Translate this page into:
Palmar creases as diagnostic clues to the dermatological disorders
Corresponding author: Dr. Ramamoorthy Logamoorthy, Department of Dermatology Venereology and Leprosy, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, India. logamoorthy.r@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Radhakrishnan S, Logamoorthy R, Karthikeyan K. Palmar creases as diagnostic clues to the dermatological disorders. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1865_2024
Introduction
Palmar creases, the lines on the palms, provide valuable diagnostic clues for dermatological, genetic and systemic conditions, aiding in the recognition of both congenital and acquired disorders. This review examines their anatomical basis, variations, and disease associations, emphasising their importance in diagnosis and management while excluding the broader field of dermatoglyphics.
Types of palmar creases
Palmar creases are the epidermal flexure lines on the hand’s palmar surface, with three primary types: radial longitudinal crease (RLC), proximal transverse crease (PTC), and distal transverse crease (DTC) [Figure 1]. The radial longitudinal crease begins near or below the proximal transverse crease at the palm’s radial border, curves laterally, and extends toward the wrist. The proximal transverse crease starts at the radial side, runs medially with a slight curve, and ends at the hypothenar eminence. The distal transverse crease originates proximal to the index-middle finger interdigital space and extends toward the ulnar side, with a slight distal concavity. The proximal transverse crease and distal transverse crease typically do not traverse the palm’s full width. Palmar creases are classified based on one, two, or three radial origins.1 Variants include branched, forked, broken (detached segments), or cascade (closely running broken segments) patterns. Accessory creases, parallel to the main ones, may exceed half the length of the primary crease, offering significant diversity in palmar crease morphology and clinical relevance.2-4
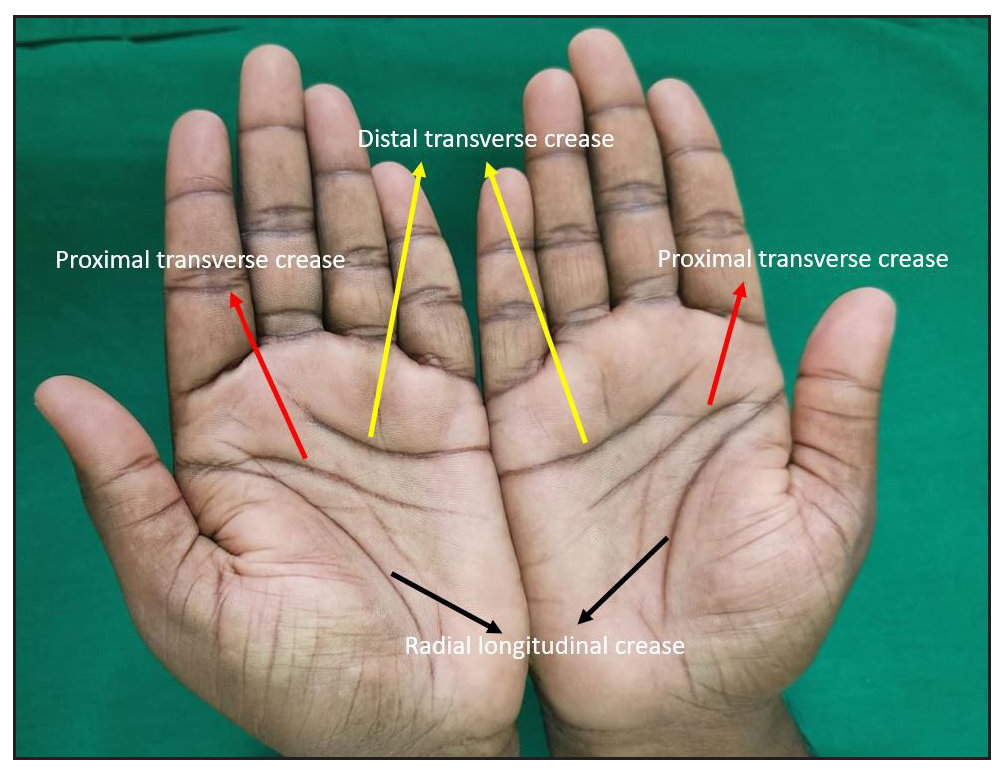
- Normal palms of an individual displaying the three major palmar creases: radial longitudinal crease (black arrows), proximal transverse crease (red arrows), and distal transverse crease (yellow arrows).
Abnormal palmar creases
Palmar creases are classified into Simian, Sydney, and Suwon creases based on the relationship between the proximal transverse crease and distal transverse crease. The Simian crease is a single transverse line seen in Down and Turner syndromes. The Sydney crease is an elongated proximal transverse crease crossing the palm, first described in Sydney. The Suwon crease, found in Suwon, Korea, spans the palm due to proximal transverse crease-distal transverse crease fusion or an extended distal transverse crease with an accessory PTC.5Aberrant palmar creases are observed in healthy individuals across various populations, including Nigerians, Koreans, Central Indians, and Americans. Their presence does not always indicate an underlying medical condition.6
Clinical significance in dermatology
1. Hyperlinearity of palms
Hyperlinear palms (HP) indicate abnormalities in keratinisation and are characterised by the presence of more than five distinct lines, each exceeding 1 cm in length, running across the palm, especially over the thenar eminence.7 The different patterns of palmar hyperlinearity can act as clinical markers for evaluating prognosis and treatment outcomes in atopic eczema. These patterns [Figure 2a-d] correspond to barrier function and disease severity, as summarised in Table 1.8 Notably, the extensive crosshatch pattern is closely linked to higher Eczema Area Severity Index (EASI) scores, Patient-Oriented Eczema Measure (POEM) scores, reduced skin hydration, increased transepidermal water loss and filaggrin (FLG) mutations. Finer patterns indicate milder disease and better barrier function, while crosshatch and diamond patterns signify more severe eczema and impaired barrier function.8

- Palmar hyperlinearity patterns. (a) Pattern 1: Fine perpendicular lines. (b) Pattern 2: Fine crosshatch. (c) Pattern 3: Extensive crosshatch. (d) Pattern 5: Prominent diamond-shaped hyperlinearity.
| Sr.no | Types | Pattern | Description | Significance |
|---|---|---|---|---|
| 1 | Pattern 1 | Fine perpendicular lines | Delicate, straight lines that run perpendicular to the palm’s length. | Lower severity and better barrier function |
| 2 | Pattern 2 | Fine crosshatch | Subtle crosshatched lines that form a grid-like pattern. | Lower severity and better barrier function |
| 3 | Pattern 3 | Extensive crosshatch | Dense crosshatching that covers a significant area of the palm. |
More severe disease and poorer barrier function. |
| 4 | Pattern 4 | Thick perpendicular | Prominent, thicker lines that run vertically across the palm. | Lower severity and better barrier function |
| 5 | Pattern 5 | Prominent diamond | Intersecting lines on the palm form distinct diamond shapes. |
More severe disease and poorer barrier function. |
2. Inverse Gottron sign
The inverse Gottron sign is a rare but specific cutaneous finding in dermatomyositis.9 It is characterised by painful erythematous papules and macules involving the palmar creases of the fingers [Figure 3]. It is a highly specific cutaneous marker of anti-MDA-5 positive dermatomyositis, linked to rapidly progressive interstitial pneumonia.10

- Multiple erythematous, raised, scaly papules localised over the palmar creases of the interphalangeal joints on both hands, characteristic of inverse Gottron papules.
3. Kindler syndrome
Kindler syndrome is an autosomal recessive disorder characterised by acral blistering in infancy, photosensitivity, poikiloderma, cutaneous atrophy, and mucosal involvement. Common associations include periodontitis, gingivitis, palmoplantar keratoderma and diminution of palmar crease.11 In Kindler syndrome, palmar creases are notably diminished due to progressive cutaneous atrophy. This leads to a smooth, almost glossy appearance of the palms, with reduced dermal ridges and a loss of the typical fingerprint pattern.12
4. Keratosis punctata of the palmar crease (KPPC)
KPPC is a benign dermatological condition primarily affecting African Americans (prevalence: 1.9–3.1%). It may be autosomal dominant or sporadic and is associated with Dupuytren contracture, knuckle pads, and striate keratoderma. It is characterised by 1–5 mm hyperkeratotic pits in palmar creases [Figure 4]; KPPC can cause discomfort, affect hand aesthetics, and hinder daily activities.13
- Hyperkeratotic pits over the palmar creases predominantly localised to the distal palmar crease of the left hand in a 15-year-old girl, suggestive of keratosis punctata of the palmar creases.
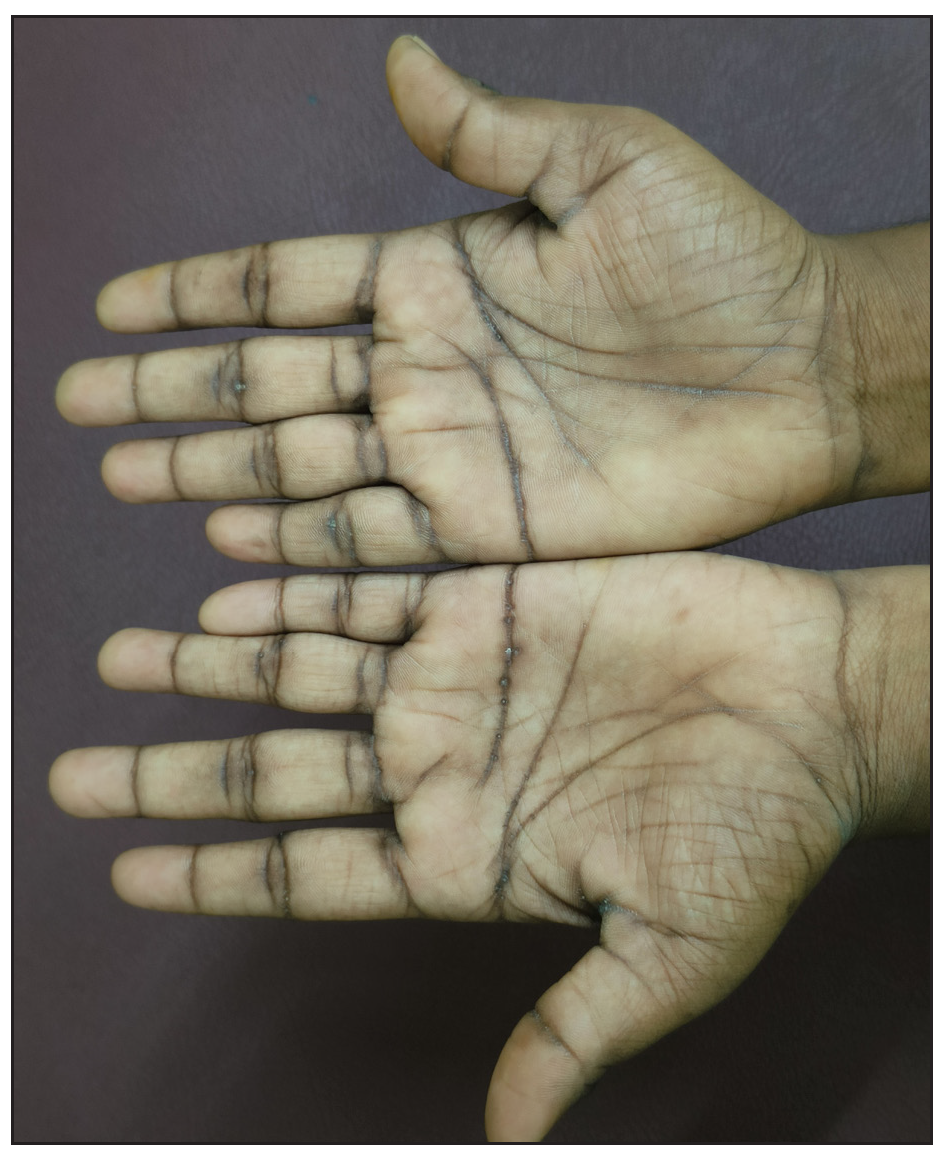
5. Palmar crease hyperpigmentation
Palmar crease pigmentation [Figure 5] refers to darkening or discolouration along the palmar creases due to various physiological, pathological, or external factors. It may manifest in systemic diseases, nutritional deficiencies, or exposure to chemicals. Various causes of palmar crease pigmentation have been listed in Figure 6.14

- Diffuse hyperpigmentation of the palmar creases in a patient with Addison disease, predominantly affecting the creases.
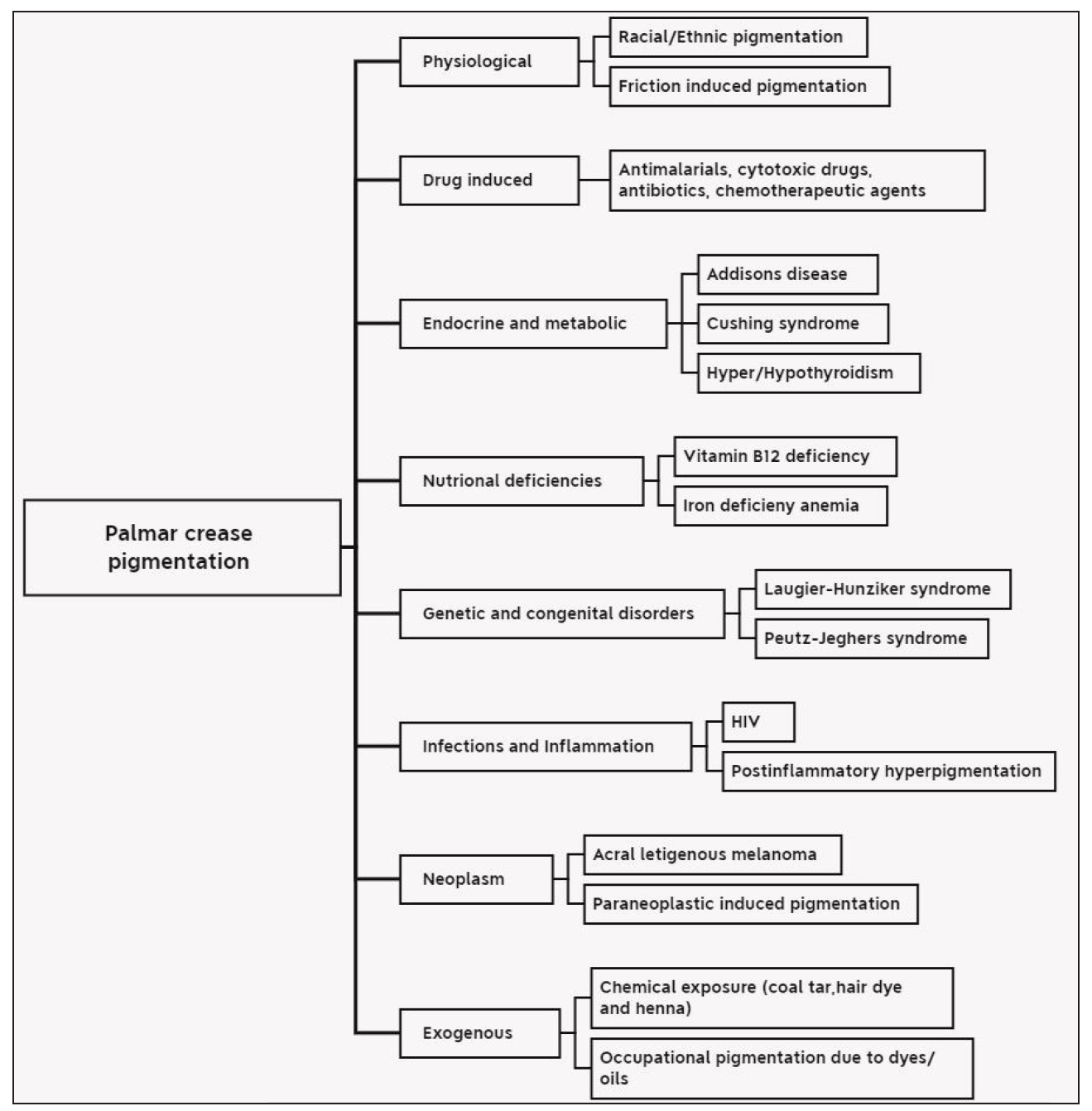
- Various causes of palmar crease pigmentation.
6. Palmar pits
Palmar pits are small, asymmetrical depressions on the palms and soles due to stratum corneum loss. They appear flesh-toned to pink, measuring 2–3 mm in diameter and 1–3 mm in depth.15 Palmar pits are classically associated with disorders such as pitted keratolysis, arsenical keratosis, Darier disease, and acrokeratosis verruciformis of Hopf.16
7. Palmar xanthoma
Palmar xanthomas, or xanthoma striatum palmare, are plane xanthomas affecting the palms and finger creases, presenting as yellow-orange subcutaneous lesions. It is associated with dysbetalipoproteinemia.These lesions arise from microtrauma-induced lipid accumulation, linking localised inflammation to systemic lipid metabolism abnormalities.17
8. Punctate porokeratosis
Punctate porokeratosis (PP) is an uncommon variant of porokeratosis, first identified by Rahbari et al. in 1977. It presents as small, seed-like lesions with raised margins, appearing either in a linear distribution or diffusely across the palms and soles.18
9. Tinea manuum
Tinea manuum is a dermatophyte infection of the palms, often presenting with diffuse scaling and hyperkeratosis [Figure 7]. Dermoscopy aids diagnosis by revealing whitish scales along palm creases, distinguishing it from other dermatoses.19

- Unilateral tinea manuum with scales more pronounced over the palmar creases.
10. Tinea nigra
Tinea nigra is a superficial fungal infection of the stratum corneum caused by the dematiaceous fungus Hortaea werneckii. Tinea nigra presents as dark brown or black patches on palms and soles, with accentuated pigmentation along palmar creases.20
Palmar crease pigmentation scale
The palmar crease pigmentation scale predicts the risk of post-inflammatory hyperpigmentation (PIH), a genetically determined reactive melanosis independent of skin phototype or eye colour. The 4-point visual scale evaluates pigmentation contrast between palmar creases and surrounding skin: score 0 (no difference), Score 1 (low difference), score 2 (moderate difference) and score 3 (high difference). Scores 0 and 1 indicate low PIH risk, while scores 2 and 3 suggest higher risk.21
Conclusion
This review highlights the clinical significance of palmar creases in dermatology, emphasising their potential as diagnostic indicators for various dermatological, genetic and systemic conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Dermatoglyphic assessment in Down and Klinefelter syndromes. Iran J Med Sci. 2007;32:105-9.
- [Google Scholar]
- Improved analysis of palm creases. Anat Cell Biol. 2010;43:169-77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatoglyphics in adults with congenital rubella. Lancet. 1968;2:141-3.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of the different types of palmar creases among medical and dental students in addisababa, Ethiopia. Ethiop J Health Sci. 2019;29:391-400.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hanifin’s and rajka’s minor criteria for atopic dermatitis: Which do 2-year-olds exhibit? J Am Acad Dermatol. 2000;43:785-92.
- [CrossRef] [PubMed] [Google Scholar]
- Deep palmar phenotyping in atopic eczema: Patterns associated with filaggrin variants, disease severity and barrier function in a south asian population. Br J Dermatol. 2023;188:785-92.
- [CrossRef] [PubMed] [Google Scholar]
- Inverse Gottron’s sign in anti-MDA5 antibody-associated dermatomyositis. Rheumatology (Oxford) 2020:keaa108.
- [Google Scholar]
- Inverse Gottron’s sign in anti-MDA5 dermatomyositis. QJM. 2024;117:213.
- [CrossRef] [PubMed] [Google Scholar]
- Kindler syndrome. Indian J Dermatol Venereol Leprol. 2005;71:348-50.
- [CrossRef] [PubMed] [Google Scholar]
- Kindler syndrome: a case series of three Indian children. Indian J Dermatol. 2010;55:393-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case of keratosis punctata of the palmar creases. Ann Dermatol. 2002;14:114.
- [CrossRef] [Google Scholar]
- Addisonian Pigmentation - The Great Mimicker - A Review. Indian J Dermatol. 2024;69(5):422.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Multiple palmar pits and basal cell carcinomas. CMAJ. 2010;182:E533.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Palmar pits and epidermodysplasia verruciformis: A rare association. Indian J Dermatol Venereol Leprol. 2012;78:501-3.
- [CrossRef] [PubMed] [Google Scholar]
- Palmar xanthoma: mirror to pernicious underlying condition. Gulf J Dermatol Venerol. 2017;24:47-50.
- [Google Scholar]
- Punctate porokeratosis. A clinical variant of porokeratosis of Mibelli. J Cutan Pathol. 1977;4(6):338-341.
- [CrossRef] [PubMed] [Google Scholar]
- Tinea nigra: Clinical and diagnostic guidance. Cureus. 2024;16:e66443.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Predicting the risk of postinflammatory hyperpigmentation: The palmar creases pigmentation scale. J Cosmet Dermatol. 2021;20:1263-70.
- [CrossRef] [PubMed] [Google Scholar]





