Translate this page into:
Novel glycine substitution G2037R of COL7A1 in a Chinese boy with pretibial epidermolysis bullosa treated with oral olopatadine hydrochloride and topical Vitamin E
2 Department of Dermatology, Shenzhen Hospital, Southern Medical University, Shenzhen, Guangdong 518000, China
Correspondence Address:
Yanhua Liang
Department of Dermatology, Shenzhen Hospital, Southern Medical University, 1333 Xinhu Road, Shenzhen, Guangdong 518000
China
| How to cite this article: Chen J, Liang Y. Novel glycine substitution G2037R of COL7A1 in a Chinese boy with pretibial epidermolysis bullosa treated with oral olopatadine hydrochloride and topical Vitamin E. Indian J Dermatol Venereol Leprol 2017;83:229-231 |
Sir,
Epidermolysis bullosa has been divided into distinct subtypes depending on the level of tissue separation in the dermal-epidermal basement membrane zone; mainly classified as epidermolysis bullosa simplex, junctional epidermolysis bullosa and dystrophic epidermolysis bullosa.[1] The site-specific structural abnormalities are correlated to the genetic dysfunction of different genes, such as K5/K14 mutations in epidermolysis bullosa simplex, mutations of laminins in junctional epidermolysis bullosa and COL7A1 mutations in dystrophic epidermolysis bullosa. So far, only six mutations have been detected in pretibial dystrophic epidermolysis bullosa, according to the literature.[2],[3] We found a novel glycine substitution mutation (G2037R) in exon 73 in a sporadic pretibial dystrophic epidermolysis bullosa patient, whose symptoms were well controlled with a combination treatment regime of oral olopatadine hydrochloride and topical Vitamin E.
An 11-year-old Chinese boy presented to the dermatology clinic with multiple bullous lesions of approximately 0.5–1 cm size, on the abdomen and back; Nikolsky's sign was positive. Several tense and clear blisters, scars and small erosions were also found on the skin around the ankle, knee, hip, elbow and finger joints [Figure 1a]. Some nails were fragile, disfigured and some were absent. His teeth were irregularly arranged, defective or absent [Figure 1b]. Biopsy from a flat papule on the left shin revealed epidermal hyperkeratosis, keratin cysts, irregular acanthosis, hyperplasia and subepidermal cleft formation containing a mild-to-moderate perivascular and interstitial eosinophilic, neutrophil and lymphocytic infiltrate within the proliferative collagen fibers in the papillary dermis [Figure 1c].
 |
| Figure 1a: Clinical presentation and histological features. Relaxed blisters and scars scattered on hands |
 |
| Figure 1b: His teeth are irregularly positioned and/or absent |
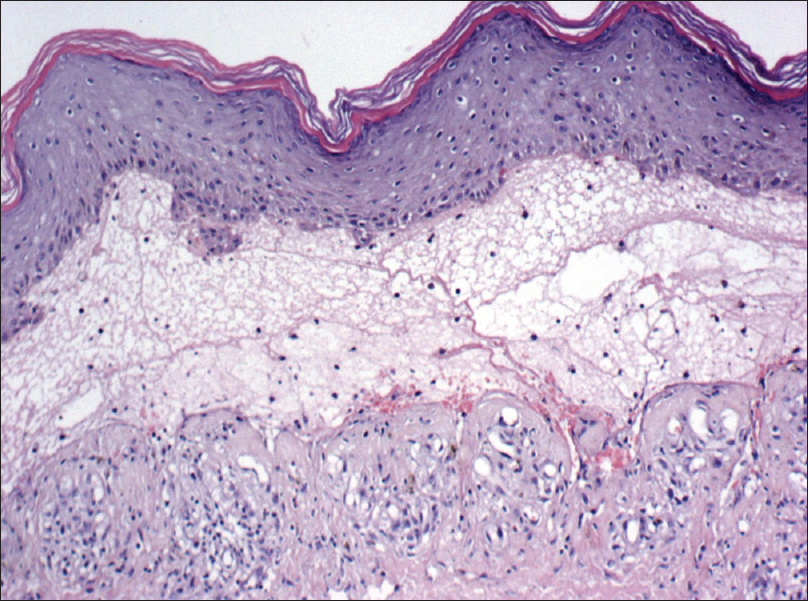 |
| Figure 1c: H and E staining revealed epidermal hyperkeratinization, subepidermal bulla formation and infiltration of numerous inflammatory cells (×100, 100 μm) |
After starting treatment with oral olopatadine hydrochloride and topical Vitamin E, the pruritus was well controlled, as evidenced by reduced excoriations at the lesional sites. After 2 weeks of treatment, new blisters no longer appeared and the older lesions showed signs of healing. In addition, the nails became clearer and the skin became more smooth and elastic [Figure 1d].
 |
| Figure 1d: The cutaneous lesions were much improved after 5-month treatment with olopatadine and Vitamin E |
Genetic studies were performed on the patient and a heterozygous missense mutation was identified in the proband by directly sequencing the polymerase chain reaction products, designated as c. 6109 G>A or p.G2037R in exon 73 of COL7A1 gene [Figure - 2]a. His parents carried an unaffected homozygous allele [Figure - 2]b. The mutation G2037R was not found in his parents and 100 unrelated, unaffected control individuals. This mutation is predicted to be “probably damaging” with a score of 1.000 by polyphen-2 (polymorphism phenotyping-2 http://genetics.bwh.harvard.edu/pph 2/). A three-dimensional molecular modeling of the mutant COL7A1 protein was predicted by a web-based software I-TASSER (University of Kansas, Lawrence, Kansas, USA) [Figure - 3].
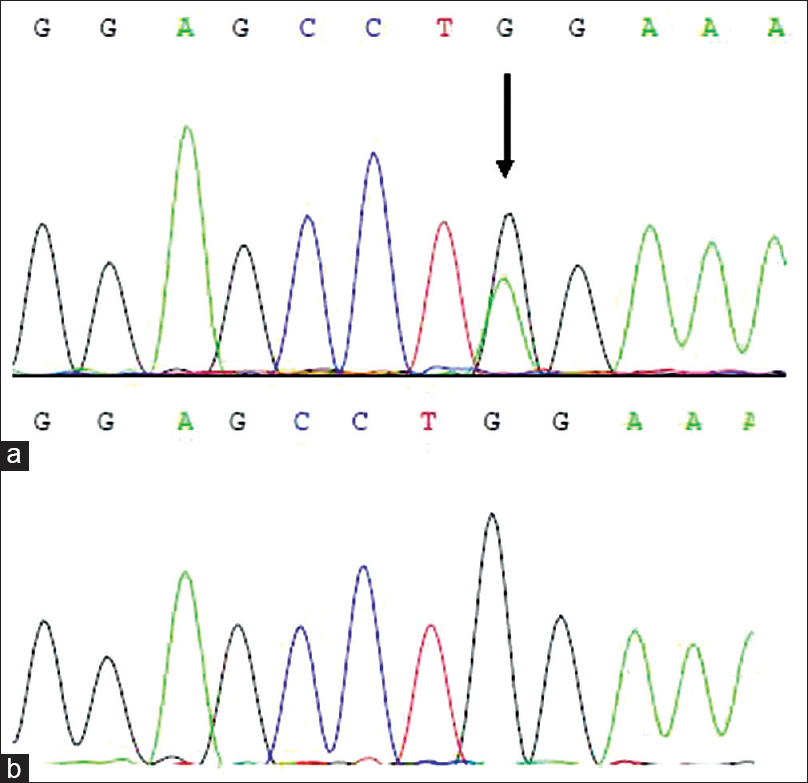 |
| Figure 2: Detection of COL7A1 mutation. (a) After direct sequence analysis of 118 exons and exon-intron boundary of COL7A1 gene, a nucleotide substitution was found in exon 73 of the patient, designated as c. 6109G>A, causing change of the 2037th amino residue from glycine (GGA) to arginine (AGA). (b) The same genomic change were not seen in a population of matched, unrelated healthy controls |
 |
| Figure 3: The three-dimensional molecular modeling of the mutant COL7A1 protein |
Herein, we studied a Chinese case with pretibial dystrophic epidermolysis bullosa, where the proband was found to have a heterozygous glycine substitution p. Gly2037Arg. We also found that the combination of olopatadine hydrochloride and topical Vitamin E was effective in reducing the itch and helped in achieving disease control.
Financial support and sponsorship
This work was supported by a grant from National Natural Science Foundation of China (81371724) to Yan-Hua Liang.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Fine JD, Eady RA, Bauer EA, Bauer JW, Bruckner-Tuderman L, Heagerty A, et al. The classification of inherited epidermolysis bullosa (EB): Report of the Third International Consensus Meeting on Diagnosis and Classification of EB. J Am Acad Dermatol 2008;58:931-50.
[Google Scholar]
|
| 2. |
Hamada T, Fukuda S, Ishii N, Abe T, Nagata K, Koro O, et al. A Japanese family with dominant pretibial dystrophic epidermolysis bullosa: Identification of a new glycine substitution in the triple-helical collagenous domain of type VII collagen. J Dermatol Sci 2009;54:212-4.
[Google Scholar]
|
| 3. |
Liu YH, Shang X, Li ZT, Wu YM, Li LF, Xu XM. A novel COL7A1 gene mutation causing pretibial epidermolysis bullosa: Report of a Chinese family with intra-familial phenotypical diversity. Gene 2013;524:377-80.
[Google Scholar]
|
Fulltext Views
2,740
PDF downloads
2,171





