Translate this page into:
Papular mucinosis associated with monoclonal gammopathy of unknown significance
Correspondence Address:
Sarvesh S Thatte
Department of Dermatology, Seth G. S. Medical College and K.E.M Hospital, Parel, Mumbai
India
| How to cite this article: Thatte SS, Dongre AM, Chikhalkar SB, Khopkar US. Papular mucinosis associated with monoclonal gammopathy of unknown significance. Indian J Dermatol Venereol Leprol 2015;81:213-214 |
Sir,
Papular mucinosis or lichen myxedematosus is a disorder of cutaneous mucin deposition. It usually presents as small, firm, waxy papules, plaques or nodules predominantly localized to upper and lower extremities and/or trunk but can be generalized. There can be underlying systemic involvement. [1],[2]
A 38-year-old married woman presented with multiple, skin colored, slightly itchy, raised lesions over upper extremities, trunk, lower extremities, and both ears for 4 months. There was no history of pain, spontaneous resolution of lesions or loss of sensations. On examination, general condition of the patient was fair and she was of average built. Multiple, well defined, skin colored, waxy, firm, 1-3 mm papules were present over both upper [Figure - 1]a and lower extremities, chest, abdomen, and back with mild diffuse thickening of both ear lobes [Figure - 1]b. Koebner phenomenon was present over both upper extremities [Figure - 2], thighs, and abdomen. Palms, soles, nails, mucosae, genitalia, and the rest of the examination revealed no abnormality. Considering the differential diagnoses of eruptive lichen planus, lichen nitidus, granuloma annulare and warts, a skin biopsy was taken from one of the papules.
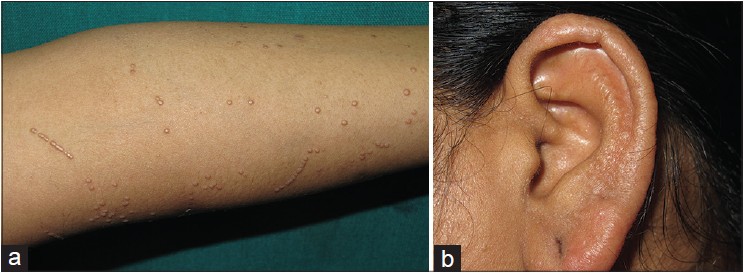 |
| Figure 1: (a) Multiple, skin colored, discrete, 1– 3 mm papules with Koebner phenomenon. (b) Diffuse thickening of ear lobe |
 |
| Figure 2: Koebner phenomenon |
Routine investigations revealed normal complete blood count and serum biochemistry with hemoglobin 11.3 g/dl, total leukocyte count 7300/cu.mm, platelets 3.73 lacs/cu.mm, total protein 6.8 g/dl, albumin: globulin ratio 1.3, SGPT/SGOT 23/25 U/l, blood urea nitrogen 15 mg/dl, and serum creatinine 0.8 mg/dl. Urine routine and microscopic examination did not reveal any abnormality. Histopathology of individual papules revealed mucin deposition in the upper dermis [Figure - 3]a, which stained positive with Alcian blue [Figure - 3]b. On further investigation, 24 hour urinary proteins were raised to 1.2 g and serum protein electrophoresis revealed M band (0.5 g%) in gamma region. Level of serum immunoglobulins were normal except lambda light chain, which was raised (962 mg/dl, normal: 313-723 mg/dl). Urinary Bence Jones proteins were absent and the whole body bone scan was normal. Bone marrow examination revealed 5% normal plasma cells. Based on clinical examination, histopathology, serum protein electrophoresis and bone marrow biopsy findings, a final diagnosis of papular mucinosis associated with monoclonal gammopathy of unknown significance was made. The patient was started on topical steroids and tablet methotrexate 7.5 mg/week and is currently under follow up.
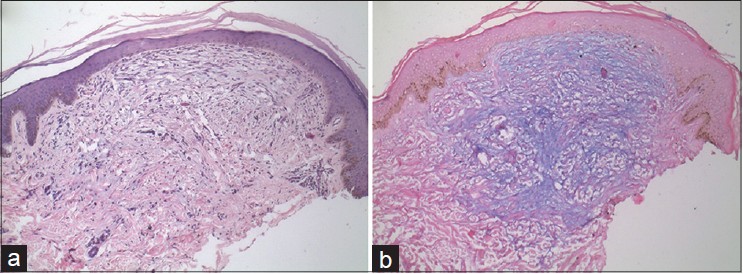 |
| Figure 3: (a) Mucin deposition (blue) in upper dermis (H and E, ×10). (b) Alcian blue staining of mucin (Alcian blue, ×10) |
The cutaneous mucinoses are a heterogeneous group of disorders in which an abnormal amount of mucin accumulates in the skin, either discretely or diffusely. [1],[2] Papular mucinosis can present as a localized papular eruption or a generalized lichenoid papular eruption. [2] It usually presents with small, firm, waxy papules that are limited to a few sites. [1],[2] Disease is usually associated with paraproteinemia, generally with IgG light chains. [2],[3] Koebner phenomenon refers to the appearance of lesions similar to a dermatosis at distinct uninvolved sites following trauma and is classically seen in psoriasis, lichen planus, vitiligo, warts and lichen nitidus. However, Koebner phenomenon has also been mentioned in lichen myxedematosus in some reports. [3],[4] Yamazaki et al. reported a case of lichen myxedematosus with exacerbated skin lesions after ultraviolet B (UVB) irradiation, which they considered to be due to Koebner phenomenon (photo-koebnerization). [4] Cather and Menter reported a case of papular mucinosis in a 33-year-old African-American woman who had Koebner phenomenon along the areas of scratching along with IgG-λ monoclonal gammopathy on serum electrophoresis and mild plasmacytosis in the bone marrow. [3]
In our patient, skin lesions along with findings on histopathology confirmed the diagnosis of papular mucinous. In addition the patient had associated monoclonal gammopathy of unknown significance (MGUS) as confirmed on serum protein electrophoresis and bone marrow biopsy. Koebner phenomenon was present over upper extremities, abdomen and thighs. The condition needs to be differentiated from granuloma annulare, amyloidosis, sarcoidosis, lichen nitidus, lichen planus, warts, and eruptive collagenomas. [1],[2] Localized lichen myxedematosus or papular mucinosis does not require any specific treatment. In severe lichen myxedematosus or scleromyxedema with or without systemic involvement, various treatment modalities like melphalan, cyclophosphamide, methotrexate, chorambucil, acitretin, interferon-alpha, and psoralen plus UVA (PUVA) are effective to some extent. [1],[2],[3]
In conclusion, whether papular mucinosis represents a true plasma cell dyscrasia is unknown as multiple myeloma ensues rarely in these patients. [3] Presence of Koebner phenomenon in papular mucinosis is rarely mentioned in literature.
| 1. |
Rongioletti F, Rebora A. Mucinoses. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2 nd ed. Spain: Elsevier Limited; 2008. p. 611-21.
[Google Scholar]
|
| 2. |
Kumar B, Dogra S. Metabolic Disorders. In: Walia RG, Walia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai: Bhalani Publishing House; 2008. p. 1307-9.
[Google Scholar]
|
| 3. |
Cather JC, Menter MA. Diffuse eruption of pigmented papules. Proc (Bayl Univ Med Cent) 2001;14:185-6.
[Google Scholar]
|
| 4. |
Yamazaki S, Fujisawa T, Yanatori A, Yamakage A. A case of lichen myxedematosus with clearly exacerbated skin eruptions after UVB irradiation. J Dermatol 1995;22:590-3.
[Google Scholar]
|
Fulltext Views
6,572
PDF downloads
2,327





