Translate this page into:
Papulonecrotic tuberculid at the site of tuberculin test in a patient with concomitant erythema induratum and papulonecrotic tuberculid
Correspondence Address:
Atul M Dongre
Department of Skin and VD, OPD No. 117, Seth GS Medical College and KEM Hospital, Parel, Mumbai-400 012
India
| How to cite this article: Dongre AM, Sanghavi SA, Khopkar US. Papulonecrotic tuberculid at the site of tuberculin test in a patient with concomitant erythema induratum and papulonecrotic tuberculid. Indian J Dermatol Venereol Leprol 2013;79:248-251 |
Sir,
The tuberculids represent a group of disorders resulting from hypersensitive immune reactions within the skin due to hematogenous dissemination of Mycobacterium tuberculosis (MTB) (or its antigens) from a primary source, occurring in a patient with strong antituberculous cell-mediated immunity. [1] The concomitant occurrence of two tuberculids in a patient is rare. [2]
A 36-year-old female presented with multiple painful red lesions on both legs, associated with swelling and pain in both knee joints since 4 months.She also had multiple asymptomatic raised red lesions on both the forearms, dorsum of hands, and back of same duration as lesions on legs. She was not suffering from cough, fever, or weight loss. She had no past history of tuberculosis (TB) or contact with case of TB. She had undergone tuberculin testing 2 days back.
On examination, multiple, tender erythematous nodules measuring 2 × 3 cm in size on both calves and lateral side of legs were seen [Figure - 1]. She also had multiple, erythematous to violaceous papules over both the forearms [Figure - 2], dorsum of hands, and a few over the back. Examination of tuberculin test site revealed indurated plaque (20 × 18 mm) and multiple erythematous papules at the periphery of the positive tuberculin reaction [Figure - 3]. There was no evidence of lymphadenopathy and hepatosplenomegaly, and rest of her systemic examination was unremarkable.
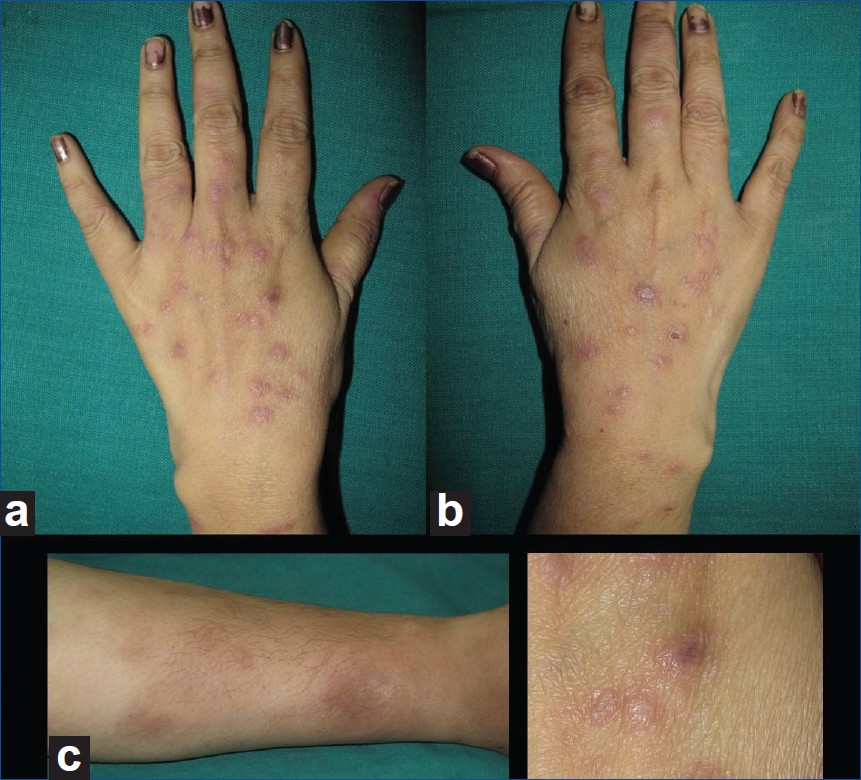 |
| Figure 1: (a) Erythematous papules with a dusky center on dorsum of hand; (b) Erythematous nodules on leg; (c) Close up of the lesions on dorsum of hand |
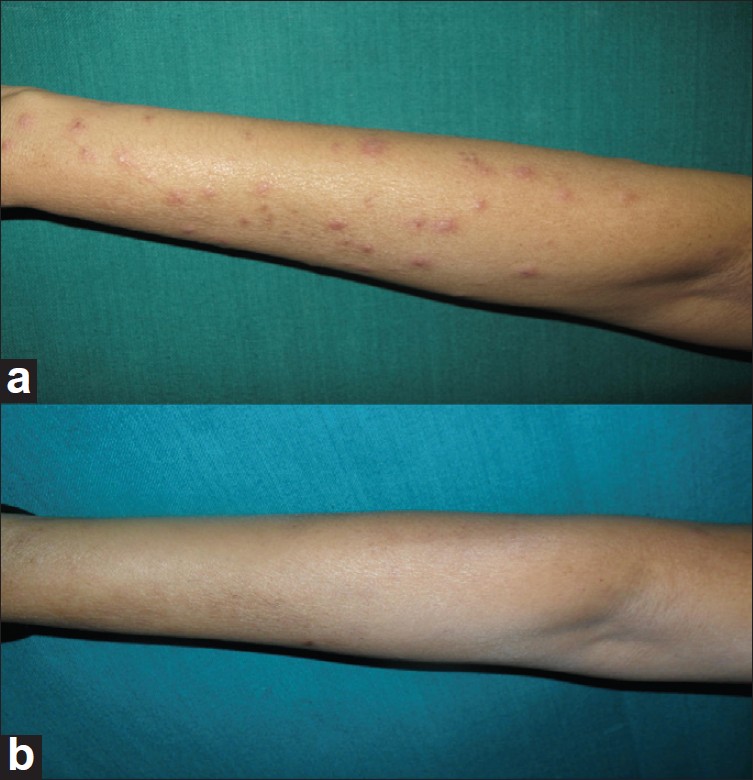 |
| Figure 2: (a) Erythematous papules on the forearm; (b) resolution of lesions after antituberculous treatment |
 |
| Figure 3: (a) Erythematous papules around the site of tuberculin test (b) disappearance of lesions following antituberculosis treatment |
Her routine blood investigations (Hb, complete blood count, liver, and renal function tests) were normal except for markedly raised erythrocyte sedimentation rate (ESR) (110 mm/hr). Chest X-ray and abdominal ultrasonography examination were normal. Her enzyme-linked immunosorbent assay (ELISA) test for HIV was negative.
Biopsy of the tender nodule on the leg revealed lobular panniculitis, fat necrosis, granulomatous infiltrate, and vasculitis which were suggestive of erythema induratum (EI) [Figure - 4]. Biopsies of the papule on forearm and the papule around the site of tuberculin test revealed similar histopathological appearance, i.e., wedge-shaped area of necrosis involving the dermis, overlying epidermis along, and vasculitis at the base of necrotic dermis. Moderately dense lymphohistiocytic infiltrate was noted in the surrounding dermis. In a single focus, collection of lymphocytes, histiocytes, and epitheliod cells forming a granuloma was seen in the dermis. Polymerase chain reaction (PCR) test (nested amplification technique) of the biopsy taken from the nodule over the leg was positive for 123 base pair sequence which is considered specific for MTB complex.
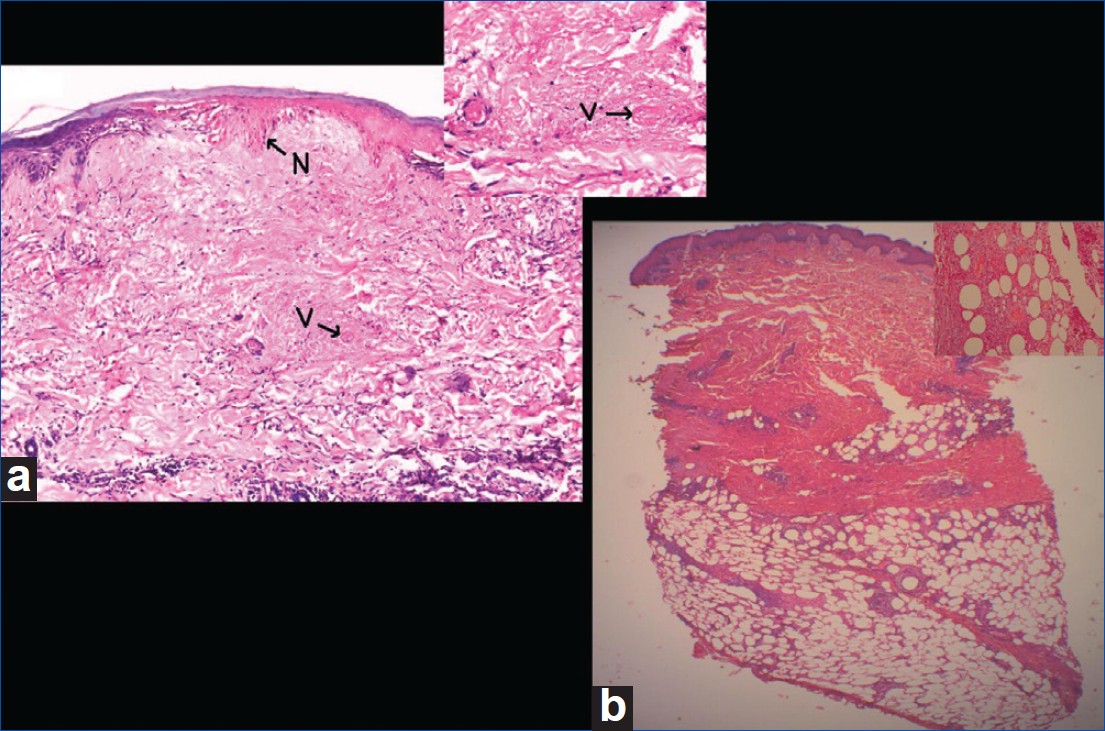 |
| Figure 4: (a) Wedge-shaped necrosis involving epidermis and the dermis marked as arrow and letter N (H and E, × 50). Inset shows deposition of fibrin in the vessel walls and lumina along with nuclear dust marked as arrow and letter V (H and E, × 400); (b) Infiltrate in the subcutaneous tissue (H and E, × 25). Inset shows lobular panniculitis, granulomatous infiltrate, and vasculitis (H and E, × 400) |
In view of clinicopathological features, she was started on standard antituberculous regimen consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol. At the end of 1 month, complete disappearance of lesions [Figure - 2]b including lesions at the site of tuberculin test was seen [Figure - 3]b.
The term tuberculid was coined by Darier in 1896. [3] EI, papulonecrotic tuberculid (PNT), and lichen scrofulosorum are generally classified as true tuberculids, i.e., skin manifestations of TB in which no organisms can be demonstrated on acid-fast bacteria (AFB) stain or on culture of the skin lesions.
EI presents as tender, erythematous nodules on the lower legs which have chronic recurrent course and female preponderance. The lesions may ulcerate and heal with depressed scars. Histologically, lobular panniculitis with vasculitis and caseation necrosis are seen.
PNT occurs as crops of symmetric, small, erythematous, inflammatory papules which have an acral and extensor surface predilection. Lesions may undergo central ulceration and heal spontaneously within weeks, leaving varioliform scars. Microscopically, wedge-shaped area of necrosis is seen with underlying vasculitis and granulomatous infiltrate.
Though in the lesions of tuberculids, bacilli cannot be demonstrated on AFB stain or culture, tuberculous etiology is suggested by a significantly positive tuberculin test, demonstration of MTB by PCR in the lesions, and prompt resolution of the condition on antituberculous therapy. Failure to demonstrate tubercle bacilli in lesions of tuberculids probably occurs due to presence of only a very few number of bacilli in skin lesions which may be rapidly destroyed by a locally delayed hypersensitivity reaction, or may be killed upon arrival. [1]
Advanced investigations like PCR to demonstrate mycobacterial DNA in the lesions of tuberculids have been found helpful to validate this entity and MTB to be the underlying causative agent. The amplified 123-bp sequence is considered specific for M. tuberculosis complex. [4]
Though the techniques like PCR are helpful to prove the role of tuberculous infection, a low detection rate for primary tuberculous foci has been reported at the time of appearance of tuberculids. For PNT, the frequency of locating extracutaneous TB foci varies from 26% to 67% in various series. For EI, the evidence for TB was found in 5 out of 20 cases in one series. [5] Newer techniques like interferon (IFN) gamma release assays (IGRAs), e.g. Quantiferon-TB gold assay, are useful to diagnose latent tuberculous infections. [6]
A very few cases of simultaneous occurrence of one type of tuberculid with other have been reported in literature. Occurrence of EI with lichen scrofulosorum, lichen scrofulosorum with PNT has been reported. Occurrence of tuberculids with other form of cutaneous or internal focus of MTB infection has been documented.Simultaneous occurrence of EI and PNT has been reported sporadically in literature. Our extensive literature search showed that less than 15 such cases have been reported. [2] In these case reports, females outnumber the males in a ratio of 4:1. The sites of predilection for both the tuberculids were legs. The general condition of these patients was generally good and constitutional symptoms were absent. It is assumed that simultaneous presence of EI and PNT in a patient may represent a morphological continuum where immune-mediated vasculitis and delayed hypersensitivity reaction occur at different levels leading to appearance of lesions of two different morphologies. Thappa has reported an unusual presentation where transformation from PNT to lichen scrofulosorum occurred in a child. [5] The occurrence of PNT lesions at the site of tuberculin testing has not been reported earlier. However, popular tuberculid eruptions following Bacillus Calmette Guerin (BCG) vaccination have been reported. [6]
Though TB is very common in developing countries like India, such simultaneous occurrence of PNT and EI has not been reported from India. However, such occurrence in two Indian females has been documented from UK. [7],[8]
Thus, we report a rare case of concomitant EI and PNT with interesting observation of occurrence of PNT lesions at the site of tuberculin test, which has not been reported earlier. We propose that, in our case, occurrence of lesions of PNT at the site of tuberculin test indicates strong immune reaction against the tuberculin purified protein derivative (PPD) and validates the theory of occurrence of tuberculids as a hypersensitivity reaction to tuberculous antigen.
| 1. |
Degitz K, Steidl M, Thomas P, Plewig G, Volkenandt M. Aetiology of tuberculids. Lancet 1993;341:239-40.
[Google Scholar]
|
| 2. |
Chuang YH, Kuo TT, Wang CM, Wang CN, Wong WR, Chan HL. Simultaneous occurrence of papulonecrotic tuberculide and erythema induratum and the identification of Mycobacterium tuberculosis DNA by polymerase chain reaction. Br J Dermatol 1997;137:276-81.
[Google Scholar]
|
| 3. |
Darier MJ. Des ''tuberculides'' cutanees. Arch Dermatol Syph 1896;7:1431-6.
[Google Scholar]
|
| 4. |
Eisenach KD, Cave MD, Bates JH, Crawford JT. Polymerase chain reaction amplification of a repetitive DNA sequence specific for Mycobacterium tuberculosis. J Infect Dis 1990;161:977-81.
[Google Scholar]
|
| 5. |
Thappa DM, Karthikeyan K, Jayanthi S. Tuberculid in a child: Transformation from papulonecrotic to lichen scrofulosorum. Pediatr Dermatol 2003;20:91-3.
[Google Scholar]
|
| 6. |
Muto J, Kuroda K, Tajima S. Papulartuberculides post-BCG vaccination: Case report and review of the literature in Japan. Clin Exp Dermatol 2006;31:611-2.
[Google Scholar]
|
| 7. |
Milligan A, Chen K, Graham-Brown RA. Two tuberculides in one patient-a case report of papulonecrotic tuberculide and erythema induratum occurring together. Clin Exp Dermatol 1990;15:21-3.
[Google Scholar]
|
| 8. |
Roblin D, Kelly R, Wansbrough-Jones M, Harwood C. Papulonecrotic tuberculide and erythema induratum as presenting manifestations of tuberculosis. J Infect 1994;28:193-7.
[Google Scholar]
|
Fulltext Views
4,043
PDF downloads
1,062





