Translate this page into:
Nonablative lasers and nonlaser systems in dermatology: Current status
2 MS Dermatology Group, Bangalore, India
3 Venkat Charmalaya Centre for Advanced Dermatology, Bangalore, India
Correspondence Address:
Mukta Sachdev
HOD, Department of Dermatology, Manipal Hospital, 98 Rustom Bagh Road, Old Airport Road, Bangalore 560017
India
| How to cite this article: Sachdev M, Hameed S, Mysore V. Nonablative lasers and nonlaser systems in dermatology: Current status. Indian J Dermatol Venereol Leprol 2011;77:380-388 |
Abstract
Nonablative lasers and nonlaser systems are newer systems used for skin rejuvenation, tightening, body sculpting, and scar remodeling. Devices: Different technologies such as lasers, Intense Pulsed Light (IPL), and radiofrequency have been introduced. Most nonablative laser systems emit light within the infrared portion of the electromagnetic spectrum (1000-1500nm). At these wavelengths, absorption by superficial water containing tissue is relatively weak, thereby effecting deeper tissue penetration. A detailed understanding of the device being used is recommended. Indications: Nonablative technology have been used for several indications such as skin tightening, periorbital tissue tightening, treatment of nasolabial lines and jowl, body sculpting/remodeling, cellulite reduction, scar revision and remodeling and for the treatment of photodamaged skin. Facility: Nonablative laser and light modalities can be carried out in a physician treatment room or hospital setting or a nursing home with a small operation theater. Preoperative counseling and informed consent: The dermatologic consultation should include detailed assessment of the patient's skin condition and skin type. An informed consent is mandatory to protect the rights of the patient as well as the practitioner. All patients must have carefully taken preoperative and postoperative pictures. Choice of the device and parameters: Depends on the indication, the area to be treated, the acceptable downtime for the desired correction, and to an extent the skin color. Anesthesia: These lasers are mostly pain-free and tolerated well by patients but may require topical anesthesia. In most cases, topical cooling and numbing using icepacks is sufficient, even in an apprehensive patient. Postoperative care: The nonablative lasers, light sources and radiofrequency systems are safe, even in darker skin types, and postoperative care is minimal. Proper postoperative care is important in avoiding complications. Post-treatment edema and redness settle in a few hours to a few days. Postoperative sun avoidance and use of sunscreen is mandatory.Introduction
Nonablative technologies are newer systems used for skin rejuvenation, tightening, body sculpting, and scar remodeling. These technologies provide an alternative to ablative lasers, and are said to reduce the incidence of side effects and increase patient compliance. Nonablative lasers induce dermal neocollagenesis without epidermal disruption, thereby limiting adverse effects and virtually eliminating down-time. [1] Although the results are less dramatic, these lasers are of special interest in skin of colour, where risk of complications is higher with ablative modalities. Most nonablative laser systems emit light within the infrared portion of the electromagnetic spectrum (1000-1500nm). At these wavelengths, absorption by superficial water containing tissue is relatively weak, thereby effecting deeper tissue penetration. [1] The term nonablative skin resurfacing includes the term subsurfacing, noninvasive resurfacing, skin toning, and wrinkle reduction. [2]
Nonablative skin resurfacing technology can be categorized into five different general modalities: Radiofrequency systems, mid-infrared lasers, intense pulsed light systems (IPL), vascular lasers, and light emitting diodes (LED). [3]
This article will discuss radiofrequency systems, lasers, and IPL technology.
References
- Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of Laser Skin Resurfacing: Nonablative, Fractional and Ablative laser resurfacing. J Am Acad Dermatol 2008;58:719-37.
- Marmur ES, Goldberg DJ. Nonablative skin resurfacing. In: Goldberg DJ, Dover SJ, editors. Lasers and Lights. 2nd ed, vol 2. Philadelphia: Elsevier; 2008. p. 43-54.
- Alexiades-Armenakas MR, Kaminer MS. Skin tightening with radiofrequency. In: Goldberg DJ, Dover SJ, editors. Lasers and Lights. 2nd ed, vol 2. Philadelphia: Elsevier; 2008. p. 55-72.
Rationale and Scope
This is a new technology with rapidly expanding and changing profile and concepts. This article reviews the current status of this technology in the light of available evidence.
Radiofrequency Devices
Radiofrequency devices for skin rejuvenation are new and provide distinctive treatment options for nonablative rejuvenation. Radiofrequency devices heat the dermis and possibly the subdermal tissues, resulting in clinical findings of skin tightening. The first device in this area was a monopolar radiofrequency (RF) device that was FDA approved for the noninvasive tightening of periorbital rhytides using this proven mechanism of skin tightening. [1] Disadvantages of that first generation device included inconsistency of clinical results and significant discomfort during treatment. Newer bipolar and monopolar RF devices are constantly being developed to improve results and minimize discomfort.
RF energy is produced by an electric current rather than by a light source. Radiofrequency energy is conducted electrically to tissue, and heat is produced when the tissue′s inherent resistance (impedance) converts the electrical current to thermal energy. This reaction is dictated by the following formula: energy (J) = I2 Χ R Χ T (where I = current, R = tissue impedance, and T = time of application). [2] High-impedance tissues, such as subcutaneous fat, generate greater heat and account for the deeper thermal effects of RF devices.
Both monopolar and bipolar RF devices have been used for cutaneous applications. Monopolar systems deliver current through a single contact point with an accompanying grounding pad that serves as a low resistance path for current flow to complete the electrical circuit. [2] Monopolar electrodes concentrate most of their energy near the point of contact, and energy rapidly diminishes as the current flows toward the grounding electrode. [3] Bipolar devices pass electrical current only between two positioned electrodes applied to the skin. No grounding pad is necessary with these systems because no current flows throughout the rest of the body. [4],[5],[6],[7]
Lately, even tripolar RF systems have been devised. Tripolar treatments exclusively utilize the effects of combining unipolar RF and bipolar RF energies in one applicator to simultaneously heat deep and superficial tissue layers, while protecting the surface skin. [3] The tripolar RF technology uses sophisticated algorithms to control the treatment electrodes which change the current and polarity to achieve variable energy focus in different fat layers resulting in visible clinical results. This system is also used for the treatment of skin laxity and facial recontouring.
References
-
Weiss RA, Weiss MA, Munavalli G, Beasley KL. Monopolar radiofrequency facial tightening: A retrospective analysis of efficacy and safety in over 600 treatments. J Drugs Dermatol 2006;5:707-12.
- Fitzpatrick R, Geronemus R, Goldberg D, Kaminer M, Kilmer S, Ruiz-Esparza J. Multicenter study of noninvasive radiofrequency for periorbital tissue tightening. Lasers Surg Med 2003;33:232-42.
- Zelickson BD, Kist D, Bernstein E, Brown DB, Ksenzenko S, Burns J, et al. Histological and ultrastructural evaluation of the effects of a radio-frequency- based non-ablative dermal remodeling device: A pilot study. Arch Dermatol 2004;140:204-9.
- Sadick NS, Mulholland RS. A prospective clinical study to evaluate the efficacy and safety of cellulite treatment using the combination of optical and RF energies for subcutaneous tissue heating. J Cosmet Laser Ther 2004;6:187-90.
- Hsu TS, Kaminer MS. The use of non-ablative radiofrequency technology to tighten the lower face and neck. Semin Cutan Med Surg 2003;22:115-23.
- Sadick N, Alexiades-Armenakas M, Bitter P, Hruza G, Mulholland S. Enhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted, bipolar radiofrequency energy (ELOS): Introducing selective radiophotothermolysis. J Drugs Dermatol 2005;4:181-6.
- Ruiz-Esparza J, Gomez JB. The medical facelift: A noninvasive, nonsurgical approach to tissue tightening in facial skin using nonablative radiofrequency. Dermatol Surg 2003;29:325-32.
Technical Information about Different Radiofrequency Machines
It is not the objective of this article to discuss individual machines from different manufacturers. However, since each device has different specifications, basic information about some commonly used machines in India are discussed here briefly.
ThermaCool (Thermage Laser; ) : The first radiofrequency device for skin rejuvenation was the monopolar RF device. ThermaCool, which was FDA approved in 2002, is a non-invasive, non-ablative device that uses monopolar radiofrequency energy to bulk heat underlying skin while protecting the epidermis. The generated heat produces subtle damage to collagen, and in combination with the subsequent inflammatory cascade induced by heating, a tightening effect is realized. The device heats tissues to 65°C to 75°C, which is the critical temperature at which collagen denaturation occurs. [1] ThermaCool is an efficacious and safe nonsurgical alternative for treating mild skin laxity. It is used for the treatment of rhytids on the face including the periorbital region and lower face. [1] Advanced Fluorescence Technology (AFT) lasers work on the same lines as the Thermage laser.
Advantages include the minimal erythema postoperatively that typically resolves within hours, and lack of significant risk of side effects. Initial disadvantages of the system were inconsistent results, skin atrophy, and depressions from very aggressive treatment at high fluences, blistering, scarring, development of temporary nodules and swellings, and no improvement in the treated patient.
Electro-Optical Synergy (ELOS) : ELOS is a unique combination of RF and optical energies. With electro-optical synergy technology, optical energy is converted to heat within the tissue according to the principles of selective photothermolysis. [2] The optical energy is emitted to preheat dermal structures, which then creates a temperature differential between the targeted structures and the surrounding tissues; these temperature changes allow for the directed application of RF energy to dermal chromophores with less impedance. A combination of skin pre-cooling and selective target heating using the optical energy source creates this thermal gradient. The optical energy levels are lower than those used in traditional light-based systems, thereby enabling potentially safer treatments in all skin types. It is used for the treatment of skin laxity.
Accent system: The Accent system contains both bipolar and unipolar technologies in one device. [3] The base system generates 40.84 MHz of RF energy. In the unipolar mode, RF energy is applied as electromagnetic radiation, not electrical current from a single electrode tip without a grounding plate. The energy is delivered to a penetration depth of up to 20 mm. In the bipolar mode, the RF current is applied between two points on the tip of the probe, to a penetration depth of 2 mm to 6 mm. In addition, since this is not a stationary energy delivery device, but rather energy is delivered in a mobile fashion, pain control is not needed. Mineral oil is used to decrease friction of the hand-piece across the skin. Skin surface temperature monitoring is performed and a peak temperature of 40−42 °C is maintained. This system is used not only for facial tightening but also for body fat re-sculpting and cellulite reduction.
Nonablative Lasers
Several nonablative laser systems have been introduced for different indications such as dermal remodeling, acne scars, etc. The manufacturers claim that these systems are effective and safer than the previously available ablative lasers. Postoperative sequelae and healing time are reported to be less. [4] However, more recently nonabaltive fractional lasers have become available and have replaced many of the conventional nonabaltive lasers. These fractional lasers have been dealt with separately in another taskforce report.
1540 nm Erbium Glass Laser
This is a mid-infrared range laser that targets intracellular water to a depth of 0.4 mm to 2 mm. At this wavelength, there is minimal absorption of energy by melanin, hence it is safer to use in darker skin types. Its emitted wavelength of 1.54 ΅m shows high water absorption. [4] This is a flashlamp pumped system. The wavelength is obtained from a specific co-doped Yb-Er:phosphate glass material, optimized for high efficiency pumping absorption and delivered by an optic fiber. [5] The light energy is deposited predominantly in the dermis, leading to new collagen formation, dermal thickening and clinical improvement. This laser has been used in the treatment of fine lines, wrinkles, and acne scars.
Long pulsed neodymium-doped yttrium aluminium garnet laser 1320 nm or 1064 nm
Nonablative remodeling lasers such as Nd:YAG 1320 or 1064nm have been used to reduce acne scarring. [6] It can be used either alone or in combination with another nonabaltive system such as a combined 585/1064 laser (sequential dual wavelength PDL and long-pulsed Nd:YAG). [7] Reported efficacy compared to fractional ablative and ablative lasers may be lower. A split-face clinical study conducted in Seoul, Korea in 2009, revealed that combining two nonablative systems, for example, a combined 585/1064 laser (sequential dual wavelength PDL and long-pulsed Nd:YAG) is more effective for deeper boxcar scars. [8] Histopathological analysis revealed neocollagenesis and greater scar tissue reorganization. Another study conducted in Gyeongbuk, Korea concluded that combining nonablative lasers like 1320 nm or 1064nm Nd:YAG laser systems with an ablative technology like an AFR carbon dioxide (CO 2 ) laser device, results in better efficacy and fewer complications. [9]
1550 nm erbium doped fiber laser
This is a non ablative fractional laser (NAFL) with a mid-infrared wavelength emitted by a 1550 nm erbium doped laser that creates non contiguous columns of microscopic thermal zones (MTZ) in the dermis. [4] These MTZs produce localized epidermal necrosis and collagen denaturation at 125 or 250 MTZ/cm 2 . As the tissue surrounding each MTZ column is intact, the surrounding normal epidermal and dermal cells migrate into the zone of damage to produce rapid healing. This technology has been used in the treatment of atrophic, hypertrophic, erythematous, and even hypopigmented scars.
585 nm flashlamp pulsed dye laser (FLPDL)
With its selective photothermolysis action, the pulsed dye laser targets the chromophore oxyhemoglobin to create a thermal insult to the dermal microvasculature, thereby inducing a low grade inflammatory response, which triggers fibroblast activity, which are responsible for dermal collagen production. Bjerring et al., showed that an 84% increase in the rate of type III collagen production above normal background levels was observed in areas treated with a low fluence 585 nm pulsed dye laser with a temporal profile and pulse duration designed specifically to target healthy microvasculature in the dermis. [3] It is a safe alternative to conventional ablative lasers, especially in darker skin types, although the efficacy is not comparable to conventional ablative CO 2 laser or Erbium:YAG laser. [10]
References
- Ruiz-Esparza J, Gomez JB. The medical facelift: A noninvasive, nonsurgical approach to tissue tightening in facial skin using nonablative radiofrequency. Dermatol Surg 2003;29:325-32.
- Sadick N, Alexiades-Armenakas M, Bitter P, Hruza G, Mulholland S. Enhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted, bipolar radiofrequency energy (ELOS): Introducing selective radiophotothermolysis. J Drugs Dermatol 2005;4:181-6.
- Bjerring P, Clement M, Heickendorff L, Lybecker H, Kiernan M. Selective non-ablative wrinkle reduction by laser. J Cutan Laser Ther 2002;4:39-43.
- Alam M, Hsu TS, Dover JS, Wrone DA, Arndt KA. Nonablative laser and light treatments: Histology and tissue effects- a review. Lasers Surg Med 2003,33:30-9.
- Cassuto DA, Emanuelli G. Non-ablative scar revision using a long pulsed frequency doubled Nd:YAG laser. J Cosmet Laser Ther 2003;5:1-5.
- Lefell DJ. Clinical efficacy of devices for nonablative photorejuvenation. Arch Dermatol 2002;20:97-111.
- Chan HH. Effective and safe use of lasers, light sources, and radiofrequency devices in the clinical management of Asian patients with selected dermatoses. Lasers Surg Med 2005;37:179-85.
- Min SU, Choi YS, Lee DH, Yoon MY, Suh DH. Comparison of a long-pulse Nd:YAG laser and a combined 585/1,064-nm laser for the treatment of acne scars: A randomized split-face clinical study. Dermatol Surg 2009;35:1720-7.
- Kim S, Cho KH. Clinical trial of dual treatment with an ablative fractional laser and a non ablative laser for the treatment of acne scars in Asian patients. Dermatol Surg 2009;35:1-10.
- Goldberg DJ. Nonablative dermal remodeling: Does it really work? Arch Dermatol 2002;138:1366-8.
Selection of Appropriate Lasers
Laser technology is constantly changing and newer technologies are emerging on a regular basis. It is important to understand that there is no ideal laser, and depending on one′s patient profile and requirements, a choice of machine can be made. [1] It is not the mandate of the taskforce to make recommendations of individual machines. Hence, a prospective buyer should carefully look at different parameters before making a choice. The available systems and their parameters are listed below in [Table - 1].

Extensive study should be done prior to purchasing a machine, and a complete understanding of laser physics is a pre-requisite in order to make an informed choice. The parameters to be considered should include: [2]
- Clinical efficacy of the technology
- Safety on Indian skin types
- Practicality of use, including patient comfort, downtime, ease of treatment, and risk of post operative complications
- Cost of the technology
- Reliability of the manufacturer and distributor, including service back-up.
Indications
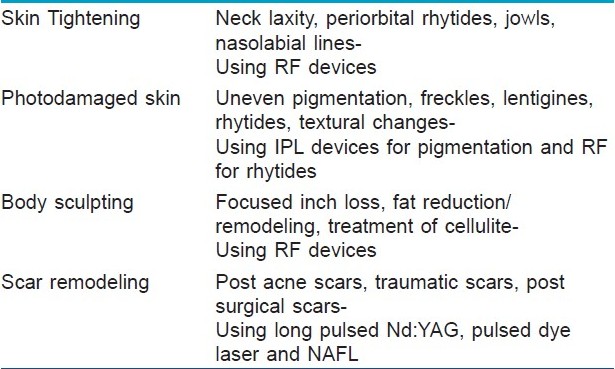
Nonablative technology have been used for several indications such as skin tightening, periorbital tissue tightening, treatment of nasolabial lines and jowl, body sculpting/remodeling, cellulite reduction, scar revision and remodeling and for the treatment of photodamaged skin. [3],[4] The conditions, which can be treated by nonablative lasers are listed in [Table - 2].
Skin tightening
Nonablative technologies stimulate collagen fiber synthesis to reduce wrinkles and lax skin. The goal is to achieve skin tightening without the creation of an epidermal wound, thereby minimizing the morbidity and recovery time. Higher treatment fluences generally lead to improved or more consistent results. The greater the surface area treated, the better are the results.
Periorbital tissue tightening
Radiofrequency and other nonablative laser and light systems are a nonsurgical alternative for the correction of periorbital rhytides and skin laxity, provided that proper patient selection and management of expectations is achieved. It is ideal for patients with milder cutaneous pathology, or in those who are unwilling or unable to undergo a labour-intensive procedure like blepharoplasty, which is associated with considerable postoperative morbidity. [5]
Treatment of nasolabial lines and jowl
Nonablative technologies work best in patients in their 30s to 60s, who have medium quality skin thickness and mild to moderate jawline and neck laxity. [6] Treating the areas on and adjacent to the described laxity may also improve response rate. The thyroid region of the anterior neck must be clearly demarcated and excluded from treatment. [7] Younger age is a predictor for increased efficacy.
References
- Arnoczky SP, Aksan A. Thermal modification of connective tissues: Basic science considerations and clinical implications. J Am Acad Orthop Surg 2000;8:305-13.
- Marmur ES, Goldberg DJ. Nonablative skin resurfacing. In: Goldberg DJ, Dover SJ, editors. Lasers and Lights. 2nd ed, vol 2. Philadelphia: Elsevier; 2008. p. 43-54.
- Glogau RG. Chemical Peeling and ageing skin. J Geriatric Dermatol 1994;2:5-10.
- Glogau RG. Aesthetic and anatomic analysis of the ageing skin. Semin Cutan Med Surg 1996;15:134-8.
- Fitzpatrick R, Geronemus R, Goldberg D, Kaminer M, Kilmer S, Ruiz-Esparza J. Multicenter study of noninvasive radiofrequency for periorbital tissue tightening. Lasers Surg Med 2003;33:232-42.
- Hsu TS, Kaminer MS. The use of non-ablative radiofrequency technology to tighten the lower face and neck. Semin Cutan Med Surg 2003;22:115-23.
- Jacobson LG, Alexiades-Armenakas M, Bernstein L, Geronemus RG. Treatment of nasolabial folds and jowls with a noninvasive radiofrequency device. Arch Dermatol 2003;139:1371-2.
Body sculpting and cellulite reduction
A wide variety of devices are being evaluated to help improve the appearance of cellulite as well as in the recontouring of body fat. The proposed mechanism of action consists of increased tissue perfusion and mobilization of lymphatic drainage from mechanical manipulation of the skin combined with low level laser irradiation, and reduction in tissue edema due to contact cooling, thereby resulting in the improved appearance of cellulite. [1] Improvement includes reduction in the appearance of skin dimpling, improvement in the overall contour of the limb and improvement in overall skin texture. [2] There are no changes reported in blood lipid analysis. Bruising is the most commonly noted adverse effect. [2] There are no published studies comparing the efficacy of laser and lights systems to results achieved through lipolysis. Presently, therefore, it is difficult to make any recommendations about the use of these machines for body sculpting and cellulite reduction.
References
- Sadick NS, Mulholland RS. A prospective clinical study to evaluate the efficacy and safety of cellulite treatment using the combination of optical and RF energies for subcutaneous tissue heating. J Cosmet Laser Ther 2004;6:187-90.
- Reynaud JP, Skibinski M, Wassmer B, Rochon P, Mordon S. Lipolysis using a 980-nm diode laser: a retrospective analysis of 534 procedures. Aesth Plast Surg 2009:33:28-36.
Scars and acne scar remodeling-
Various nonablative devices have been used for acne scar remodeling as well as the correction of postsurgical and post-traumatic scars. The results are visibly less dramatic compared to fractional and ablative laser systems, although it is well established that nonablative lasers have a better safety profile in darker skin types. [1] When the aesthetic drawback is mainly a result of hypervascularity and hyperpigmentation, these problems can be specifically targeted using devices with wavelengths that are well absorbed by both the melanin and well as the hemoglobin chromophore. [1],[2] Some degree of epidermal tightening is also achieved, which is useful in the treatment of atrophic scars. The results are progressive and can continue to improve months after the laser treatment has been completed.
References
-
Min SU, Choi YS, Lee DH, Yoon MY, Suh DH. Comparison of a long-pulse Nd:YAG laser and a combined 585/1,064-nm laser for the treatment of acne scars: A randomized split-face clinical study. Dermatol Surg 2009;35:1720-7.
- Kim S, Cho KH. Clinical trial of dual treatment with an ablative fractional laser and a non ablative laser for the treatment of acne scars in Asian patients. Dermatol Surg 2009;35:1-10.
Photodamage
Nonablative skin resurfacing is ideally used for the patient with mild-to-moderate photodamage and signs of skin ageing including lentigenes, mild rhytides and mild to moderate poikiloderma. Patients with advanced photoageing or more severe skin sagging may also benefit from these treatments, but possibly to a lesser extent. [1],[2],[3]
References
- Sadick N, Alexiades-Armenakas M, Bitter P, Hruza G, Mulholland S. Enhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted, bipolar radiofrequency energy (ELOS): Introducing selective radiophotothermolysis. J Drugs Dermatol 2005;4:181-6.
- Goldberg DJ. Nonablative dermal remodeling: Does it really work? Arch Dermatol 2002;138:1366-8.
- Bjerring P, Clement M, Heickendorff L. Selective non-ablative wrinkle reduction by laser. J Cutan Laser Ther 2000;2:9-15.
Recommendations
Physician qualification
A basic dermatology degree namely Diploma (DVD) or Masters Degree (MD) in Dermatology Venereology and Leprology is a pre-requisite. Specific training under an experienced and qualified practitioner is necessary for proper understanding and use of the technology. It is also important to be involved in continuing medical education on newer systems and newer techniques by attending lectures, workshops and conferences on a regular basis
Facility
Nonablative laser and light modalities can be carried out in a physician treatment room, or a hospital or nursing home setting with a small operation theater. The room must be a dedicated laser room with standard size adequate ventilation and air-conditioning, smoke evacuator and a full length patient bed. For further information on guidelines of requirements for setting up a laser room, refer to Indian J Dermatol Venereol 2009;75(Suppl 2):101-10.
Patient selection
Detailed examination should be performed. The dermatologic consultation should include detailed assessment of the patient′s skin condition and skin type. An informed consent is mandatory to protect the rights of the patient as well as the practitioner (please check APPENDIX).[SUPPORTING:1] All patients must have carefully taken preoperative and postoperative pictures.
- Optimal candidate is in his/her mid 30s to mid 60s with some sagging of jowls and neck, but lacks the need for surgical lifting procedure. Patients who are concerned about risk of more aggressive treatments, recovery time, and are willing to accept minimal efficacy in exchange for minimal risk are the ideal candidates for nonablative approaches. [1]
- Nonablative skin tightening devices are of negligible benefit to obese patients and patients with extreme skin redundancy.
- These lasers can be used safely on patients who have had prior cosmetic procedures, including rhytidectomy, laser surgery, fillers and botox. [2] A combination or sequential therapy approach to treating the complete face or area is recommended. It is advisable to do laser treatments and/or botox and fillers on separate occasions with a minimum of 15 days gap.
- For those who have been treated previously with nonablative RF devices or the ELOS system, it is preferable to wait at least 3 months before initiating them on a Thermage or AFT system. [1] This is because the tightening effects of Nonablative Radiofrequency (NARF) continues for months following treatment with the device.
- Use in patients with pacemakers is contraindicated. In addition, care should be taken to obtain history of any metal implants, braces or hardware. [3] Treatment should be avoided overlying these areas.
- Do not treat pregnant women or lactating women.
- In patients with history of recurrent herpes or staphylococcal infections, a course of antiviral/antibacterial prophylaxis is advised. [4]
- In patients with a history of keloidal tendency, a conservative approach is advised.
- It is important to discuss specific concerns of the patient and their expectations from the treatment. Patient must be given reading material on the procedure to be undertaken, as patients are likely to forget a lot of what is discussed in the consultation room. It is advisable not to undertake a procedure on the same day of the initial consult. Make referrals to other doctors, especially plastic surgeons when necessary. A psychiatric consult must also be advised when deemed necessary.
All patients should have preoperative photography. Standardized photography in the same room with the same lighting using a 10-megapixel camera in the same position must be obtained.
Preoperative preparation
- Thorough cleansing of the area to be treated with a mild acetone-based cleanser to facilitate adequate degreasing of the skin.
- Patients must be asked to protect against sun exposure for 1−2 weeks prior to treatment. Alternatively, a tanned patient can also be pretreated with hydroquinone twice daily for a month before the treatment. This may also help to minimize post-treatment inflammatory hyperpigmentation, particularly in patients with darker skin types. [4]
- Preoperative pictures must be taken with a high-resolution camera, from the front, from the sides, and at three-quarter turns.
Intraoperative strategies
- Coupling fluid (transparent ultrasound gel) is applied generously to the area to be treated (Level D). If the philtrum and upper lip is to be treated, the teeth are protected by wet gauze placed between the teeth and the upper lip. [5]
- Eye protection is a must for patient, treating physician and any other assistant/nurse.
- Use lower energies and fewer passes for the neck areas. This is due to the higher vascularity of this region, leading to faster heating and early erythema and edema. [5]
- Constantly evaluate the skin for signs of tightening and edema. This is an important and expected clinical end point, and it correlates with clinical efficacy. Patient tolerance is also an important indicator, so the physician must be constantly engaged with the patient during the procedure.
- Dynamic or in-built cooling devices allow higher fluences to be applied more safely. Cooling is particularly helpful in the treatment of darker skin types.
Postoperative care
- The nonablative lasers, light sources, and RF systems discussed within the purview of this article are very safe, even in darker skin-types, and post operative care is minimal. Application of icepacks or gauze soaked in cold water helps in soothing the skin and faster resolution of erythema and edema.
References
- Weiss RA, Weiss MA, Munavalli G, Beasly KL. Monopolar radiofrequency facial tightening: A retrospective analysis of efficacy and safety in over 600 treatments. J Drugs Dermatol 2006;5:707-12.
- Alam M, Levy R, Pavjani U, Ramierez JA, Guitart J, Veen H, et al. Safety of radiofrequency treatment over human skin previously injected with medium-term injectable soft tissue augmentation materials: A controlled pilot trial. Lasers Surg Med 2006;38:205-10.
- Arnoczky SP, Aksan A. The mal modification of connective tissues: Basic science considerations and clinical implications. J Am Acad Orthop Surg 2000;8:305-13.
- Fisher GH, Geronemus RG. Short-term side effects of fractional photothermolysis. Dermatol Surg 2005;31:1245-9.
- Handley JM. Adverse events associated with nonablative cutaneous visible and infrared laser treatment. J Am Acad Dermatol 2006;55:482-9.
Complications
- Most patients experience mild erythema and edema immediately post procedure, which resolves within several hours. [1]
- Rarely, patients may complain of tenderness or temporary dysesthesia. [2]
- Vesiculation may occur in patients with history of flushing and rosacea, and may be prevented by premedication with antihistamines. In event of vesiculation, patient is advised to apply a petroleum based ointment, twice daily, till lesions heal. Vesicles heal without pigmentation or scarring in most cases. [3],[4]
- Risk of post inflammatory hyperpigmentation and scarring. [3],[4]
References
- Weiss RA, Weiss MA, Munavalli G, Beasly KL. Monopolar radiofrequency facial tightening: A retrospective analysis of efficacy and safety in over 600 treatments. J Drugs Dermatol 2006;5:707-12.
- Marmur ES, Goldberg DJ. Nonablative skin resurfacing. In: Goldberg DJ, Dover SJ, editors. Lasers and Lights. 2nd ed, vol 2. Philadelphia: Elsevier; 2008. p. 43-54.
- Alexiades-Armenakas MR, Kaminer MS. Skin tightening with radiofrequency. In: Goldberg DJ, Dover SJ, editors. Lasers and Lights. 2nd ed, vol 2. Philadelphia: Elsevier; 2008. p. 55-72.
- Handley JM. Adverse events associated with nonablative cutaneous visible and infrared laser treatment. J Am Acad Dermatol 2006;55:482-9.
Summary
The use of nonablative technology is proving to be one of the treatments of choice in skin rejuvenation. The choice of technology and settings in darker skin types is important, in order to prevent post-inflammatory hyperpigmentation. Combination treatments for anti-ageing are recommended, and there is no single gold standard therapy.
Fulltext Views
6,658
PDF downloads
3,101





