tolerability and efficacy of a novel formulation in the treatment of melasma. J Drugs Dermatol 2010;9:215-8.
[Google Scholar]
|
| 38. |
Lazou K, Sadick NS, Kurfurst R, Bonnet Duquennoy M, Neveu M, Nizard C, et al. The use of antisense strategy to modulate human melanogenesis. J Drugs Dermatol 2007;6:s2-7.
[Google Scholar]
|
| 39. |
Handog EB, Galang DA, de Leon Godinez MA, Chan GP. A randomized, double-blind, placebo-controlled trial of oral procyanidin with vitamins A, C, E for melasma among Filipino women. Int J Dermatol 2009;48:896-901.
[Google Scholar]
|
| 40. |
Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res 2002;16:567-71.
[Google Scholar]
|
| 41. |
Hwang SW, Oh DJ, Lee D, Kim JW, Park SW. Clinical efficacy of 25% L-ascorbic acid (C'ensil) in the treatment of melasma. J Cutan Med Surg 2009;13:74-81.
[Google Scholar]
|
| 42. |
Sharquie KE, Al-Mashhadani SA, Salman HA. Topical 10% zinc sulfate solution for treatment of melasma. Dermatol Surg 2008;34:1346-9.
[Google Scholar]
|
| 43. |
Sharquie KE, Tikreety MM, Masshadani SA. Lactic acid as a new therapeutic peeling agent in melasma. Dermatol Surg 2005;31:149-54.
[Google Scholar]
|
| 44. |
Sharquie KE, Tikreety MM, Masshadani SA. Lactic acid chemical peels as a new therapeutic modality in melasma in comparison to Jessner's solution chemical peels. Dermatol Surg 2006;32:1429-36.
[Google Scholar]
|
| 45. |
Berardesca E, Cameli N,Primavera G, Carrera M.Clinical and instrumental evaluation of skin improvement after treatment with a new 50% pyruvic acid peel.Dermatol Surg;32:526-34.
[Google Scholar]
|
| 46. |
Khunger N, Sarkar R, Jain RK. Tretinoin peels versus Glycolic acid peels in the treatment of melasma in dark skinned patients. Dermatol Surg 2004;30:756-60.
[Google Scholar]
|
| 47. |
Ghersetich I, Troiano M, Brazzni B, Arunachalam M, Lotti T. Melasma: Treatment with 10% tretinoin peeling mask. J Cosmet Dermatol 2010;9:117-21.
[Google Scholar]
|
| 48. |
Jegasothy SM. Acidifed amino acid in the management of melasma. Available at http://www. miamiskininstitute wordpress.com. Accessed June 24,2010.
[Google Scholar]
|
| 49. |
Ilknur T, Bicak MU, Demirtasoglu M, Ozkan S. Glycolic acid peels versus amino fruit acid peels in the treatment of melasma. Dermatol Surg 2010;36:490-5.
[Google Scholar]
|
| 50. |
Sharmani. Mandelic acid for acne, wrinkles and melasma. Available at http://www.blog. pharmacymix. com. Accessed on May 26, 2011.
[Google Scholar]
|
| 51. |
Taylor MB. Summary of mandelic acid for the improvement of skin conditions. Cosmet Dermatol 1999;21:26-8.
[Google Scholar]
|
| 52. |
Rendon MI, Berson DS, Cohen JL, Roberts WE, Starker J, Wang B, et al. Evidence and Considerations in the Application of Chemical Peels in Skin Disorders and Aesthetic Resurfacing. J Clin Aesthet Dermatol 2010;3:32-43.
[Google Scholar]
|
| 53. |
Effron C, Briden ME, Green BA. Enhancing cosmetic outcomes by combining superficial glycolic acid (alpha-hydroxy acid) peels with nonablative lasers, intense pulsed light, and trichloroacetic acid peels. Cutis 2007;79:4-8.
[Google Scholar]
|
| 54. |
Lee GY, Kim HJ, Whang KK. The effect of combination treatment of the recalcitrant pigmentary disorders with pigmented laser and chemical peeling. Dermatol Surg 2002;28:1120-3.
[Google Scholar]
|
| 55. |
Soliman MM, Ramadan SA, Bassiouny DA, Abdelmalek M. Combined trichloroacetic acid peel and topical ascorbic acid versus trichloroacetic acid peel alone in the treatment of melasma: A comparative study. J Cosmet Dermatol 2007;6:89- 94.
[Google Scholar]
|
| 56. |
Sarkar R, Kaur C, Bhalla M, Kanwar AJ. The combination of glycolic acid peels with a topical regimen in the treatment of melasma in dark-skinned patients: A comparative study. Dermatol Surg 2002;28:828-32.
[Google Scholar]
|
| 57. |
Rokhsar CK, Fitzpatrick RE. The treatment of melasma with fractional photothermolysis. Dermatol Surg 2005;31:1645-50.
[Google Scholar]
|
| 58. |
Goldberg DJ, Berlin AL, Phelps R. Histologic and ultrastructural analysis of melasma after fractional resurfacing. Lasers Surg Med 2008;40:134-8.
[Google Scholar]
|
| 59. |
Lee HS, Won CH, Lee DH, An JS, Chang HW, Lee JH, et al. Treatment of melasma in Asian skin using a fractional 1550 nm laser: An open clinical study. Dermatol Surg 2009;35:1499-504.
[Google Scholar]
|
| 60. |
Neeley MR, Pearce FB, Collann SS. Successful treatment of malar dermal melasma with fractional ablative CO2 laser in a patient with type V skin. J Cosmet Laser Ther 2010;12: 258-66.
[Google Scholar]
|
| 61. |
Xi Z, Gold MH, Zhong L, Ying L. Efficacy and Safety of Q-Switched 1,064-nm Neodymium-Doped Yttrium Aluminum Garnet Laser Treatment of Melasma. Dermatol Surg 2011;37:962-70.
[Google Scholar]
|
| 62. |
Wattan akrai P, Momchan R, Eimpunth S. Low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser for the treatment of facial melasma in Asians. Dermatol Surg 2010;36:76-87.
[Google Scholar]
|
| 63. |
Nouri K, Bowes L, Chartier T, Romagosa R. Combination treatment of melasma with pulsed CO2 followed by Q switch Alexandrite laser. Dermatol Surg 1999;25:494-7.
[Google Scholar]
|
| 64. |
Wang HW, Liu KY. Efficacy and safety of low energy QS Nd Yag and QS Alexandrite laser for melasma. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2009;31:45-7.
[Google Scholar]
|
| 65. |
Trelles MA, Velez M, Gold MH. The treatment of melasma with topical creams alone, CO2 fractional ablative resurfacing alone, or a combination of the two: A comparative study. J Drugs Dermatol 2010;9:315-22.
[Google Scholar]
|
| 66. |
Kim EH, Kim YC, Lee ES, Kang HY. The vascular characteristics of melasma. J Dermatol Sci 2007;46:111-6.
[Google Scholar]
|
| 67. |
Lee HI, Lim YY, Kim BJ, Kim MN, Min HJ, Hwang JH, et al. Clinicopathologic efficacy of copper bromide plus/yellow laser (578 nm with 511 nm) for treatment of melasma in Asian patients. Dermatol Surg 2010;36:885-93.
[Google Scholar]
|
| 68. |
Salem A, Gamil H, Ramadn A, Harras M, Amer A. Melasma: Treatment evaluation. J Cosmet Laser Ther 2009;11:146-50.
[Google Scholar]
|
| 69. |
Grimes PE. Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg 2009;28:77-85.
[Google Scholar]
|
Fulltext Views
15,385
PDF downloads
4,341





