Translate this page into:
Non-pruritic blisters over extensors in a young male
Corresponding author: Dr. Anupama Bains, Department of Dermatology, Venereology and Leprology, All India Institute of Medical Sciences, Jodhpur, India. whiteangel2387@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kannan K, Bains A, Alam A, Bano N, Thirunavukkarasu B. Non-pruritic blisters over extensors in a young male. Indian J Dermatol Venereol Leprol. 2024;90:526-9. doi: 10.25259/IJDVL_22_2023
A 23-year-old man presented with multiple asymptomatic tiny blisters over the trunk and extremities since 2 years. Lesions used to rupture in 1–2 days and healed with hyperpigmentation. There was no history of abdominal pain, vomiting, loose stools or any other illness. Cutaneous examination revealed multiple grouped vesicles and crusted papules on a background of normal skin over the trunk and extremities with post an inflammatory hyperpigmentation [Figures 1a, 1b, 1c and 1d]. The mucosae were normal.

- Multiple grouped vesicles and crusted papules on a background of normal skin – right elbow.

- Multiple grouped vesicles and crusted papules on a background of normal skin and a few lesions healing with hyperpigmentation – upper back.
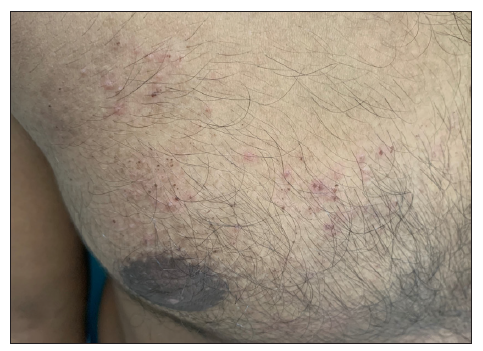
- Multiple grouped vesicles and crusted papules on a background of normal skin and a few lesions healing with hyperpigmentation – chest.

- Multiple grouped vesicles and crusted papules on a background of normal skin and a few lesions healing with hyperpigmentation – back.
Microscopic Findings
Tzanck smear from the vesicle didn’t show any acantholytic cells and a KOH examination of skin scrapings was negative. Histopathology revealed neutrophilic exocytosis, spongiosis and intraepidermal vesicles filled with oedema fluid, neutrophils, eosinophils and occasional degenerated epidermal cells. Superficial dermis showed mild perivascular inflammatory infiltrate composed of lymphocytes and few neutrophils [Figures 2a and 2b]. Direct immunofluorescence (DIF) from perilesional skin showed intercellular deposition of IgG (2+) in the upper epidermal layers [Figure 3] while IgA, IgM, C3 and fibrinogen were negative.
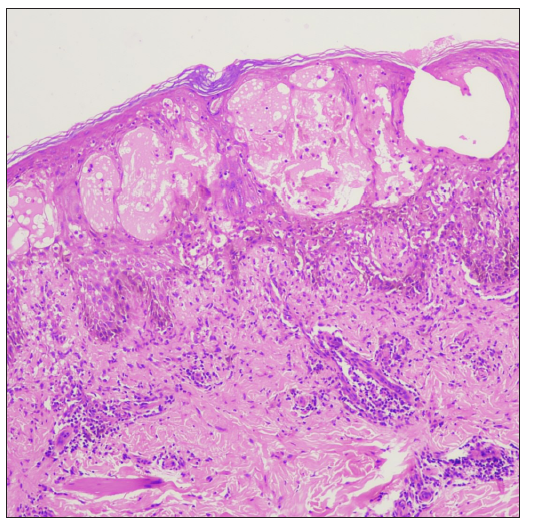
- Epidermis showing neutrophilic exocytosis, spongiosis and intraepidermal vesicle formation. Superficial dermis showed mild perivascular inflammatory infiltrate composed of lymphocytes and a few neutrophils (Haematoxylin and Eosin; 100x).
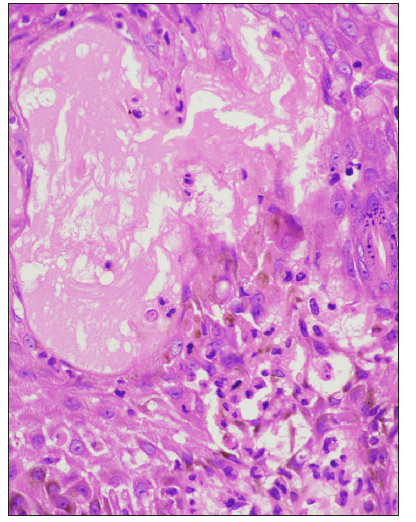
- There is basal layer vacuolar degeneration, inflammatory infiltrate rich in neutrophils, eosinophils and lymphocytes (Haematoxylin and Eosin; 400x).
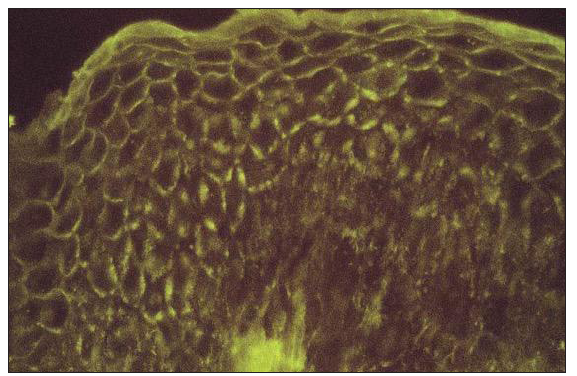
- High power image of direct immunofluorescence from perilesional skin showing intercellular deposition of IgG (Intensity 2+) – fishnet pattern positivity predominantly in the upper layer of the epidermis (DIF - IgG) (200x).
Question
What is your diagnosis?
Diagnosis
Pemphigus herpetiformis
Based on clinical and immunopathological findings, a diagnosis of pemphigus herpetiformis (PH) was made and the patient had complete resolution of lesions within 8 weeks of starting oral dapsone 100 mg once a day.
Discussion
Pemphigus herpetiformis is a rare variant of pemphigus accounting for around 7% of all pemphigus cases. It usually presents with pruritic herpetiform vesicles or annular/urticarial erythematous plaques with/without erosions on the trunk and proximal extremities. The index case also presented with grouped vesicles; however, the lesions were non-pruritic which was unusual. The mucosae are usually spared. These patients usually have circulating auto-antibodies against desmoglein 1 (Dsg1) and less commonly against desmoglein 3 (Dsg3) or desmocollins. It can evolve into pemphigus foliaceous (PF) or vulgaris in a few cases.1
Clinical differential diagnoses considered in the present case were dermatitis herpetiformis (DH), pemphigus herpetiformis and tinea corporis (vesicular variant). Pemphigus herpetiformis can present with clinical features of dermatitis herpetiformis and immunopathologic findings consistent with pemphigus; hence, it is also known as mixed bullous disease.2 It can also mimic eczema, pemphigus vulgaris, pemphigus foliaceous, bullous pemphigoid, IgA pemphigus or linear IgA disease.1 Biopsy findings can vary based on the duration/stage of the disease. Many times, multiple or repeat biopsies are required to diagnose pemphigus herpetiformis. Pemphigus herpetiformis and its mimickers are differentiated with the help of histopathology, direct immunofluorescence and serology.
Histopathology of pemphigus herpetiformis, as in our case, usually shows intraepidermal split with minimal or absent acantholysis, eosinophilic or neutrophilic spongiosis and microabscesses with intraepidermal intercellular staining of IgG/C3 on DIF. This contrasts with dermatitis herpetiformis which shows subepidermal split with papillary tip neutrophilic microabscesses with granular IgA deposition at the tips of the dermal papillae on DIF. In addition, ELISA (Enzyme-linked immunosorbent assay), indirect immunofluorescence or immunoblotting in pemphigus herpetiformis can detect circulating auto-antibodies against Dsg1 and less commonly, Dsg3 or desmocollins.1,3
Clinically, pemphigus herpetiformis differs from pemphigus vulgaris in sparing the mucosae and from pemphigus foliaceous in having herpetiform vesicles (rather than crusted erosions) over trunk and proximal extremities. Acantholytic cells are virtually always present in the histology of pemphigus vulgaris and pemphigus foliaceous while they are either scarce or absent in pemphigus herpetiformis.1,3 Intercellular IgG/C3 staining on DIF is common to pemphigus vulgaris, pemphigus foliaceous and pemphigus herpetiformis, hence DIF findings may not be able to differentiate between these diagnoses. Pemphigus vulgaris though shows a fishnet/chicken wire pattern of staining in direct immunofluorescence, while pemphigus foliaceous can show more intense staining of the upper epidermal layers.3,4
Intraepidermal type of IgA pemphigus can closely mimic pemphigus herpetiformis on histopathology and it is diagnosed based on the intercellular IgA deposition on direct immunofluorescence in IgA pemphigus, whereas there is deposition of IgG/C3 in a case of pemphigus herpetiformis. Both Linear IgA disease and bullous pemphigoid are easy to exclude as histology shows subepidermal blisters with staining for IgA and IgG/C3 respectively at the dermoepidermal junction. Vesicular/vesiculobullous tinea, which was considered as one of the differential shows spongiosis and parakeratosis with periodic acid schiff (PAS)/methanamine silver stain demonstrating fungal elements while eczema would show spongiosis, moderate to dense inflammatory infiltrate, dermal oedema in the acute phase and hyperkeratosis, acanthosis and minimal infiltrate in chronic phase.5,6
Pemphigus herpetiformis is treated primarily with dapsone which may be supplemented with oral steroids and/or other immunosuppressants like azathioprine, cyclophosphamide, mycophenolate mofetil, rituximab, in case of inadequate response.7
The present case had been misdiagnosed as tinea corporis and received antifungals from various dermatologists and physicians over the last 2 years. This case highlights the importance of a careful clinico-immunopathological correlation to reach the correct diagnosis of this rare variant. It is also important to identify this type of pemphigus because of its better prognosis and its remarkable response to dapsone which may obviate the need for oral steroids unlike pemphigus vulgaris,
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Clinical, pathologic and immunologic features of pemphigus herpetiformis: A literature review and proposed diagnostic criteria. Int J Dermatol. 2019;58:997-1007.
- [CrossRef] [PubMed] [Google Scholar]
- Pruritic blistering eruption: Answer. Am J Dermatopathol. 2020;42:144-5.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of immunofluorescence in dermatology. Indian Dermatol Online J. 2017;8:1-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pemphigus herpetiformis: A case series and review of the literature. Int J Dermatol. 2015;54:1014-22.
- [CrossRef] [PubMed] [Google Scholar]






