Translate this page into:
Nicolau syndrome involving whole ipsilateral limb induced by intramuscular administration of gentamycin
Correspondence Address:
Jae Eun Choi
Department of Dermatology, Korea University College of Medicine, Inchon-ro 73 (Anam-dong 5ga), Seongbuk-gu, Seoul - 136 705
Korea
| How to cite this article: Kim DH, Ahn HH, Kye YC, Choi JE. Nicolau syndrome involving whole ipsilateral limb induced by intramuscular administration of gentamycin. Indian J Dermatol Venereol Leprol 2014;80:96 |
Sir,
Nicolau syndrome is a serious adverse complication of drug administration. Nicolau syndrome usually presents with severe pain and erythematous -ecchymotic livedoid patches at the injection site. Several studies have indicated that Nicolau syndrome is associated with intra- or perivascular injections, which cause associated vessel damage and, ultimately, lead to peripheral vascular occlusion. Herein, a case of Nicolau syndrome along with a review of the literature is presented.
A 55-year-old man presented with a 1-week history of tender violaceous, ecchymotic patches on his left buttock, thigh, and leg. A few days ago, he had sprained his left elbow and underwent multiple intramuscular injections of gentamycin in the left buttock at a local orthopedic clinic. He experienced unusually severe pain on the night of the fourth injection. The intense burning pain continued the next day in the area around the injection site, which showed erythematous, ecchymotic to purpuric patches. Over the following 5 days, his skin turned violaceous, with more widespread purpuric and irregularly bordered patches spreading over his left limb [Figure - 1]a and b. On magnetic resonance imaging (MRI), a subacute intramuscular hematoma was observed in the left gluteus maximus muscle. The MRI showed soft tissue swelling in the subcutaneous layer of the left buttock, muscle fascia of the gluteus maximus, and the posterior aspect of gluteus medius [Figure - 2]a. Laboratory investigations revealed no abnormalities, except for elevated lactate dehydrogenase levels (1012 IU/L, normal; below 525 IU/L). Histopathologic findings showed multiple extravasated RBCs, superficial perivascular lymphocytic infiltration, focal degeneration of dermal collagen, and fibrin clots in the lumen of the vessels of superficial dermis [Figure - 2]b. Bacteriological culture of the tissues was negative. The patient was diagnosed with Nicolau syndrome on the basis of the clinical and histopathologic evidence. He provided informed consent at the first visit. The patient had mild fever from the first admission date and, thus, a secondary bacterial infection was suspected. Furthermore, our department advised surgical debridement because of the possibility of other disease entities such as necrotizing fasciitis. Therefore, he was treated with intravenous ciprofloxacin for 8 days, oral pentoxifylline for 4 weeks, and recommended rest during the admission. The lesion resolved completely without any functional impairment or residual scarring [Figure - 1]c.
 |
| Figure 1: (a and b) Clinical photo at the first visit, with lesion showing violaceous, ecchymotic, irregular bordered patches that spread over his left limb. (c) After 4 weeks of treatment, the lesion resolved completely without any functional impairment or residual scar |
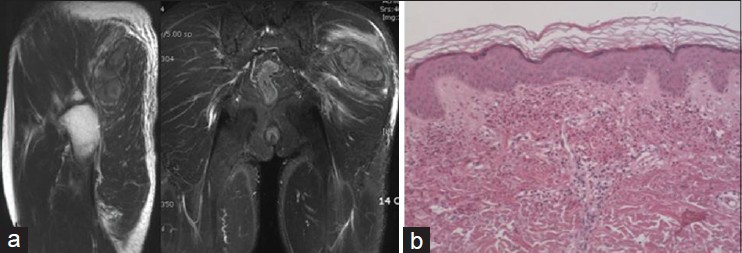 |
| Figure 2: (a) Multiloculated lesion with irregular concentric ring and adjacent edema in the left gluteus maximus muscle. MRI showing soft tissue swelling in the subcutaneous layer of left buttock, muscle fascia of gluteus maximus, and posterior aspect of gluteus medius. (b) Multiple extravasated RBCs, superficial perivascular lymphocytic infiltration, focal degeneration of dermal collagen, and fi brin clots in the lumen of the vessels of the superficial dermis (H and E, ×100) |
Nicolau syndrome is characterized by severe pain followed by early pallor and livedoid hemorrhagic erythema at the injection site. In some cases, Nicolau syndrome can lead to cutaneous, subcutaneous, and even muscular aseptic necrosis with ulceration. It is an unforeseeable but potentially serious complication, mainly observed after the intramuscular administration of a variety of drugs. However, it has also been observed to occur after subcutaneous injections such as injections with etanercept. [1],[2]
Although the pathogenesis of Nicolau syndrome has not been fully elucidated, several theories are suggested. The most reasonable pathogenesis proposed is inflammation, embolism, thrombosis, and vasospasm. First, inflammation produced by vascular or perivascular injection may induce destruction of the whole arterial wall and subsequent necrosis of the skin. Second, embolism caused by an inadvertent intra-arterial injection may give rise to occlusion of small skin arteries. Third, a periarterial injection with arterial wall perforation may lead to thrombosis and necrosis. Fourth, secondary sympathetic vasospasm induced by intra-arterial, periarterial, or perinervous injection may lead to ischemic necrosis. Direct or indirect vessel damage involving any or all these mechanisms ultimately leads to peripheral arterial occlusion. [3],[4] Nicolau syndrome recurrence after a reinjection with the same agent has not been reported. Therefore, Nicolau syndrome is likely not mediated by an allergic/immunologic reaction, or caused by the drug itself. [1],[3]
Although the majority of lesions of Nicolau syndrome are confined to the injection site, the skin lesion of our patient showed rapid spread and an unusually broad range of involvement that included the whole ipsilateral limb in addition to spreading to a part of the contralateral buttock. However, the relatively favorable outcome experienced by this patient who had no residual scarring and no significant necrosis or deep ulceration at the lesion sites implies that the arterial occlusion could not have been the main mechanism of Nicolau syndrome in this patient. The lesion in this patient could have been more substantially associated with occlusion of the peripheral venules or capillary vessels rather than occlusion of the large arteries. [5] Although further research is required for validation of the above hypothesis, our case could be an intriguing reference case for the pathophysiology of Nicolau syndrome.
| 1. |
Koller S, Kränke B.Nicolau syndrome following subcutaneous glatiramer-acetate injection. J Am AcadDermatol 2011;64:e16-7.
[Google Scholar]
|
| 2. |
Guarneri C, Polimeni G. Nicolau syndrome following etanercept administration. Am J ClinDermatol 2010;11(Suppl 1):51-2.
[Google Scholar]
|
| 3. |
Luton K, Garcia C, Poletti E, Koester G. Nicolausyndrome: Three cases and review.Int J Dermatol 2006;45:1326-8.
[Google Scholar]
|
| 4. |
Marangi GF, Gigliofiorito P, Toto V, Langella M, Pallara T, Persichetti P.Three cases of embolia cutis medicamentosa (Nicolau's syndrome). J Dermatol 2010;37:488-92.
[Google Scholar]
|
| 5. |
García-Vilanova-Comas A, Fuster-Diana C, Cubells-Parrilla M, Pérez-Ferriols MD, Pérez-Valles A, Roig-Vila JV.Nicolau syndrome after lidocaine injection and cold application: Arare complication of breast core needle biopsy. Int J Dermatol2011;50:78-80.
[Google Scholar]
|
Fulltext Views
4,171
PDF downloads
2,719





