Translate this page into:
Onychomycosis: Diagnosis and management
2 Chacha Nehru Bal Chikitsalaya, Delhi, India
Correspondence Address:
Archana Singal
B-14, Law Apartments, Karkardooma, Delhi - 110 092
India
| How to cite this article: Singal A, Khanna D. Onychomycosis: Diagnosis and management. Indian J Dermatol Venereol Leprol 2011;77:659-672 |
Abstract
Onychomycosis is a common nail ailment associated with significant physical and psychological morbidity. Increased prevalence in the recent years is attributed to enhanced longevity, comorbid conditions such as diabetes, avid sports participation, and emergence of HIV. Dermatophytes are the most commonly implicated etiologic agents, particularly Trichophyton rubrum and Trichophyton mentagrophytes var. interdigitale, followed by Candida species and non dermatophytic molds (NDMs). Several clinical variants have been recognized. Candida onychomycosis affects fingernails more often and is accompanied by paronychia. NDM molds should be suspected in patients with history of trauma and associated periungual inflammation. Diagnosis is primarily based upon KOH examination, culture and histopathological examinations of nail clippings and nail biopsy. Adequate and appropriate sample collection is vital to pinpoint the exact etiological fungus. Various improvisations have been adopted to improve the fungal isolation. Culture is the gold standard, while histopathology is often performed to diagnose and differentiate onychomycosis from other nail disorders such as psoriasis and lichen planus. Though rarely used, DNA-based methods are effective for identifying mixed infections and quantification of fungal load. Various treatment modalities including topical, systemic and surgical have been used.Topically, drugs (ciclopirox and amorolfine nail lacquers) are delivered through specialized transungual drug delivery systems ensuring high concentration and prolonged contact. Commonly used oral therapeutic agents include terbinafine, fluconazole, and itraconazole. Terbinafine and itraconazole are given as continuous as well as intermittent regimes. Continuous terbinafine appears to be the most effective regime for dermatophyte onychomycosis. Despite good therapeutic response to newer modalities, long-term outcome is unsatisfactory due to therapeutic failure, relapse, and reinfection. To combat the poor response, newer strategies such as combination, sequential, and supplementary therapies have been suggested. In the end, treatment of special populations such as diabetic, elderly, and children is outlined.Introduction
Onychomycosis is a common condition affecting 5.5% of the population worldwide and represents 20-40% of all onychopathies and about 30% of cutaneous mycotic infections. [1] Onychomycosis of fingernails may lead to pain, discomfort, and impaired/lost tactile functions. Toenail dystrophy can interfere with walking, exercise, or proper shoe fit. In addition, onychomycosis has both psychosocially and physically detrimental effects.
Prevalence
The prevalence of onychomycosis is determined by age, occupation, climate, and frequency of travel. Increase in the aged population, HIV infection or immunosuppressive therapy, avid sports participation, commercial swimming pools, and occlusive foot wear are responsible for an increased incidence. [1],[2] Men are affected more frequently possibly due to more frequent nail damage from sports and leisure activities. [1] Toe nails are about seven times more frequently affected than fingernails due to three times slower growth rate. [2] Walking barefoot, wearing ill-fitting shoes, nail biting (onychophagia), and working with chemicals further predispose Indian patients to onychomycosis. [3]
Other predisposing factors include nail trauma, peripheral vascular disease (PVD), smoking, and psoriasis. [1],[2]
Etiology
There is a wide variety of fungi causing onychomycosis which varies from one geographic area to another primarily due to different climatic conditions. [3]
Dermatophytes are the most frequently implicated causative agents in onychomycosis (approximately 90% in toenail and 50% in fingernail). Dermatophyte invasion of the nail plate is termed tinea unguium. Trichophyton rubrum (T. rubrum) is the most common causative agent followed by T. mentagrophytes. [1]
Nondermatophyte molds (NDM) mainly affect toenails and occasionally fingernails. NDM account for 1.5-6% of all onychomycosis that fall into two main categories: first group encompasses fungi that are nearly always isolated from nails as etiologic agents, such as Scytalidium dimidiatum and Scytalidium hyalinum; the second group is formed by opportunistic fungi that may also be isolated as contaminants, such as Scopulariopsis brevicaulis, Aspergillus sydowii, and Onychocola canadensis. [1] Certain NDM such as Acremonium species can invade the nail surface, while others such as Scytalidium species are more often associated with distal and lateral subungual onychomycosis. [1],[4] Molds are considered pathogens when the following criteria are fulfilled:
- Nail abnormalities consistent with diagnosis.
- Positive direct microscopy visualizing hyphae in the nail keratin.
- Failure to isolate a dermatophyte in the culture
- Growth of more than five colonies of the same mold in at least two consecutive nail samplings. [5]
Involvement of molds should be suspected in the absence of tinea pedis, history of trauma, presence of one or two affected toe-nails with periungual inflammation. [1]
Yeasts: Previously regarded as contaminants, yeasts are now increasingly recognized as pathogens in fingernail infections. Candida albicans accounts for 70% of cases, while C. parapsilosis, C. tropicalis, and C. krusei account for the remainder. Candida onychomycosis (CO) is increasingly found in individuals with defective/lowered immunity consequential to aging, diabetes, vascular diseases, immunosuppression, and broad spectrum antibiotics, and is common in patients with DiGeorge syndrome, agammaglobulinemia, and thymus dysplasia. [6] Chronic exposure to moisture and chemicals including detergents and breached local immunity due to trauma, as seen in housewives, farmers, and fishermen, contributes to CO accompanied by Candida paronychia. [6] Candida can be a primary or secondary pathogen. Its role as a primary pathogen is almost always seen in severe immunosuppression such as HIV infection and chronic mucocutaneous candidiasis (CMC), while secondary invasion by Candida occurs in cases with PVD, malnutrition, and compromised local immunity at the nail complex. [6] Keratin in the nail substance is known to act as an excellent growth environment for virulent Candida strains. [6]
Clinical Features
There are five major clinical presentations of onychomycosis:
- Distal and lateral subungual onychomycosis (DLSO)
- Proximal subungual onychomycosis (PSO)
- Superficial white onychomycosis (SWO)
- Endonyx
- Total dystrophic onychomycosis (TDO)
Distal and lateral subungual onychomycosis
DLSO is the commonest clinical variant affecting both finger and toenails. The fungus enters via the distal subungual and lateral nail groove, invades the horny layer of the hyponychium and/or nail bed, and spreads proximally against the stream of nail growth and subsequently through the under surface of nail plate which becomes opaque. Clinically, there is onycholysis and subungual hyperkeratosis [Figure - 1] which acts as a mycotic reservoir for fungal proliferation. [1] The commonest causative species is T. rubrum followed by T. mentagrophytes, T. tonsurans, and Epidermophyton floccosum. ′One hand two feet′ tinea syndrome is a distinct clinical pattern in DLSO caused by T. rubrum in which the fungus spreads from the plantar and palmar surface of feet and hands [Figure - 2]. Chronic dermatophytosis syndrome, caused by T. mentagrophytes var. interdigitale starts as minute plantar vesicles of 1 mm size and collarettes over the soles that are the site of abundant hyphae. The vesicles dry leaving a keratinous collarette and later on other sites become infected, especially the nail bed, leading to DLSO. [2]
 |
| Figure 1: Distal and lateral subungal onychomycosis |
 |
| Figure 2: One hand two feet' tinea syndrome |
Proximal subungal onychomycosis
Proximal subungal onychomycosis (PSO) is a relatively uncommon subtype described with increased frequency in patients with AIDS. It affects fingernails and toenails equally and is usually caused by T. rubrum, with exceptional reports implicating T. megnini, T. schoenleinii, and Epidermophyton floccosum. [2] The fungus first appears from below the proximal nail fold, migrates to the underlying matrix, and then spreads distally under the nail plate. Infection occurs within the substance of the nail plate, but the surface remains intact. Clinically, there is subungual hyperkeratosis, transverse leukonychia, and proximal onycholysis [Figure - 3] and eventually destruction of the proximal nail plate. [1] Periungual inflammation may be marked, painful, and associated with purulent discharge.
 |
| Figure 3: Proximal subungual onychomycosis |
Superficial white onychomycosis
SWO is a distinctive pattern mainly affecting toenails, in which the nail plate is the primary site of invasion. T. mentagrophytes var. interdigitale is responsible for most cases (> 90%). It may be caused by T. rubrum and sometimes by NDM such as Acremonium species, Aspergillus terreus, and Fusarium oxysporum. Clinically, small well delineated opaque white islands are present on the dorsal nail plates [Figure - 4] which coalesce resulting in a rough and crumbly appearance of the nail. [1] SWO usually affects a single toe nail and may show a diffuse involvement of the nail. The nail becomes friable and diffusely opaque with variable pigmentation. In children, nail may become homogenously white, opaque, and flexible. SWO caused by Candida species affecting several fingernails and toenails has been seen in premature infants born to mothers with vaginal candidiasis. [1],[6] Baran et al., [7] have proposed a classification of SWO as: classical SWO; dual invasion of the nail plate, superficial and ventral; and the pseudo-SWO with deep fungal invasion of the nail plate. [7]
 |
| Figure 4: Superficial white onychomycosis caused by nondermatophtytic molds |
Endonyx
Endonyx onychomycosis is invasion of the nail plate where the infection starts from the pulp as in DLSO, but instead of infecting the nail bed, the fungus penetrates the distal nail keratin of nail plate where it forms milky white patches without subungual hyperkeratosis or onycholysis. It has been described with T. soudanense and T. violaceum infections.
Total dystrophic onychomycosis
There is total destruction of the nail plate where the nail crumbles and disappears leaving a thickened abnormal nail bed retaining keratotic nail debris [Figure - 5]. It may occur secondarily as the end result of any of the four main patterns. Primary TDO is observed only in patients suffering from CMC or the immunodeficient states where the thickening of the soft tissues results in a swollen distal phalanx that is more bulbous than clubbed and the nail plate is thickened, opaque, and yellow brown in color.
 |
| Figure 5: Total dystrophic onychomycosis of left big toe |
Candida onychomycosis
It commonly affects fingernails and nearly half of the fingernail-related onychomycosis are due to Candida species. [6] CO is more commonly reported in women possibly due to self inoculation of nails from vaginal Candida flora. Frequent handling of water and soap during household work may also be contributory. [6] CO may present in the following ways:
Candida paronychia: In most cases of CO, invasion of the nail plate occurs secondarily via soft tissues around the nail. There is painful swelling and erythema of the proximal and lateral nail folds. Infection of the nail matrix results in transverse depressions known as Beau′s lines in the nail plate [Figure - 6]. The end result is a rough, irregular, convex, and finally dystrophic nail. [1],[6] There is no subungual hyperkeratosis and the nail does not crumble away as in TDO.
 |
| Figure 6: Candida onychomycosis of long duration with paronychia |
Candida granuloma: This is an uncommon presentation seen primarily in patients with CMC and characterized by invasion of the full thickness of the nail by Candida. [6] Progressive thickening of the nail and swelling of the proximal and lateral nail folds may cause digit deformity called pseudoclubbing or chicken drumstick appearance.
Candida onycholysis: In this entity, distal subungual hyperkeratosis with a yellowish grey mass lifts off the nail plate with resultant onycholysis.
Diagnosis of Onychomycosis
The clinical presentation of onychomycosis may provide clues to the infecting organism; however, at times, appearance caused by different fungal species may be indistinguishable. It is important to identify the causative fungus before initiating treatment, because some therapies are more effective against certain organisms than others.
Specimen collection: Proper specimen collection is essential to avoid false negative results and to eliminate contaminants. Separate samples should be obtained from fingernails and toenails, associated tinea pedis, or manuum. [2] The specimen should be obtained when the patient has been off both topical and systemic antifungal drugs for 2-4 weeks. Fine shavings or minute clippings are preferred. Specimens must not be kept in moist media to avoid rapid multiplication of bacterial and fungal spores and should be processed within a week. [1]
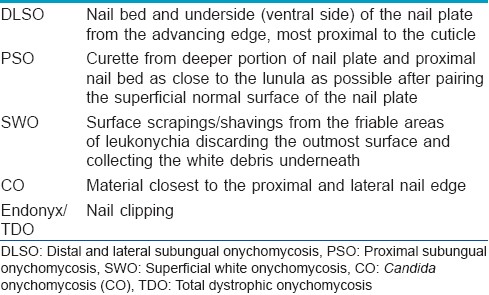
The entire nail unit should be thoroughly cleaned with alcohol. The affected nail bed should be exposed by removing the onycholytic nail plate with a nail clipper and scraping the hyperkeratotic nail bed with a solid or disposable scalpel or curette and outermost debris should be discarded. [2] Sampling of distal nail plate should be avoided as it frequently contains contaminants that may obscure the growth of pathogenic fungi. Preferred sites for sample collection in different clinical variants are listed in [Table - 1].
Direct microscopy is the quickest and easiest technique to confirm fungal nail infection. The specimen can be mounted in a solution of 10-30% KOH or NaOH mixed with 5% glycerol, warmed to emulsify lipids and examined first under 10× and then under 40× magnification. An alternative formulation consists of 20% KOH and 36% DMSO, which provides a rapid method of diagnosis of mycosis without heating and specimens last longer for re-examination. [2] The nail is examined for fungal hyphae, arthrospore or yeast forms. Fungal elements should be differentiated from artefacts including lipid vesicles, air bubbles, muscle fibers, and mosaic fungi. [2] The specimen may be counterstained with chlorazol black or Parkers blue ink. Chlorazol accentuates the hyphae by staining the carbohydrate rich wall without staining potential contaminants such as cotton or elastic fibers. Calcofluor white (CW), a fluorescent dye, which also stains chitin in the fungal cell wall, has a sensitivity of 92% and specificity of 95%, but requires a fluorescent microscope. [8] Direct microscopy establishes the presence or absence of fungi, but cannot identify the specific fungus or differentiate viable from nonviable fungi.
Culture is essential for confirming the diagnosis and ascertaining the exact etiologic fungus. Half of the specimen should be sent for culture even when direct microscopy is negative. Different media used for culturing nail specimens include:
- Primary medium - containing cycloheximide against most NDM and bacteria, e.g., DTM , mycosel (BBL), and mycobiotic (DIFCO)
- Secondary media such as Sabouraud glucose agar (SGA), Littman′s Oxgall medium, and potato dextrose agar (PDA) that are free of cycloheximide and allow isolation of NDM. Antibiotics such as chloramphenicol and gentamicin may be added to SGA or PDA to eliminate bacterial contamination. Specimens should be incubated at 25-30°C. [1]
NDM grow faster than dermatophytes and produce well-formed colonies within 1 week. Colonies of most dermatophytes are usually completely differentiated in 2 weeks. All plates should be kept for a minimum of 2 weeks and absence of growth after 3-6 weeks should be interpreted as negative. Though considered gold standard for diagnosis, culture takes a longer time and yield of positive culture is often disappointing. False-negative results may be seen with inadequate and inappropriate nail sampling. The nail specimen must be crushed thoroughly to ensure fungal growth. [9]
Various improvisations have been adopted for sample collection to improve fungal yield. Shemer et al., [10] found higher culture sensitivity when the sample was obtained using a driller as compared to curettage and from a more proximal location. [10] Drilling can be done subungually through the nail plate to obtain proximal nail material but may cause transient deformation of the nail. [10] False-negative results are observed in about 10% of nail specimens under KOH microscopy and 20-35% of cultures. Identification of a particular fungus does not ensure its pathogenic role especially in case of saprophytic fungi. Pure growth of a dermatophyte is easily identified; however, the presence of yeasts or mold colonies may or may not constitute mixed infection.
Histopathology : Histopatholgy of nail specimens may be necessary when KOH and culture are repeatedly negative in patients with suspected onychomycosis. Nail biopsy is also helpful in differentiating nonmycotic onychodystrophy caused by psoriasis and lichen planus, but can cause permanent nail dystrophy. Alternatively, nail plate clipping may be sent in a 10% buffered formalin container for histopathological analysis with Periodic Acid Schiff (PAS) staining. PAS stains glycogen and mucoproteins in the fungal cell wall and was found to be more sensitive than KOH preparation and culture alone (92% vs. 80% or 59%, respectively). [9] Grocott Methenamine silver and calcofluor white (CFW) stains are more selective than PAS. However unlike culture, histopathology cannot differentiate between viable or nonviable organisms nor does it help to identify the particular pathogen. [1,9] Vital stains such as neutral red can help in distinguishing between viable and nonviable elements. [1] The latter however can only be performed on fresh smears from subungual hyperkeratosis and from scrapings of SWO. [4]
No fixative or transport media are required for histopathology samples obtained by nail clipping, that can be processed easily with limited number of serial sections within 3-5 days. In addition, full thickness lamina, location, and invasiveness of the fungus can be clearly observed, thus establishing a pathogenic role to a particular isolate. Histopathological processing and PAS-stained nail clipping can give results as good as nail biopsy and is faster, painless, and economical. [4],[11]
Other less frequently used tests to diagnose onychomycosis include immunohistochemistry and dual flow cytometry especially for identifying mixed infections and for quantification of fungal load in the nail. DNA-based methods such as PCR-RFLP assays have been used recently for detecting fungi. [12] In one study, combination of PCR and CFW microscopy was found to be more sensitive than CFW microscopy and culture. [13] The role of scanning electron microscopy and confocal microscopy at present is primarily for research. [14]
Treatment
Onychomycosis, though considered a cosmetic problem, is a debilitating disease with immense negative physical and psychological impact. Secondly, no spontaneous clearing is known to occur. Moreover, untreated patients can act as a reservoir for family contacts and can contaminate communal bathing places. In the elderly, it can lead to cellulitis, while in diabetic patients it carries the risk of development of diabetic foot. All these factors necessitate treatment for onychomycosis. [15],[16] Despite the availability of various treatment modalities for onychomycosis, the search for an ideal antifungal drug is going on. An ideal antifungal drug should be broad spectrum, concentrate in the nail-bed and plate at levels toxic to the fungus but not to the patient, attain high cure rates with limited drug interactions and minimal side effects, and yet be economical. There is a huge disparity between the results of different drug trials targeting onychomycosis. The primary reason for this is the lack of consistency in defining and measuring cure. Secondly, efficacy assessment are often based on final evaluation at 48 to 52 weeks, while it takes around 4-6 months and 12 to 18 months for a diseased finger or toenail to be replaced, respectively. In the treatment of onychomycosis, the desired endpoints are mycological, clinical, and complete cure. Mycological cure is defined as negative microscopy and culture; clinical cure is defined as a nail without any clinical signs of onychomycosis, whereas complete cure is defined as having both mycological and clinical cure. In severe cases, up to 10% of the nail surface is likely to remain abnormal in appearance even after attainment of mycological cure. [17] Therefore, clearance of the nail plate is a more appropriate term defined either by clinical cure with 100% clearance of signs or clinical success with a residual affected nail area less than 10% with restoration of normal nail growth (at least 4 or 5 mm in 6 months) and no signs of onycholysis, hyperkeratosis, paronychia, discoloration, or fragility. [2],[16]
Treatment can be either topical, systemic, or a combination of both.
Topical therapy
Indications for topical monotherapy include:
- Involvement limited to distal 50% of nail plate, 3 or 4 nails involvement.
- No matrix area involvement.
- Superficial white onychomycosis (SWO).
- In children with thin, fast growing nails.
- As prophylaxis in patients at risk of recurrence.
- Patients where oral therapy is inappropriate.
Topical therapy should not be used if nail penetration is expected to be suboptimal. [16] Currently used topical antifungals include ciclopirox 8% and amorolfine 5% lacquers. Both have a broad action spectrum against yeasts, dermatophytes, and NDM. Lacquers are specialized transungual drug delivery systems that produce a nonwater soluble film following application and evaporation of solvent which remains in contact with the nail for long. The amorolfine concentration in the film is 25% following 5% lacquer application. Lacquer formulation helps in preventing reinfection from propagules present in shoes and also increase nail hydration by semi-occlusion, thereby limiting the formation and persistence of drug resistant fungal spores. [2] Amorolfine has been shown to persist in the nail plate significantly longer than ciclopirox, allowing a durable "reservoir effect" making once weekly application feasible. [18] The clinical efficacy of amorolfine has been reported to be 75-80%. [16] Ciclopirox is applied to the nail as a coat daily over and above the previous applications and is removed once weekly. It is FDA approved for onychomycosis with mycological cure rates of 46-85% as reported in a meta-analysis. [19] The common side-effects of nail lacquers are transient periungual erythema and burning at the application site, and a bluish or yellow brown discoloration with use of amorolfine which clears on discontinuing treatment. [20] No systemic side-effects have been reported. Topical monotherapy however carries the drawback of the need for prolonged treatment for at least 6 months to one year.
Systemic therapy
Oral therapy is recommended when:
- Involvement of > 50% of distal nail plate/ multiple nail involvement
- Involvement of nail matrix
- Topical drug penetration is expected to be suboptimal.
Oral antifungals used to treat onychomycosis include griseofulvin, azoles including ketoconazole, itraconazole and fluconazole, and allylamine terbinafine.
Griseofulvin acts by blocking the formation of mitotic spindle and is effective only against dermatophytes. It takes a long time to saturate the nail and persists in the nail for around 2 weeks after stopping therapy. [21] This necessitates prolonged administration (4-9 months and 10-18 months for finger and toenails, respectively) and results in poor compliance. Mycological cure rates are low; around 70% for fingernail and 30-40% for toenail onychomycosis, making griseofulvin the least preferred drug. The adult dose is 500 mg to 1 g daily to be administered after a fatty meal. [15]
Azole antifungals inhibit ergosterol synthesis, reduce membrane-bound enzyme activity, and interrupt chitin synthesis, making cell membrane more permeable. Ketoconazole is rarely used nowadays because of risk of severe hepatic side-effects.
Fluconazole is highly effective against both Candida and dermatophytes. It has been detected in nails within 2 weeks of starting therapy and persists in high concentrations for 3-6 months after treatment. Rapid penetration and tendency to get concentrated in keratinous structures make weekly administration sufficient. It is generally not recommended as first-line therapy because of limited data concerning its use for dermatophyte onychomycosis. Several placebo controlled studies with fluconazole monotherapy have reported mycological cure rates ranging from 36 to 100%. The cure rates were lower (31%) when compared to terbinafine (75%) and itraconazole (61%). [22] Zisova et al., [23] also reported good efficacy of 200 mg fluconazole in a weekly regime. However, they have recommended higher weekly doses (300-450 mg) when the offending agent is a NDM. [23] Scher et al., [24] reported no significant difference in the efficacy with doses of 150, 300, and 450 mg for toenail onychomycosis. [24]
A daily and alternate day 100 mg /day regimen had also been reported to be successful (80%). [2] The common adverse effects include headache, skin rash, GI complaints, insomnia, and palpitations. [21] Fluconazole inhibits both CYP3A4 and CYP2C9 and close monitoring is required when prescribing drugs metabolized by these enzymes with narrow therapeutic index. [4] Simultaneous use of fluconazole and terfenadine or cisapride is contraindicated.
Itraconazole is a triazole antifungal with the broadest spectrum of activity against dermatophytes, Candida, and NDM. It is a highly lipophilic drug and oral bioavailability is enhanced after a full meal. Itraconazole is incorporated into the nail through both matrix and nail bed and is detectable in the nail as early as seven days after starting therapy and persists for up to 6-9 months post-treatment. Rapid appearance, concentration, and persistence of itraconazole in the nail plate make the intermittent dosing regimen as efficacious as the continuous. [2] Besides, intermittent therapy is more economical, and results in higher maximum plasma concentrations and lower cumulative dose. [21] Itraconazole is given in a dose of 200 mg once daily for 3 months or preferably as pulse regime with 200 mg twice daily for a week every month. Two such pulses are given for fingernail onychomycosis and three for toenail disease. [2] Intermittent therapy has resulted in equal mycological and higher clinical cure when compared to the continuous regimen, in a multicentric randomized trial. [25] Itraconazole pulse therapy is currently FDA approved only for fingernail onychomycosis. Binding of itraconazole to mammalian cytochrome P450 3A4 system in the liver is responsible for potential itraconazole toxicity and drug interactions. The common adverse reactions include headache and gastrointestinal upset. Asymptomatic liver function abnormalities occur in less than 3%. Hepatitis tends to occur with continuous therapy usually after 4 weeks. A case of severe hepatic dysfunction requiring liver transplantation has been reported. [26] Monitoring for hepatic functions is recommended in patients with pre-existing derangement, those receiving continuous therapy for > 1 month, and with concomitant use of hepatotoxic drugs. It is contraindicated in patients with congestive cardiac failure due to increased risk of negative inotropic effects and therefore carries a black box warning regarding heart failure. [27] Due to its ability to prolong the QT interval and increase the risk of arrhythmia, co-administration of cisapride, pimozide, and quinidine are contraindicated.
Terbinafine , an allylamine, inhibits fungal squalene epoxidase, leading to accumulation of squalene, responsible for its fungicidal effect. In vitro terbinafine is fungicidal against dermatophytes, NDM (Apergillus fumigatus and Scopulariopsis brevicaulis) and C. parapsilosis and fungistatic against C. albicans. Terbinafine is well absorbed orally with > 70% bioavailability. It is keratinophilic and detectable in the nail from 7 days of initiating therapy up to 90 days after treatment and is FDA approved for continuous treatment (250 mg daily) for 6 weeks for fingernail and 12 weeks for toenail onychomycosis. The LION study demonstrated superiority of continuous terbinafine in terms of long-term mycological and clinical cure and lower risk of recurrence over intermittent itraconazole. [28] In a cumulative meta-analysis of randomized controlled trials, mycological cure rates of 76 ± 3%, 63 ± 7%, and 59 ± 5% were reported with terbinafine, itraconazole pulse and itraconazole continuous regimes, respectively. The corresponding values for clinical response were as follows: terbinafine 66 ± 5%, pulse intraconazole 70 ± 11%, and continuous itraconazole 70 ± 5%. [29] In terms of long-term efficacy, terbinafine has been found to be superior to itraconazole, fluconazole, and ketoconazole. [30],[31] Multiple intermittent regimes of terbinafine have been evaluated. Gupta et al., [32] employed two courses of terbinafine (250 mg daily for 4 weeks) alternating with 4 weeks interval without terbinafine and found it to be as effective as continuous terbinafine and more efficacious than pulse itraconazole for treatment of toe nail onychomycosis. [32] A regimen of three weekly pulses of terbinafine (250 mg twice daily for 1 week every month) alone or in combination with topical terbinafine has also been found to be efficacious for dermatophyte onychomycosis. [33],[34] Sikder et al., found 4 weekly pulses of terbinafine to be more effective than intermittent itraconazole. [35] Common adverse reactions with terbinafine include gastrointestinal symptoms, skin rash, pruritus, urticaria, asymptomatic liver enzyme abnormalities, and taste disturbances. Severe adverse drug reactions are infrequent and include agranulocytosis, hepatitis, acute generalized exanthematous pustulosis, and lupus erythematous. Due to reports of occurrence of systemic lupus erythematosus and other autoimmune disorders in patients receiving terbinafine, it is prudent to exert caution when using in patients with known autoimmunity. [36] Terbinafine is metabolized by cytochrome P 450 enzymes and therefore concentration is decreased by rifampicin and increased by cimetidine. It decreases cyclosporin levels and inhibits the cytochrome P450 enzyme CYP2D6 responsible for metabolism of tricyclic antidepressants, beta blockers, selective serotonin reuptake inhibitors, and monoamine oxidase inhibitors type B.
Newer therapies
A ciclopirox hydrolacquer based on water soluble biopolymer technology was shown to be more effective than conventional lacquer in a recent study. [37] Baran et al., reported efficacy of 1% fluconazole and 20% urea in a mixture of ethanol and water, used daily in the treatment of onychomycosis affecting distal nail. [38] Recently, terbinafine nail solution was shown to be more effective than ciclopirox in a guinea pig model. [39] Terbinafine nail solution was also shown to be safe and efficacious when delivered through iontophoresis. [40] AN2690 is a novel oxaborole broad spectrum antifungal designed with properties required to allow for easier penetration through the nail plate, has been shown to have superior in vitro penetration compared to ciclopiroxolamine. [41] Newer strategies to enhance nail penetration of topical drugs include enhancing penetration by iontophoresis, physical modalities such as manual and electrical nail abrasion, acid etching, microporation, application of low-frequency ultrasound, laser nail ablation, and use of chemicals that have ungual enhancer activity. [42] Latest addition in the armamentarium for onychomycosis is laser therapy. Landsman et al., [43] reported the efficacy of Noveon dual-wavelength (using 870-nm, 930-nm light) near-infrared diode laser in the treatment of moderate to severe onychomycosis. [43] A novel 0.65 millisecond pulsed Nd:YAG 1064-nm laser and femtosecond infrared titanium sapphire lasers have also shown promising results. [44],[45] Photodynamic therapy has also been used with variable success. [46],[47] Dai et al., [48] demonstrated the efficacy of topical germicidal UVC radiation in the treatment of onychomycosis. [48]
Amongst the systemic therapies, voriconazole, a novel azole antifungal was found to have low MIC against dermatophytes, Candida and NDM in a recent study. However, current use is limited to invasive disease in immunocompromised patients and is not recommended as first-line therapy in onychomycosis. [49] Efficacy and safety of ravuconazole 200 mg/day in the treatment of onychomycosis reported in one study needs further confirmation. [50]
Combination therapy
Despite proven efficacy of oral antifungals, clinical outcome is often far from satisfactory. Invariably, mycological cure rates are about 30% better than clinical cure rates in most studies and treatment failure rate even in the best clinical trials is at least 25%. [17] In an attempt to improve the cure rate and reduce relapse, use of combination therapy has become necessary. Drug penetration may be suboptimal in the lateral borders of nail with oral therapy, whereas topical therapies may not penetrate deeper layers of nail. Oral drugs rapidly accumulate in the nail bed, whereas topical therapies penetrate the nail plate including the lateral margins. [17] Significant levels of oral drugs take some time to develop while amorolfine reaches the nail within few hours of treatment. Besides, oral drugs bind to the matrix tissue and are retained even after treatment cessation. The combination of oral and topical drugs may allow reduction in oral dosing resulting in increased patient tolerance and compliance while improving efficacy and reducing relapse. In an open randomized trial, mycological cure rates of 83% was achieved in patients of toenail onychomycosis receiving itraconazole and amorolfine lacquer as compared to 41% in patients receiving itraconazole alone for 12 weeks. [51] In another similar trial, combination of oral terbinafine and amorolfine lacquer achieved a mycological cure rate of 27% in 12 weeks as compared to 17% in patients receiving terbinafine alone. [52] Likewise, combination with surgical therapies like physical debridement can reduce the fungal load and aid drug penetration. [16] The combination regimes can be administered parallel (both oral and topical drugs given simultaneously) for patients likely to fail therapy or sequentially (administration of oral drug alone followed by topical). [53]
Supplementary therapy
Supplementary therapy involves microscopic examination and culture at 24 weeks or 6 months following initiation of therapy and extended administration of oral antifungal (4 weeks of daily terbinafine or another pulse of itraconazole) in patients who are found positive. This is based on the belief that there is a window of opportunity for booster therapy until 6-9 months from start of therapy during which residual drug concentration can still be detected within the nail and a short burst of extra therapy during this time may be just sufficient to produce cure especially in patients who are likely to fail therapy. [2]
Sequential therapy
Sequential therapy combines use of two oral antifungals acting on two different pathways in ergosterol metabolism. As a result, the duration of treatment and cumulative drug exposure to each antifungal is reduced. Patients are given 2 pulses of itraconazole followed by one or two pulses of terbinafine. The results were compared with patients receiving 3-4 pulses of only terbinafine. Complete cure was seen in 52 vs. 32% patients, respectively. Itraconazole was administered before terbinafine because the former is barely detectable in plasma 10-14 days after completing a pulse. [54]
Boosted oral antifungal treatment and boosted antifungal topical treatment
The boosted oral antifungal treatment (BOAT) is designed to target dormant chlamydospores and arthroconidia within the nail plate in order to produce sensitive hyphae which are less refractory to antifungal treatment. [2],[16] This is performed by securing a piece of Saboraud′s dextrose agar on to the affected nail plate for 48 hours following weekly pulse of itraconazole. A pilot study suggested that this protocol improves the mycological cure rate compared to conventional treatments (> 90%). [55] A similar approach is boosted antifungal topical treatment (BATT), designed to improve the therapeutic efficacy of amorolfine nail lacquer. [56] These therapies however carry the risk of over stimulation and systemic spread of fungi that are not susceptible to the antifungal agent and therefore not yet widely accepted.
Surgical intervention
Surgical methods can be used to remove part (debridement) or whole (avulsion) of the nail plate. Partial removal is an effective option in patients with lateral nail plate involvement or with onycholytic pockets on the undersurface of nail filled with a longitudinal spike/ dermatophytoma. Such methods can also be combined with oral and/or topical treatments. Nails can be removed using a carbon dioxide laser. Surgical distal removal is a painful procedure and carries the risk of infection and abnormal nail regrowth (distal nail embedding). Malay et al., [57] found combination of debridement and nail lacquer application (76.7% mycological cure rate) to be more effective than debridement alone. [57] However, Grover et al., [58] did not find encouraging results when surgical nail avulsion for single nail onychomycosis was combined with topical antifungal creams. [58]
Chemical nail avulsion involves application of keratolytic agents such as 40% urea to the affected nail which can be trimmed subsequently. Chemical avulsion reduces the fungal load to a lesser extent than surgical avulsion. It should be reserved for patients with very thick nails and for patients unsuitable for mechanical removal. Nail avulsion is generally not indicated in the elderly and in patients with multiple infected toenails. Apart from avulsion, mechanical nail abrasion using sandpaper fraises or a high-speed hand piece at the beginning of treatment with antifungal nail lacquer decreases the critical fungal mass and aids the penetration of the topical agent into the deepest nail layers. [2]
Nondermatophytic onychomycosis
NDM are often difficult to eradicate and usually require a combination of approaches to achieve success. Although new antifungals especially itraconazole have a broad spectrum of activity, there is paucity of data from larger clinical trials regarding its efficacy in NDM onychomycosis and treatment regimes are not well standardized. Tosti et al., [5] in their study of 59 cases of NDM, reported better cure rates with a combination of topical treatment and surgical avulsion a (~60%) compared to monotherapy with terbinafine or itraconazole alone (20% Acremonium species, 29% Fusarium, and 42% Scopulariopsis brevicaulis). [5] Aspergillus is the only exception that responds well to systemic therapy with either terbinafine or itraconazole. [59],[60] Terbinafine is believed to have good in vitro antifungal activity against Scopulariopsis species [61] In terms of clinical presentation, SWO can be treated with abrasion of nail surface followed by topical therapy with nail lacquers. Systemic therapy should be added if SWO is originating from proximal nail fold. DLSO can be treated with itraconazole or terbinafine therapy. However, duration of therapy may be prolonged as compared to dermatophytes. Treatment of other molds is often challenging and may require combination of oral, topical and surgical methods. [60]
Candida onychomycosis
CO is responsive to both systemic and topical treatment and both itraconazole and fluconazole are equally efficacious. Itraconazole can be used as continuous or pulse regime. Fluconazole is given as 50 mg/day or 300 mg/week to be continued for minimum 4 weeks for fingernail and 12 weeks for toenail onychomycosis. [60] Rigopoulos et al., [62] found combination of amorolfine nail lacquer and 2 pulses of itraconazole to be as safe and effective and less expensive than monotherapy with 3 pulses of itraconazole in moderate to severe cases of CO. [62]
Relapse
Onychomycosis relapse is defined as the return of infection, whatever time has elapsed. It can be due to either reinfection or recurrence. Recurrence is defined as the return of disease within a year of therapy completion. Reinfection implies contracting the infection after having achieved complete cure, usually after a period of one year. [63] Reinfection usually indicates the predisposition of an individual towards acquiring an infection, which can due to factors such as age, genetic factors, occupation, climate, nature and extent of initial infection or presence of tinea pedis, and comorbid conditions such as diabetes and immunosuppression.
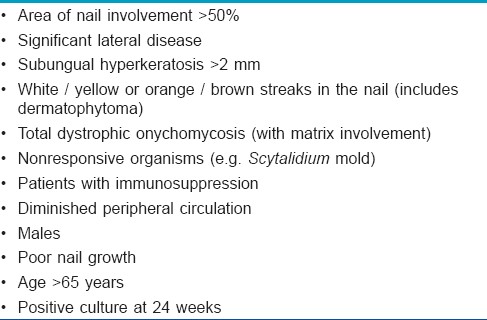
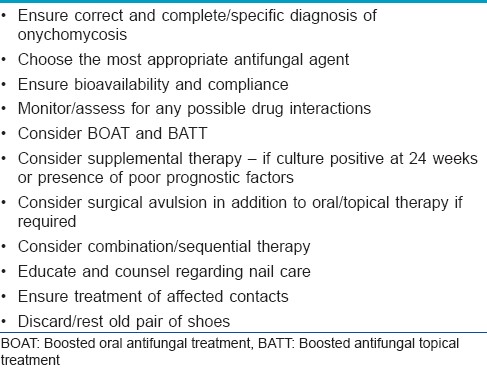
Therapeutic failure may occur due to various causes which include lack of diagnostic accuracy, inappropriate choice of antifungal or mode of delivery, presence of dormant conidia, sequestrated mycelial pockets or resistant fungal species, or lack of consistent penetration. [4] Certain prognostic factors can help determine the choice of therapeutic agent, length of treatment, and duration of follow-up and may help in identifying cases requiring extended treatment thereby reducing the chances of failure/relapse [Table - 2] and [Table - 3]. Spikes refer to the yellowish, hyperkeratotic band of nail that progresses proximally towards the matrix, while dermatophytoma is the thick mass of fungal hyphae and necrotic keratin between the nail plate and nail bed. [63] Ratajczak-Stefańska et al., [64] reported repeated monotherapy with terbinafine or itraconazole to be the least efficient regimen for recurrent onychomycosis. Combination of itraconazole and pentoxifylline or itraconazole and topical amorolfine were found to be more useful. [64]
Special Populations
Children
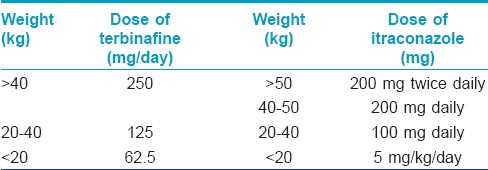
Children have a 30 fold decrease in the prevalence of onychomycosis as compared to adults possibly due to smaller contact surface, reduced environmental exposure and trauma, faster nail growth, and lower prevalence of tinea pedis. [1] Children with onychomycosis should be carefully screened for any cutaneous mycoses in them and close family contacts. Griseofulvin is the only licensed antifungal for use in children in a dosage of 10 mg/kg daily. Laboratory testing including hemogram and liver function tests should be carried out at baseline and periodically. Though newer antifungals including terbinafine and itraconazole are not approved for the use in children, they have been used safely with favorable outcome. Moreover, terbinafine is approved for the treatment of tinea capitis in children above 4 years of age. Ginter-Haanselmeyer et al., [68] have used terbinafine and itraconazole in their series of 36 patients aged 4-17 years and reported no significant side effects specific to children [Table - 4]. [68] Both daily and pulsed regimen of fluconazole (3-6 mg/kg) have also been considered safe. [69]
Elderly
Increased incidence of onychomycosis and poor treatment response with age are attributable to risk factors such as poor peripheral circulation, repeated trauma, suboptimal immune function, and inability to maintain good foot care. [1] Management of onychomycosis may include no therapy, palliative treatment with mechanical or chemical debridement, topical antifungal therapy, oral antifungal agents, or combination of these modalities. Gupta et al., [70] have reported both continuous and pulsed terbinafine and itraconazole to be safe in elderly. [70] Terbinafine is considered the drug of choice for dermatophyte onychomycosis with greater mycological cure, lesser side effects, fewer drug interactions, and lower cost than continuous itraconazole therapy. In general, topical therapy is not practical in elderly because of the recommended frequency of application, periodic debridement of affected nails, and longer treatment except in patients with SWO and in those receiving multiple medications due to the risk of possible drug interactions.
Diabetics
Diabetics, particularly men, are 2.5-2.8 times more likely to have onychomycosis than the control population. [71] The combination of ischemia, sensory neuropathy, poor glycemic control, and impaired host defence render these patients vulnerable. [27] Dogra et al., [71] reported yeast to be the most common causative agent in this group followed by dermatophytes and NDM. [71] Topical preparations are preferable but carry the drawback of prolonged treatment and cumbersome application due to comorbid obesity and advanced age. Foot care interventions including nail drilling in combination with topical therapies have been shown to be effective. [72] Drug interactions resulting in hypoglycemia are usually not significant with itraconazole and terbinafine therapy in patients on concomitant hypoglycemic medications. [73] Terbinafine is the first-line treatment due to low risk of drug interactions and proven efficacy. [61] Though itraconazole is considered safe and effective, it is not the first-line drug due to black box cardiac warning and drug interactions. [27]
Pregnancy and lactation
Terbinafine is category B drug while itraconazole and fluconazole are in pregnancy category C. Use of all these drugs should be avoided in pregnancy. All oral antifungals are excreted in breast milk and therefore contraindicated in lactating mothers. [2]
| 1. |
Kaur R, Kashyap B, Bhalla P. Onychomycosis-epidemiology, diagnosis and management. Indian J Med Microbiol 2008;26:108-16.
[Google Scholar]
|
| 2. |
Baran R, Hay R, Haneke E, Tosti A, editors. Onychomycosis: The current approach to diagnosis and therapy. London: Informa Healthcare; 2006.
[Google Scholar]
|
| 3. |
Sehgal VN, Srivastava G, Dogra S, Chaudhary A, Adhikari T. Onychomycosis: An Asian perspective. Skinmed 2010;8:37-45.
[Google Scholar]
|
| 4. |
Arrese JE, Piérard GE. Treatment failures and relapses in onychomycosis: A stubborn clinical problem. Dermatology 2003;207:255-60.
[Google Scholar]
|
| 5. |
Tosti A, Piraccini BM, Lorenzi S. Onychomycosis caused by nondermatophytic molds: Clinical features and response to treatment of 59 cases. J Am Acad Dermatol 2000;42:217-24.
[Google Scholar]
|
| 6. |
Jayayatilake JA, Tilakaratne WM, Panagoda GJ. Candida onychomycosis: A mini-review. Mycopathologia 2009;168:165-73.
[Google Scholar]
|
| 7. |
Baran R, Hay R, Perrin C. Superficial white onychomycosis revisited. J Eur Acad Dermatol Venereol 2004;18:569-71.
[Google Scholar]
|
| 8. |
Haldane DJ, Robart E. A comparison of calcofluor white, potassium hydroxide, and culture for the laboratory diagnosis of superficial fungal infection. Diagn Microbiol Infect Dis 1990;13:337-9.
[Google Scholar]
|
| 9. |
Weinberg JM, Koestenblatt EK, Tutrone WD, Tishler HR, Najarian L. Comparision of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol 2003;49:193-7.
[Google Scholar]
|
| 10. |
Shemer A, Trau H, Davidovici B, Grunwald MH, Amichai B. Collection of fungi samples from nails: Comparative study of curettage and drilling techniques. J Eur Acad Dermatol Venereol 2008;22:182-5.
[Google Scholar]
|
| 11. |
Gianni C, Morelli V, Cerri A, Greco C, Rossini P, Guiducci A, et al. Usefulness of histological examination for the diagnosis of onychomycosis. Dermatology 2001;202:283-8.
[Google Scholar]
|
| 12. |
Bontems O, Hauser PM, Monod M. Evaluation of a polymerase chain reaction-restriction fragment length polymorphism assay for dermatophyte and nondermatophyte identification in onychomycosis. Br J Dermatol 2009;161:791-6.
[Google Scholar]
|
| 13. |
Gupta AK, Zaman M, Singh J. Diagnosis of Trichophyton rubrum from onychomycotic nail samples using polymerase chain reaction and calcofluor white microscopy. J Am Podiatr Med Assoc 2008;98:224-8.
[Google Scholar]
|
| 14. |
Scherer WP, Scherer MD. Scanning electron microscope imaging of onychomycosis. J Am Podiatr Med Assoc 2004;94:356-62.
[Google Scholar]
|
| 15. |
Roberts DT, Taylor WD, Boyle J. British Association of Dermatologists. Guidelines for treatment of onychomycosis. Br J Dermatol 2003;148:402-10.
[Google Scholar]
|
| 16. |
Lecha M, Effendy I, Feuilhade de Chauvin M, Di Chiacchio N, Baran R; Taskforce on Onychomycosis Education. Treatment options-development of consensus guidelines. J Eur Acad Dermatol Venereol 2005;19 Suppl 1:25-33.
[Google Scholar]
|
| 17. |
Hay RJ. The future of onychomycosis therapy may involve a combination of approaches. Br J Dermatol 2001;145 Suppl 60:3-8.
[Google Scholar]
|
| 18. |
Sidou F, Soto P. A randomized comparison of nail surface remanence of three nail lacquers, containing amorolfine 5%, ciclopirox 8% or tioconazole 28%, in healthy volunteers. Int J Tissue React 2004;26:17-24.
[Google Scholar]
|
| 19. |
Gupta AK, Schouten JR, Lynch LE. Ciclopirox nail lacquer 8% for the treatment of onychomycosis: A Canadian perspective. Skin Therapy Lett 2005;10:1-3.
[Google Scholar]
|
| 20. |
Rigopoulos D, Katsambas A, Antoniou C, Christofidou E, Balaskas E, Stratigos J. Discoloration of the nail plate due to the misuse of amorolfine 5 % nail lacquer. Acta Derm Venereol 1996;76:83-4.
[Google Scholar]
|
| 21. |
Gupta AK, Ryder JE. The use of oral antifungal agents to treat onychomycosis. Dermatol Clin 2003;21:469-79.
[Google Scholar]
|
| 22. |
Brown SJ. Efficacy of fluconazole for the treatment of onychomycosis. Ann Pharmacother 2009;43:1684-91.
[Google Scholar]
|
| 23. |
Zisova LG. Fluconazole (Fungolon) in the treatment of onychomycosis. Folia Med (Plovdiv) 2004;46:47-50.
[Google Scholar]
|
| 24. |
Scher RK, Breneman D, Rich P, Savin RC, Feingold DS, Konnikov N, et al. Once-weekly fluconazole (150, 300, or 450 mg) in the treatment of distal subungual onychomycosis of the toenail. J Am Acad Dermatol 1998;38:S77-86.
[Google Scholar]
|
| 25. |
Havu V, Brandt H, Heikkilä H, Hollmen A, Oksman R, Rantanen T, et al. A double-blind, randomized study comparing itraconazole pulse therapy with continuous dosing for the treatment of toe-nail onychomycosis. Br J Dermatol 1997;136:230-4.
[Google Scholar]
|
| 26. |
Srebrnik A, Levtov S, Ben-Ami R, Brenner S. Liver failure and transplantation after itraconazole treatment for toenail onychomycosis. J Eur Acad Dermatol Venereol 2005;19:205-7.
[Google Scholar]
|
| 27. |
Cathcart S, Cantrell W, Elewski B. Onychomycosis and diabetes. J Eur Acad Dermatol Venereol 2009;23:1119-22.
[Google Scholar]
|
| 28. |
Sigurgeirsson B, Billstein S, Rantanen T, Ruzicka T, di Fonzo E, Vermeer BJ, et al. L.I.ON. Study: Efficacy and tolerability of continuous terbinafine (Lamisil) compared to intermittent itraconazole in the treatment of toenail onychomycosis. Lamisil vs. Itraconazole in Onychomycosis. Br J Dermatol 1999;141 Suppl 56:5-14.
[Google Scholar]
|
| 29. |
Gupta AK, Ryder JE, Johnson AM. Cumulative meta-analysis of systemic antifungal agents for the treatment of onychomycosis. Br J Dermatol 2004;150:537-44.
[Google Scholar]
|
| 30. |
Piraccini BM, Sisti A, Tosti A. Long-term follow-up of toenail onychomycosis caused by dermatophytes after successful treatment with systemic antifungal agents. J Am Acad Dermatol 2010;62:411-4.
[Google Scholar]
|
| 31. |
Cribier BJ, Paul C. Long-term efficacy of antifungals in toenail onychomycosis: A critical review. Br J Dermatol 2001;145:446-52.
[Google Scholar]
|
| 32. |
Gupta AK, Lynch LE, Kogan N, Cooper EA. The use of an intermittent terbinafine regimen for the treatment of dermatophyte toenail onychomycosis. J Eur Acad Dermatol Venereol 2009;23:256-62.
[Google Scholar]
|
| 33. |
Takahata Y, Hiruma M, Shiraki Y, Tokuhisa Y, Sugita T, Muto M. Treatment of dermatophyte onychomycosis with three pulses of terbinafine (500 mg day for a week). Mycoses 2009;52:72-6.
[Google Scholar]
|
| 34. |
Nakano N, Hiruma M, Shiraki Y, Chen X, Porgpermdee S, Ikeda S. Combination of pulse therapy with terbinafine tablets and topical terbinafine cream for the treatment of dermatophyte onychomycosis: A pilot study. J Dermatol 2006;33:753-8.
[Google Scholar]
|
| 35. |
Sikder AU, Mamun SA, Chowdhury AH, Khan RM, Hoque MM. Study of oral itraconazole and terbinafine pulse therapy in onychomycosis. Mymensingh Med J 2006;15:71-80.
[Google Scholar]
|
| 36. |
Bonsmann G, Schiller M, Luger TA, Ständer S. Terbinafine-induced subacute cutaneous lupus erythematosus. J Am Acad Dermatol 2001;44:925-31.
[Google Scholar]
|
| 37. |
Baran R, Tosti A, Hartmane I, Altmeyer P, Hercogova J, Koudelkova V, et al. An innovative water-soluble biopolymer improves efficacy of ciclopirox nail lacquer in the management of onychomycosis. J Eur Acad Dermatol Venereol 2009;23:773-81.
[Google Scholar]
|
| 38. |
Baran R, Coquard F. Combination of fluconazole and urea in a nail lacquer for treating onychomycosis. J Dermatolog Treat 2005;16:52-5.
[Google Scholar]
|
| 39. |
Ghannoum MA, Long L, Pfister WR. Determination of the efficacy of terbinafine hydrochloride nail solution in the topical treatment of dermatophytosis in a guinea pig model. Mycoses 2009;52:35-43.
[Google Scholar]
|
| 40. |
Amichai B, Nitzan B, Mosckovitz R, Shemer A. Iontophoretic delivery of terbinafine in onychomycosis: A preliminary study. Br J Dermatol 2010;162:46-50.
[Google Scholar]
|
| 41. |
Hui X, Baker SJ, Wester RC, Barbadillo S, Cashmore AK, Sanders V, et al. In vitro penetration of a novel oxaborole antifungal (AN2690) into the human nail plate. J Pharm Sci 2007;96:2622-31.
[Google Scholar]
|
| 42. |
Murdan S. Enhancing the nail permeability of topically applied drugs. Expert Opin Drug Deliv 2008;5:1267-82.
[Google Scholar]
|
| 43. |
Landsman AS, Robbins AH, Angelini PF, Wu CC, Cook J, Oster M, et al. Treatment of mild, moderate, and severe onychomycosis using 870- and 930-nm light exposure. J Am Podiatr Med Assoc 2010;100:166-77.
[Google Scholar]
|
| 44. |
Hochman LG. Laser treatment of onychomycosis using a novel 0.65-millisecond pulsed Nd:YAG 1064-nm laser. J Cosmet Laser Ther 2011;13:2-5.
[Google Scholar]
|
| 45. |
Manevitch Z, Lev D, Hochberg M, Palhan M, Lewis A, Enk CD. Direct antifungal effect of femtosecond laser on Trichophyton rubrum onychomycosis. Photochem Photobiol 2010;86:476-9.
[Google Scholar]
|
| 46. |
Watanabe D, Kawamura C, Masuda Y, Akita Y, Tamada Y, Matsumoto Y. Successful treatment of toenail onychomycosis with photodynamic therapy. Arch Dermatol 2008;144:19-21.
[Google Scholar]
|
| 47. |
Sotiriou E, Koussidou-Eremonti T, Chaidemenos G, Apalla Z, Ioannides D. Photodynamic therapy for distal and lateral subungual toenail onychomycosis caused by Trichophyton rubrum: Preliminary results of a single-centre open trial. Acta Derm Venereol 2010;90:216-7.
[Google Scholar]
|
| 48. |
Dai T, Tegos GP, Rolz-Cruz G, Cumbie WE, Hamblin MR. Ultraviolet C inactivation of dermatophytes: Implications for treatment of onychomycosis. Br J Dermatol 2008;158:1239-46.
[Google Scholar]
|
| 49. |
Bueno JG, Martinez C, Zapata B, Sanclemente G, Gallego M, Mesa AC. In vitro activity of fluconazole, itraconazole, voriconazole and terbinafine against fungi causing onychomycosis. Clin Exp Dermatol 2010;35:658-63.
[Google Scholar]
|
| 50. |
Gupta AK, Leonardi C, Stoltz RR, Pierce PF, Conetta B; Ravuconazole onychomycosis group. A phase I/II randomized, double-blind, placebo-controlled, dose-ranging study evaluating the efficacy, safety and pharmacokinetics of ravuconazole in the treatment of onychomycosis. J Eur Acad Dermatol Venereol 2005;19:437-43.
[Google Scholar]
|
| 51. |
Lecha M. Amorolfine and itraconazole combination for severe toenail onychomycosis: Results of an open randomized trial in Spain. Br J Dermatol 2001;145 Suppl 60:21-6.
[Google Scholar]
|
| 52. |
Baran R, Feuilhade M, Combernale P, Datry A, Goettmann S, Pietrini P, et al. A randomised trial of amorolfine 5% solution nail lacquer combined with oral terbinafine compared with terbinafine alone in the treatment of dermatophytic toenail onychomycoses affecting the matrix region. Br J Dermatol 2000;142:1177-83.
[Google Scholar]
|
| 53. |
Olafsson JH, Sigurgeirsson B, Baran R. Combination therapy for onychomycosis. Br J Dermatol 2003;149 Suppl 65:15-8.
[Google Scholar]
|
| 54. |
Gupta AK, Lynde CW, Konnikov N. Single-blind, randomized, prospective study of sequential itraconazole and terbinafine pulse compared with terbinafine pulse for the treatment of toenail onychomycosis. J Am Acad Dermatol 2001;44:485-91.
[Google Scholar]
|
| 55. |
Piérard GE, Piérard-Franchimont C, Arrese JE. The boosted oral antifungal treatment for onychomycosis beyond the regular itraconazole pulse dosing regimen. Dermatology 2000;200:185-7.
[Google Scholar]
|
| 56. |
Pierard GE, Pierard-Franchimont C, Arrese JE. The boosted antifungal topical treatment (BATT) for onychomycosis. Med Mycol 2000;38:391-2.
[Google Scholar]
|
| 57. |
Malay DS, Yi S, Borowsky P, Downey MS, Mlodzienski AJ. Efficacy of debridement alone versus debridement combined with topical antifungal nail lacquer for the treatment of pedal onychomycosis: A randomized, controlled trial. J Foot Ankle Surg 2009;48:294-308.
[Google Scholar]
|
| 58. |
Grover C, Bansal S, Nanda S, Reddy BS, Kumar V. Combination of surgical avulsion and topical therapy for single nail onychomycosis: A randomized controlled trial. Br J Dermatol 2007;157:364-8.
[Google Scholar]
|
| 59. |
Gianni C, Romano C. Clinical and histological aspects of toenail onychomycosis caused by Aspergillus spp.: 34 cases treated with weekly intermittent terbinafine. Dermatology 2004;209:104-10.
[Google Scholar]
|
| 60. |
Tosti A, Piraccini BM, Lorenzi S, Iorizzo M. Treatment of nondermatophyte mold and Candida onychomycosis. Dermatol Clin 2003;21:491-7.
[Google Scholar]
|
| 61. |
Cribier BJ, Bakshi R. Terbinafine in the treatment of onychomycosis: A review of its efficacy in high-risk populations and in patients with nondermatophyte infections. Br J Dermatol 2004;150:414-20.
[Google Scholar]
|
| 62. |
Rigopoulos D, Katoulis AC, Ioannides D, Georgala S, Kalogeromitros D, Bolbasis I, et al. A randomised trial of amorolfine 5 % nail solution nail lacquer in association with itraconazole pulse therapy compared with itraconazole alone in the treatment of Candida fingernail onychomycosis. Br J Dermatol 2003;149:151-6.
[Google Scholar]
|
| 63. |
Scher RK, Baran R. Onychomycosis in clinical practice: Factors contributing to recurrence. Br J Dermatol 2003;149 Suppl 65:5-9.
[Google Scholar]
|
| 64. |
Ratajczak-Stefañska V. Assessment of mycological and clinical factors on the course and results of treatment of mycotic infections in patients with recurrent onychomycosis. Ann Acad Med Stetin 2003;49:161-71.
[Google Scholar]
|
| 65. |
Sigurgeirsson B. Prognostic factors for cure following treatment of onychomycosis. J Eur Acad Dermatol Venereol 2010;24:679-84.
[Google Scholar]
|
| 66. |
Gupta AK, Ryder JE. How to improve cure rates for the management of onychomycosis. Dermatol Clin 2003;21:499-505.
[Google Scholar]
|
| 67. |
Thappa DM. Current treatment of onychomycosis. Indian J Dermatol Venereol Leprol 2007;73:373-6.
[Google Scholar]
|
| 68. |
Ginter-Hanselmayer G, Weger W, Smolle J. Onychomycosis: A new emerging infectious disease in childhood population and adolescents. Report on treatment experience with terbinafine and itraconazole in 36 patients. J Eur Acad Dermatol Venereol 2008;22:470-5.
[Google Scholar]
|
| 69. |
Gupta AK, Chang P, Del Rosso JQ, Adam P, Hofstader SL. Onychomycosis in children: Prevalence and management. Pediatr Dermatol 1998;15:464-71.
[Google Scholar]
|
| 70. |
Gupta AK, Konnikov N, Lynde CW. Single-blind, randomized, prospective study on terbinafine and itraconazole for treatment of dermatophyte toenail onychomycosis in the elderly. J Am Acad Dermatol 2001;44:479-84.
[Google Scholar]
|
| 71. |
Dogra S, Kumar B, Bhansali A, Chakrabarty A. Epidemiology of onychomycosis in patients with diabetes mellitus in India. Int J Dermatol 2002;41:647-51.
[Google Scholar]
|
| 72. |
Sumikawa M, Egawa T, Honda I, Yamamoto Y, Sumikawa Y, Kubota M. Effects of foot care intervention including nail drilling combined with topical antifungal application in diabetic patients with onychomycosis. J Dermatol 2007;34:456-64.
[Google Scholar]
|
| 73. |
Mayser P, Freund V, Budihardja D. Toenail onychomycosis in diabetic patients: Issues and management. Am J Clin Dermatol 2009;10:211-20.
[Google Scholar]
|
Fulltext Views
28,456
PDF downloads
6,646





