Translate this page into:
Papular lesions on the vulva
Corresponding author: Dr. Niharika Dhattarwal, Department of Dermatology and STD, OPD 5th floor VMMC and Safdarjung Hospital, Delhi, India. niharika.pgirtk@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dhattarwal N, Kapil K. Papular lesions on the vulva. Indian J Dermatol Venereol Leprol. 2024;90:530-1. doi: 10.25259/IJDVL_587_2023
A 40-year-old woman presented with skin-coloured, mildly itchy raised lesions on her vulva for 2–3 years. On examination, multiple, firm, freely mobile, non-tender papules of approximately 1 cm size were present on the bilateral labia majora [Figure 1]. One of the papules was excised and sent for histopathological examination [Figures 2a and 2b].

- Skin-coloured papules present on the vulva.
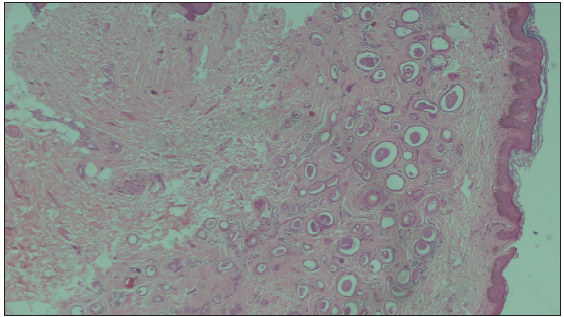
- Histopathology showing multiple variable-sized eccrine tubules with secretions and lined with a double layer of epithelium along with a few immature pilar structures (Haematoxylin & Eosin; 100x).
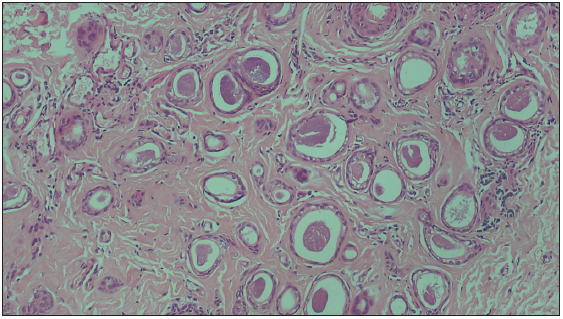
- Some of the eccrine ducts have elongated tails of epithelial cells giving them a comma-shaped or tadpole appearance (Haematoxylin & Eosin; 400x).
Question
What is your diagnosis?
Diagnosis
Vulvar syringomas
Discussion
Syringomas are benign appendageal tumours derived from the intraepidermal part of eccrine glands. The estimated prevalence is 1% worldwide.1 Exact aetiopathogenesis remains elusive. Hormonal influence is suggested as they are commonly seen in women, increase in size during pregnancy, in the premenstrual period, and with oral contraceptives.2 Some authors also suggest a possible effect of race as higher incidence is seen in Asians and African Americans.3 The role of inflammation and association with other autoimmune diseases like alopecia areata and vitiligo also need careful interpretation.1 The most common age group is adolescence and peripubertal but may also occur in children and elderly postmenopausal women.
Syringomas are classified into four types:
-
1.
Local type: Most common, seen in the periorbital area.
-
2.
Generalised (multiple and eruptive) types: Affecting two or more anatomical sites, seen on the neck, anterior chest, abdomen, and/or axilla, and associated with hereditary or systemic diseases such as hyperthyroidism, diabetes, Marfan’s syndrome, and Ehlers–Danlos syndrome.1
-
3.
Down syndrome-associated type.
-
4.
Familial type: Autosomal dominant, seen in unusual sites like the palms and neck.
Vulvar involvement is uncommon and can be seen in localised and eruptive types.4 In a study of 90 cases of eruptive syringomas, only one patient had vulvar involvement.1 Isolated vulvar syringomas without any extragenital involvement are even rarer. Clinically, there are three types of presentations:
-
1.
Papular type (most common): Multiple skin-coloured, brown, or slightly yellow papules in a symmetrical distribution are present. Usually asymptomatic and patients often delay seeking treatment.
-
2.
Cystic type: Milia-like whitish cysts are seen.
-
3.
Lichenified type: The pruritus is very severe leading to lichenification and even pseudohypertrophy of the vulva.4
In a report of two cases of localised vulvar syringomas by Pai et al., both patients had papular-type lesions.2
Diagnosis is obtained by clinicopathological correlation. In histopathology, ductal structures lined by a double layer of flattened cuboidal epithelium with small nuclei are seen along with amorphous material in the lumen, suggestive of eccrine differentiation. A characteristic diagnostic feature is the presence of tail-like elongation from one end of the duct into the stroma known as a ‘tadpole’ or ‘comma’ appearance. Dermoscopy may also provide a clue to the diagnosis. Some authors have reported the presence of distinct variable-sized, glittering yellow-whitish structures over a fading pink background. Others have also noticed ill-defined, brown incomplete pigment networks and delicate vascular networks.5
Other differentials for papular lesions on the vulva include Fox-Fordyce disease, epidermal cysts, milia, senile angiomas, condyloma acuminata, and steatocystoma multiplex.
Medical treatment options administered with success include topical atropine, topical adelmidrol, topical steroids, tretinoin, oral tranilast, and intradermal botulinum toxin. Destructive modalities like CO2 lasers, electrocautery, cryotherapy, and surgical excision can also be performed.1
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Eruptive syringomas: Summary of ninety cases and a brief literature review. J Cosmet Dermatol. 2023;22:1128-33.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar syringoma – A rare distribution of a common entity: Report of two cases. J Dermatol Dermatol Surg. 2020;24:140-2.
- [Google Scholar]
- Late-onset of eruptive syringomas: A diagnostic challenge. An Bras Dermatol. 2015;90:239-41.
- [CrossRef] [PubMed] [Google Scholar]
- Vulvar syringomas as a part of nonfamilial generalized eruptive form: Unusual lesions leading to pseudohyper-trophy of the labia majora. Dermatol Online J 2018:2413030/qt1rx2v8hc.
- [Google Scholar]
- Eruptive syringoma: Two cases with dermoscopic features. Skin Appendage Disord 2020:6319-22.
- [Google Scholar]





