Translate this page into:
Non-familial multiple keratoacanthomas in a 70 year-old long-term non-progressor HIV-seropositive man
2 Department of Pathology, Dr. RML Hospital, New Delhi, India
Correspondence Address:
Hemanta Kumar Kar
D-II/A-71, South Moti Bagh, New Delhi-110 021
India
| How to cite this article: Kar HK, Sabhnani ST, Gautam R K, Sharma P K, Solanki K, Bhardwaj M. Non-familial multiple keratoacanthomas in a 70 year-old long-term non-progressor HIV-seropositive man. Indian J Dermatol Venereol Leprol 2008;74:136-138 |
Abstract
We describe here multiple keratoacanthomas in an Human Immunodeficiency Virus (HIV)-seropositive 70 year-old man. The patient had multiple epithelial tumors of the skin showing rapid growth, histopathological features of a keratoacanthoma and a conspicuous tendency toward spontaneous remission. A diagnosis of nonfamilial multiple keratoacanthoma was established. The patient had a CD4 count of 633 cells/�L. The HIV disease in our patient was of a nonprogressive nature with CCR5-positive T cells.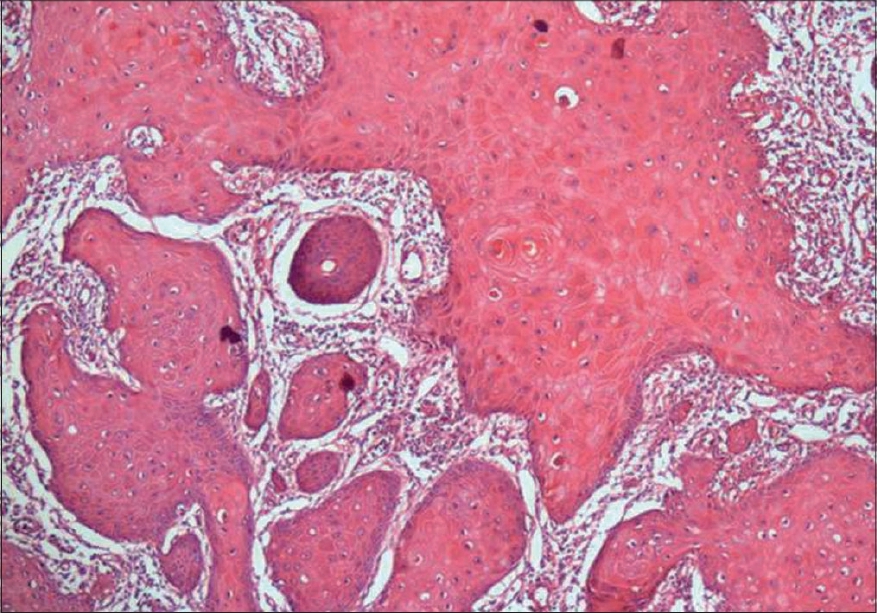 |
| Figure 4: Epidermal proliferation showing glassy cytoplasm (H and E, 100X) |
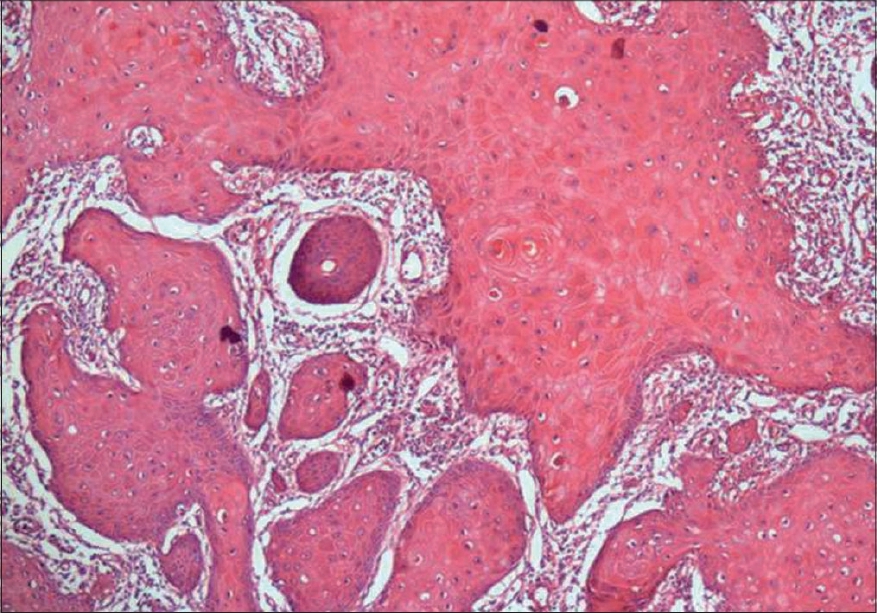 |
| Figure 4: Epidermal proliferation showing glassy cytoplasm (H and E, 100X) |
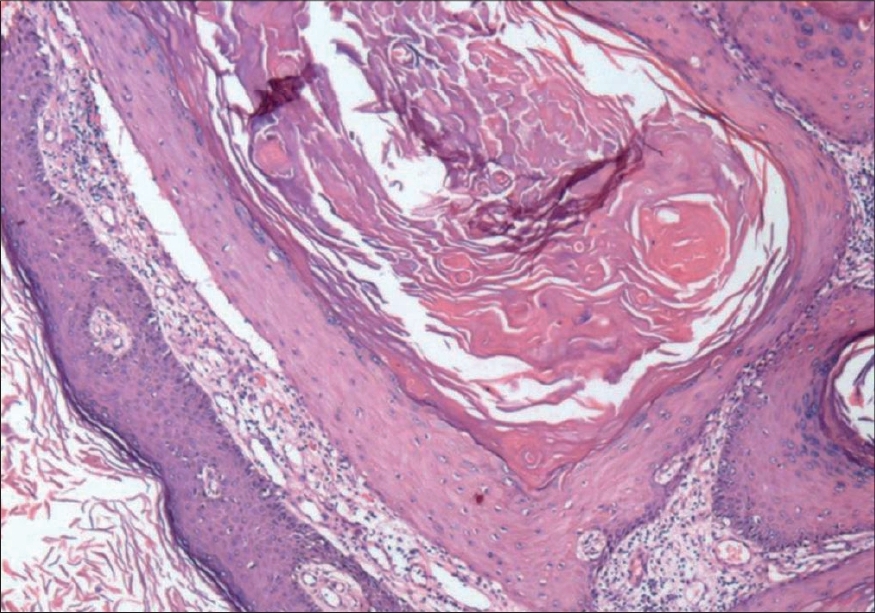 |
| Figure 3: Keratin-filled crater with irregular epidermal proliferation extending into the dermis (H and E, 40X) |
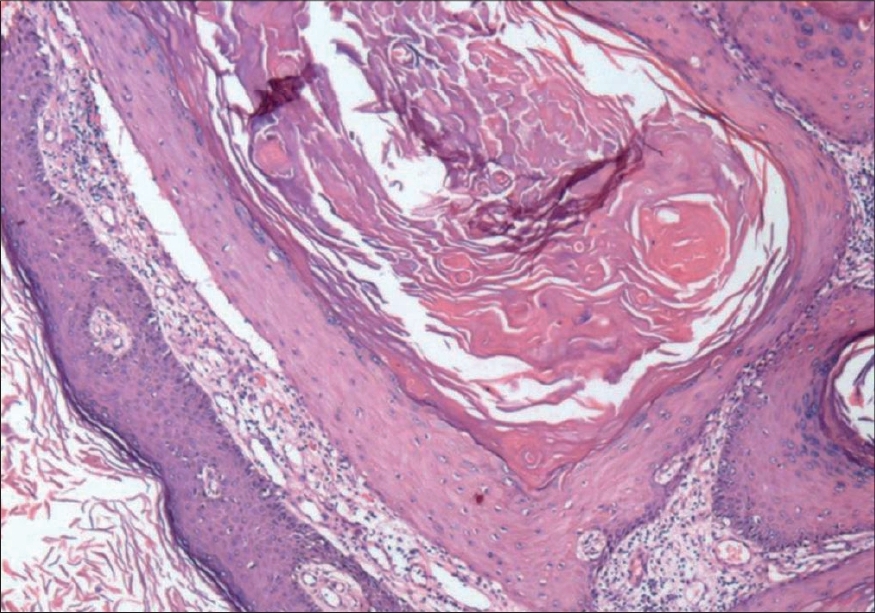 |
| Figure 3: Keratin-filled crater with irregular epidermal proliferation extending into the dermis (H and E, 40X) |
 |
| Figure 2: Multiple Keratoacanthomas at the time of admission over forearm and hand |
 |
| Figure 2: Multiple Keratoacanthomas at the time of admission over forearm and hand |
 |
| Figure 1: Multiple keratoacanthomas over leg with koebner phenomenon |
 |
| Figure 1: Multiple keratoacanthomas over leg with koebner phenomenon |
Introduction
Keratoacanthoma is an epithelial tumor of the skin characterized by rapid growth, histopathology similar to that of squamous cell carcinoma and a tendency towards spontaneous remission. [1] Keratoacanthomas have been noted in patients with immunosuppression but rarely in the HIV-infected. [2] We report here a case of non-familial multiple keratoacanthomas in a 70 year-old, long-term non-progressor, HIV-seropositive male patient.
Case Report
A 70 year-old male presented with a few pinhead-sized, itchy, papular lesions on his left wrist and the adjoining forearm. Within a week, similar lesions appeared elsewhere. These lesions increased in size over three weeks to form nodules of variable sizes (1-1.5 cm). Sexual history of the patient revealed exposure to multiple extramarital sexual contacts with female sex workers while working in Mumbai from 1958 to 1968 at his age of 28 to 38 years. There was no history of any blood transfusion, surgery, fever, diarrhea, loss of weight, joint pains or drug reaction or any other systemic disease including diabetes. The patient was a chain smoker for the last 25 years. He denied any history of skin diseases or sexually transmitted infections in the past. There was no history of similar lesions observed in his parents or siblings. The patient′s HIV status was noticed two years ago only after the death of his wife (HIV status unknown). The patient′s children had died young at ages below five years; hence, no information was available about their HIV status.
On examination, the patient looked healthy for his age and had no pallor. There was clubbing of the fingernails. He had bilateral 2-3 cm-in size, soft, nontender, mobile, discrete inguinal lymph nodes. Cutaneous examination revealed multiple skin-colored and a few pigmented papules and nodules of various sizes on the dorsal aspect of both hands, the extensor aspect of the left forearm, the medial side of both legs, on the left foot and upper back [Figure - 1],[Figure - 2]. Some of the lesions on the left leg had central crusting while the lesions on the forearm, both legs and the back showed umbilication. The papules and nodules on the left leg showed grouping and Kobner′s phenomenon [Figure - 1].
Investigations revealed normal complete hemogram, liver and kidney function tests and blood sugar levels; VDRL was nonreactive. Anti-HIV-1 antibodies were detected by using both ELISA and Western Blot. Rapid test for CCR5 cell surface marker was positive in lymphocytes using flow cytometry (conducted at the National Institute of Immunology, New Delhi). The CD4 count was 633 cells/µL, CD8: 1568 cells µL, CD 3 : 2271 cells/µL, CD 4 :CD8 = 0.40. Mantoux test was positive (13 mm x 14 mm) and sputum for acid-fast bacilli tested negative on three occasions. The X-ray chest (PA view), ultrasound (abdomen and pelvis) and sigmoidoscopy were normal.
The histopathological evaluation from one of the nodules showed an acanthotic epidermis with irregular elongations of the rete ridges. There was irregular epithelial proliferation in the islands of stratified squamous epithelium with glassy cytoplasm [Figure - 3],[Figure - 4]. Individual cell keratinization was also observed. The dermis showed the presence of a chronic inflammatory infiltrate. There was no human papilloma virus (HPV) DNA in the skin tissue samples analyzed by means of the polymerase chain reaction (PCR) technique.
During the patient′s stay in the wards, there were fresh crops of similar lesions followed by resolution. However, some of the bigger lesions were treated with cryotherapy using liquid nitrogen for quicker resolution. In the next two months′ follow-up period after discharge from the hospital, there was almost complete resolution of all lesions.
Discussion
Keratoacanthoma commonly occurs in the elderly as a solitary lesion; however, occasionally, there are several lesions growing rapidly within a few weeks. [2] The lesions usually measure 1-2.5 cm and three clinical stages have been described: proliferative, mature and resolving. [2] There are two variants of multiple keratoacanthoma: the self-healing epitheliomas (Ferguson-Smith) type and the eruptive Grzybowski type. Both variants are rare. The Ferguson-Smith type is a familial form, which affects both sexes with equal severity. Most cases develop during childhood and adolescence and are characterized by the appearance of multiple, sometimes hundreds of keratoacanthomas. This disorder is inherited in an autosomal dominant form and has been described only in a few Scottish families. The eruptive Grzybowski type is characterized by tiny (2-3 mm diameter) and numerous follicular keratotic papules disseminated all over the body including the oral mucosa. In our case, the lesions clinically and histopathologically resembled solitary keratoacanthoma although they were multiple. In our patient, lesions of all three stages were observed during his continuous four months′ stay indoors.
Graells et al. reported a case of Muir-Torrι syndrome in an HIV-positive male, who presented with a solitary keratoacanthoma and multiple sebaceous adenomas without any visceral neoplasm. [3] Our patient with multiple keratoacanthomas was evaluated for the presence of the typical traits of Muir-Torrι syndrome but there was no cutaneous sebaceous tumor or any other carcinoma of the GI tract, lung and genitourinary tract.
Keratoacanthomas have also been reported in immunosuppresed patients after bone marrow transplantation cyclosporine treatment or infection with HIV, thus suggesting that immunosuppression may play an etiologic role in some cases. [2],[3],[4] Payne et al. reported two homosexual HIV-positive men with solitary keratoacanthoma, one preceded an epidermal cyst on the cheek while the chest was affected in the other patient. [4] Studies by Payne et al. and others showed an association of keratoacanthoma with human papilloma virus (HPV) 25, HPV-19 and HPV-48 in lesions arising in HIV-infected patients. [4],[5] By the use of PCR, cutaneous HPV DNA was detected in only 51% (37/72) of the keratoacanthomas. [5] In our case, the isolation and typing of HPV by PCR revealed a negative result, which was in corroboration with study by Lus et al. [6] who did not find any association between known HPV types and keratoacanthoma.
The atypical features in our case were multiple keratoacanthomas occurring in crops for a few months and the prolonged asymptomatic phase of the HIV disease itself. The patient possibly acquired HIV infection thirty-five years ago and was still asymptomatic and disease-free but for the appearance of multiple keratoacanthomas. The present CD4 count was 633 cells/µL. Our case can be labeled as a long-term nonprogressor case. The lack of HIV disease progression has been explained in some by a defect in the virus, in others by any of a variety of host factors including recognized and as yet unrecognized genetic factors and in yet others by a combination of both. Several genetic mutations have been demonstrated to result in a delay in the progression of HIV disease. They include heterozygosity for CCR5-∆32 deletion, heterozygosity for CCR2-641 mutation, homozygosity for the SDF1-3′A mutation and heterozygosity for the RANTES-28G mutation. [7] Peripheral lymphocytes from our patient tested positive for CCR5 cell surface markers and thus, we excluded one of the genetic factors of nonprogression.
It is difficult to ascertain the cause and association of HIV and multiple keratoacanthoma in the absence of HPV infection, significant immunosuppression due to HIV infection (nonprogressive) and Muir-Torre syndrome as in this case. It is possible that HIV infection could have influenced the appearance of keratoacanthomas over several months. To the best of our knowledge, this is the first case of an association of HIV infection with multiple keratoacanthomas.
Acknowledgment
The authors gratefully acknowledge Dr. Jameel Shahid, group leader, Virology group, National Institute of Immunology, New Delhi for his contribution in the determination of CCR5 on the lymphocytes and for ongoing studies factors for the nonprogression of HIV disease.
| 1. |
MacKie RM, Quinn AG. Non-melanoma skin cancer and other epidermal skin tumors. In : Burns T, Breathnach S, Cox N, Griffiths C, et al. editors. Rook's textbook of dermatology, 7 th ed, Oxford: Blackwell Publishing; 2004. p. 36.45.
th ed, Oxford: Blackwell Publishing; 2004. p. 36.45.'>[Google Scholar]
|
| 2. |
Cerroni L, Kerl H. Keratoacanthoma. In : Freedberg IM, Eisen AZ, Austen KF, Goldsmith LA, Katz SI, editors. Fitzpatrick's dermatology in general medicine, 6 th ed. New York: McGraw Hill; 2003. p. 762-3.
th ed. New York: McGraw Hill; 2003. p. 762-3.'>[Google Scholar]
|
| 3. |
Graells J, Marcoval M, Badell A, Notario J, Fulladosa X. Muir-Torrι syndrome in a patient with acquired immunodeficiency syndrome. Br J Dermatol 1996;135:159-61.
[Google Scholar]
|
| 4. |
Payne D, Newman C, Trying S. Human papillomavirus DNA in nonanogenital keratoacanthoma and squamous cell carcinoma of patients with HIV infection. J Am Acad Dermatol 1995;33:1047-9.
[Google Scholar]
|
| 5. |
Forslund O, DeAngelis PM, Beigi M, Schjolberg AR, Clausen OP. Identification of human papillomavirus in keratoacanthomas. J Cutan Pathol 2003;30:423-9.
[Google Scholar]
|
| 6. |
Lu S, Syrjanen SL, Havu VK, Syrjanen S. Known HPV types have no association with keratoacanthomas. Arch Dermatol Res 1996;288:129-32.
[Google Scholar]
|
| 7. |
Anthony S, Fauci H, Lane C. Human immunodeficiency virus (HIV) disease: AIDS and related disorders. In : Braunwald, Fauci, Kasper, Hauser, Longo, Jameson, editors. Harrison's principles of clinical medicine, 15 th ed, New York: McGrawHill; 2003. p. 1865.
th ed, New York: McGrawHill; 2003. p. 1865.'>[Google Scholar]
|
Fulltext Views
1,910
PDF downloads
988





