Translate this page into:
Palmar pits and epidermodysplasia verruciformis: A rare association
2 Department of Dermatology, Medical College and Hospital, Kolkata, India
Correspondence Address:
Piyush Kumar
Department of Dermatology, Katihar Medical College and Hospital, Karim Bagh, Katihar 854105, Bihar
India
| How to cite this article: Kumar P, Lal NR, Gharami RC. Palmar pits and epidermodysplasia verruciformis: A rare association. Indian J Dermatol Venereol Leprol 2012;78:501-503 |
Sir,
Epidermodysplasia verruciformis (EV) is a rare autosomal recessive condition, characterized by genetic susceptibility to persistent, refractory cutaneous infections by specific human papilloma virus strains- called EV types. The clinical picture is quite polymorphic and is characterized by a variety of cutaneous lesions. [1] Palmar pitting is a unique dermatological finding; though it has been reported in healthy individuals too, it is often associated with few malignant and non-malignant conditions. [2] Our case of EV was unique in having bilateral palmar pitting. Till date, only one case of EV with palmar pitting has been documented in English literature. [3]
A 16-year-old boy, born of non-consanguineous marriage, presented with numerous asymptomatic hypopigmented macules, patches and plaques all over body for 10 - 12 years [Figure - 1]. Lately, he started developing hyperpigmented papules and plaques for last 2 - 3 years and presented to us. He was not having any systemic symptoms, and no other family member was affected with similar condition. On examination, multiple hypopigmented macules, patches and thin plaques were noted all over the body, relatively sparing lower limbs. Few hyperpigmented thin plaques, verrucous papules and plaques too were noted [Figure - 2]. Palm was notable for multiple linear pits, distributed in a random fashion over both pressure bearing and non-pressure bearing areas [Figure - 3]. Mucosa including genitalia was spared. The clinical picture was consistent with the diagnosis of epidermodysplasia verruciformis (EV). Histopathology from verrucous lesion was consistent with the diagnosis of wart [Figure - 4]. The finding of palmar pits in EV patients is extremely rare, and only one case has been reported in English literature so far.
 |
| Figure 1: Multiple hypopigmented pityriasis versicolor-like lesions on back |
 |
| Figure 2: Multiple hyperpigmented verruca plana-like lesions on dorsum of hand |
 |
| Figure 3: Close up view of palmar pits |
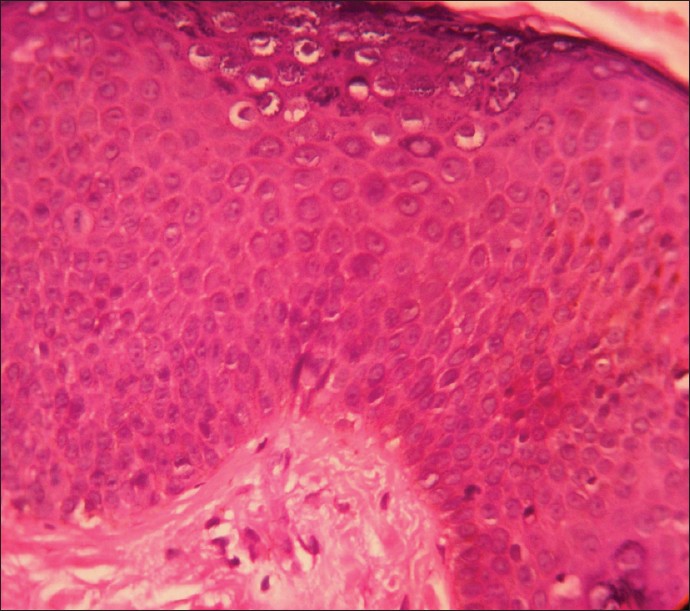 |
| Figure 4: Acanthosis and prominent koilocytes. (H and E, ×400) |
Palmar pits have always fascinated dermatologists. Classically, it is found in Pitted keratolysis, Arsenical keratosis, Darier′s disease, Acrokeratosis verruciformis of Hopf, Reticulate acropigmentation of Kitamura, Nevoid basal cell carcinoma syndrome (Gorlin syndrome), Cowden syndrome, Basaloid follicular hamartoma (familial form), Generalized follicular hamartoma, Porokeratosis, Dupuytren′s contracture, Lichen nitidus, Lichen planus, Psoriasis, Porokeratotic eccrine ostial and dermal duct nevus (PEODDN), Keratosis punctata of palmar creases, Focal acral hyperkeratosis and Mal de Meleda type of palmoplantar keratoderma. Some rarer associations include Histoplasmosis, [4] Hailey Hailey disease, [5] Sarcoidosis, [6] and EV. [3] EV is believed to be caused by defect in specific cell mediated immunity, which makes affected persons susceptible to persistent cutaneous infection by specific human papilloma viruses (HPV). Such strains, called EV types, are rarely reported in immunocompetent patients. About two dozen EV-specific HPV types have been identified; a subset (mainly types 5 and 8) is associated with skin cancers in EV patients. EV usually manifests in childhood with highly polymorphic widespread lesions, which is clinically characterized by combination of pityriasis versicolor (PV)-like hypopigmented lesions, verruca plana-like lesions and seborrhoeic keratosis-like verrucous plaques. These PV-like lesions, especially in sun exposed areas, have higher risk of developing squamous cell carcinoma (SCC). These SCC are usually multiple and locally invasive, but have low metastatic potential. [1] The authors do not exclude the possibility of chance association of EV and palmar pits; however, they believe that multiple examples of co-occurrence of two rare conditions must go beyond chance association. So far, two (including ours) such cases have been documented. The association will be further strengthened if more such cases are reported.
| 1. |
Sterling JC. Virus Infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 7 th ed. West Sussex: Wiley Blackwell Publishers; 2004. p. 25.58-9.
th ed. West Sussex: Wiley Blackwell Publishers; 2004. p. 25.58-9. '>[Google Scholar]
|
| 2. |
De D, Narang T, Dogra S, Kanwar AJ. Asymptomatic palmar pits: clinical evaluation of six cases and review of the literature. J Cutan Med Surg 2008;12:198-202.
[Google Scholar]
|
| 3. |
Galadari I, Abdul Aal J. Epidermodysplasia verruciformis: Report of a case with palmar pits. Cutis 1993;52:53-5.
[Google Scholar]
|
| 4. |
Lindgren AM, Fallon JD, Horan RF. Psoriasiform papules in the acquired immunodeficiency syndrome. Disseminated histoplasmosis in AIDS. Arch Dermatol 1991;127:722-3.
[Google Scholar]
|
| 5. |
Verbov JL. Palmar lesions in familial benign pemphigus. Br J Dermatol 1969;81:77.
[Google Scholar]
|
| 6. |
Morrison JG. Sarcoidosis in a child, presenting as an erythroderma with keratotic spines and palmar pits. Br J Dermatol 1976;95:93-7.
[Google Scholar]
|
Fulltext Views
11,997
PDF downloads
2,060





