Translate this page into:
Paradigm shift in antinuclear antibody negative lupus: Current evidence
2 Department of Dermatology, Katihar Medical College, Katihar, Bihar, India
Correspondence Address:
Anup Kumar Tiwary
Department of Dermatology, Venereology and Leprosy, Government Medical College and Hospital, Haldwani, Uttarakhand
India
| How to cite this article: Tiwary AK, Kumar P. Paradigm shift in antinuclear antibody negative lupus: Current evidence. Indian J Dermatol Venereol Leprol 2018;84:384-387 |
Introduction
Systemic lupus erythematosus is an autoimmune multi-system disease most commonly involving skin, joints and vasculature. Owing to its protean clinical manifestations, it could be under-diagnosed or over-diagnosed. To minimize incorrect diagnosis of systemic lupus erythematosus, several clinical and laboratory features are included in the diagnostic and classification criteria. Antinuclear antibody assay, although an old screening test, still plays a pivotal role in diagnosis. But, it has to be correctly performed on properly chosen antigenic substrate and correctly interpreted.
Most laboratories use bead-based multiplex tests, solid phase assays or immunofluorescence technique using liver or kidney tissue substrates of rat/mice for testing for antinuclear antibodies. The reasons for choosing these methods are lower cost, simplicity and easiness in standardization of these tests. But limited antigenicity of the substrate used for testing lead to lower sensitivity of these tests.[1] Consequently, the concept of antinuclear antibody negative lupus emerged and several cases of antinuclear antibody negative lupus were published in the literature around the world. The prevalence of antinuclear antibody negative lupus was even pegged as 5–10%.[2]
Need to Revisit 'antinuclear Antibody Negative Lupus' and its Causes
Unlike multiplex/solid phase assays or IF-ANA assays using rodent substrates, rapidly dividing human epithelial cell line expresses more nuclear antigens resulting in greater sensitivity. Rodent tissue does not express Ro (SS-A) antigen. Human epithelial cell line expresses other nuclear and nucleolar antigens more readily as well.[3] With increasing use of human epithelial cell line substrates for antinuclear antibody testing during the past decade, cases of systemic lupus erythematosus seronegative for antinuclear factors have become rare. Moreover, many reported cases of systemic lupus erythematosus who were wrongly labelled as “antinuclear antibody negative lupus” became antinuclear antibody positive on serial testing with immunofluorescence utilizing human epithelial cell line substrate.[1] This, coupled with lack of information about the laboratory methods employed for antinuclear antibody assay in a majority of published cases of antinuclear antibody negative lupus raised a question mark on the accuracy of diagnosis of these cases.
In this changed scenario, prevalence of true antinuclear antibody negative lupus seems to be less than 2%.[4] Furthermore, there are certain clinical factors to be kept in mind when interpreting antinuclear antibody test results in suspected cases of systemic lupus erythematosus before jumping to conclusions.[5]
Causes for False Antinuclear Antibody Negative Lupus
Questionable or incorrect diagnosis of 'lupus'
Incorrect diagnosis of systemic lupus erythematosus has led to an increase in the reporting of antinuclear antibody negative cases. Hence, before proceeding to antinuclear antibody assay and interpreting its results, it is necessary to consider the accuracy of provisional diagnosis. No diagnostic method has 100% sensitivity and 100% specificity in systemic lupus erythematosus. Even histopathologic examination or systemic lupus international collaborating clinics 2012 diagnostic criteria cannot rule out the possibility of “false-positive” diagnosis. It has been reported that the diagnosis of “lupus” in approximately 78% cases of “antinuclear antibody negative lupus” reported between 1976 and 2003 around the globe were based on insufficient clinical data and laboratory findings, not even fulfilling the American College of Rheumatology criteria for systemic lupus erythematosus.[1] Hence, before commenting on antinuclear antibody reactivity of suspected cases of lupus, we need to confirm such cases in the best possible way, so that non-lupus or doubtful cases of lupus are not mis- reported as antinuclear antibody negative lupus.
Antigenic deficient substrate and leaching of antigens
The most important and critical factor in antinuclear antibody test is the substrate used for it. The result of the test is based on the availability of sufficient substrate antigen to react with the autoantibody. Inadequacy or deficiency of the antigen due to poor choice of the substrate can lead to false-negative antinuclear antibody results. Human epithelial cell line appears to be a more suitable substrate than rodent tissue. It is possible that an antinuclear antibody negative patient may become antinuclear antibody positive if the substrate is changed from rat liver to human epithelial cell line.[1]
Inadequate fixation of the substrate leading to leaching of the antigens may also result in a false-negative antinuclear antibody test.[6]
Concurrent immunosuppressive treatment
Review by Simmons et al. identified seven cases which were antinuclear antibody negative at presentation, butlater became seropositive. The interval to develop seropositivity for antinuclear antibody ranged from five months to 10 years, with a median of six years. Of importance, all these patients were on one or more of immunosuppressive drugs.[7] It is now being increasingly recognized that immunosuppressants can alter antinuclear antibody results. Hence, details of previous or concurrent medications should always be reviewed before interpretation of results of antinuclear antibody assay. Most of the earlier published cases of antinuclear antibody negative systemic lupus erythematosus suffered from incomplete documentation of concurrent and previous medications.[1] This raises doubts about the accuracy of diagnosis of antinuclear antibody negative lupus in many reported cases.
Persistent renal loss of proteins
Proteinuria is a prominent feature of systemic lupus erythematosus and profound and persistent renal loss of immunoglobulins may result in false antinuclear antibody negative result. This fact also explains those cases of antinuclear antibody negative lupus with profound proteinuria reported by Persellin and Takeuchi, who became antinuclear antibody positive after treatment with prednisolone and chlorambucil.[8] In such cases, detection of antinuclear antibody in pleural fluid and urine may be helpful, as noted by Ferreiro et al.[2] Clinicians should be aware of the possibility of false antinuclear antibody negativity in the presence of marked proteinuria. Serial testing of serum samples is warranted in such cases.
National Committee for Clinical Laboratory Standards Guidelines for Antinuclear Antibody Testing by Indirect Immunofluorescence
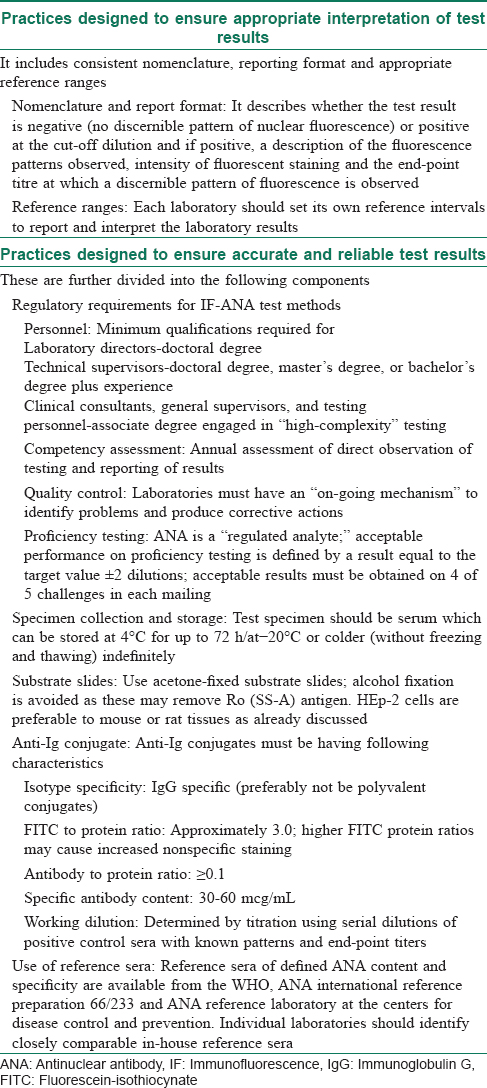
Variations in antinuclear antibody testing methods may have profound impact on the diagnosis and management of lupus patients. Attempts have been made to standardize laboratory testing for antinuclear antibodies. In December 1996, National Committee for Clinical Laboratory Standards proposed certain recommendations to be followed during antinuclear antibody testing by immunofluorescence technique.[9] These are categorized into two groups for better understanding. [Table - 1].
Limitations of immunofluorescence-antinuclear antibody test
- Inter-method standardization of immunofluorescence-antinuclear antibody substrates and anti-Ig conjugates is still difficult [9]
- There is no standard protocol for reference ranges in the background of variable prevalence of weakly positive antinuclear antibody results in healthy persons.
Current Established Cases of True Antinuclear Antibody Negative Lupus
On reviewing evidence from literature, it becomes apparent that there are only some case reports or series which followed proper technical guidelines to diagnose antinuclear antibody negative lupus. The features that establish the diagnosis of systemic lupus erythematosus unequivocally are high-titre anti-double stranded DNA antibody, anti-Sm (Smith) antibody, biopsy-proven kidney disease or biopsy-proven skin disease. One can make a diagnosis of antinuclear antibody negative lupus if at least one of these features has been documented and due care (as described earlier) has been taken in interpreting the laboratory findings of antinuclear antibody.[10] Searching through the PUBMED database, an attempt has been made to review the cases of antinuclear antibody negative lupus reported in the last 15 years [Table - 2].[7],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28] Based on the confounding factors taken into consideration in this review, out of 19 previously diagnosed cases of antinuclear antibody negative lupus, only two cases deserved to be called as 'true antinuclear antibody negative lupus'. On scrutinizing, true antinuclear antibody negative lupus appears to constitute less than 2% of all systemic lupus erythematosus patients.

Look Before You Leap to Antinuclear Antibody Negative Lupus!!
Based on the use of human cell line derived substrates current NCCLS guidelines for testing and interpretation and considering various clinical and technical factors which can affect the results, it becomes clear that the term 'antinuclear antibody negative lupus' should not be used for labelling any suspicious case of systemic lupus erythematosus. True antinuclear antibody negative lupus appears to be extremely rare. Serial antinuclear antibody assay has to be done in such cases.
Limitations
As we have reviewed antinuclear antibody negative cases of lupus reported in the past 15 years using PUBMED database, it is possible that we may have missed cases of lupus enlisted under other databases. Second limitation of this review is the doubtful reliability of old American College of Rheumatology criteria to label a case as true or questionable lupus. Considering the complex and unpredictable clinical presentations of systemic lupus erythematosus and low specificity of old American College of Rheumatology criteria, it may not be correct to label cases which do not fulfil four of the American College of Rheumatology criteria as non-lupus. Third limitation is the lack of sufficient clinical and laboratory information in many cases. Conclusions made on such incomplete data may not be valid.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Cross LS, Aslam A, Misbah SA. Antinuclear antibody-negative lupus as a distinct diagnostic entity – Does it no longer exist? QJM 2004;97:303-8.
[Google Scholar]
|
| 2. |
Ferreiro JE, Reiter WM, Saldana MJ. Systemic lupus erythematosus presenting as chronic serositis with no demonstrable antinuclear antibodies. Am J Med 1984;76:1100-5.
[Google Scholar]
|
| 3. |
Maddison PJ, Provost TT, Reichlin M. Serological findings in patients with “ANA-negative” systemic lupus erythematosus. Medicine (Baltimore) 1981;60:87-94.
[Google Scholar]
|
| 4. |
Worrall JG, Snaith ML, Batchelor JR, Isenberg DA. SLE: A rheumatological view. Analysis of the clinical features, serology and immunogenetics of 100 SLE patients during long-term follow-up. Q J Med 1990;74:319-30.
[Google Scholar]
|
| 5. |
Wallace DJ, Linker-Israeli M. It's not the same old lupus or Sjögren's any more: One hundred new insights, approaches, and options since 1990. Curr Opin Rheumatol 1999;11:321-9.
[Google Scholar]
|
| 6. |
Koller SR, Johnston CL Jr., Moncure CW. Lupus erythematosus cell preparation-antinuclear factor incongruity. A review of diagnostic tests for systemic lupus erythematosus. Am J Clin Pathol 1976;66:495-505.
[Google Scholar]
|
| 7. |
Simmons SC, Smith ML, Chang-Miller A, Keddis MT. Antinuclear antibody-negative lupus nephritis with full house nephropathy: A case report and review of the literature. Am J Nephrol 2015;42:451-9.
[Google Scholar]
|
| 8. |
Persellin RH, Takeuchi A. Antinuclear antibody-negative systemic lupus erythematosus: Loss in body fluids. J Rheumatol 1980;7:547-50.
[Google Scholar]
|
| 9. |
Kavanaugh A, Tomar R, Reveille J, Solomon DH, Homburger HA. Guidelines for clinical use of the antinuclear antibody test and tests for specific autoantibodies to nuclear antigens. American college of pathologists. Arch Pathol Lab Med 2000;124:71-81.
[Google Scholar]
|
| 10. |
Lahita RG. The clinical presentation of systemic lupus erythematosus. In: Lahita RG, Tsokos G, Buyon JP, Koike T, editors. Systemic Lupus Erythematosus. 5th ed. New York: Elsevier; 2011. p. 525-35.
[Google Scholar]
|
| 11. |
Locham KK, Jaswir S, Rajinder G, Manjit S, Chanchal J. Case report; ANA negative lupus erythematosus. Indian Pediatr 2000;37:540-2.
[Google Scholar]
|
| 12. |
Maraina CH, Kamaliah MD, Ishak M. ANA negative (Ro) lupus erythematosus with multiple major organ involvement: A case report. Asian Pac J Allergy Immunol 2002;20:279-82.
[Google Scholar]
|
| 13. |
Sugisaki K, Takeda I, Kanno T, Nogai S, Abe K, Sakuma H, et al. An anti-nuclear antibody-negative patient with systemic lupus erythematosus (SLE) accompanied with anti-ribosomalPantibody (anti-P). Intern Med 2002;41:1047-51.
[Google Scholar]
|
| 14. |
Pratap DV, Reddy SK, Rani SC, Krishna VA, Indira D. ANA-negative systemic lupus erythematosus. Indian J Dermatol Venereol Leprol 2004;70:243-4.
[Google Scholar]
|
| 15. |
Eilertsen GØ, Nossent JC. Erythroleukaemia complicating ANA-negative systemic lupus erythematosus. Scand J Rheumatol 2007;36:478-80.
[Google Scholar]
|
| 16. |
Kim HA, Chung JW, Park HJ, Joe DY, Yim HE, Park HS, et al. An antinuclear antibody-negative patient with lupus nephritis. Korean J Intern Med 2009;24:76-9.
[Google Scholar]
|
| 17. |
Akhoondian J, Rezaii Yazdi Z, Behmanesh F, Talebi S. Cerebritis and neutropenia in a child with ANA negative lupus. Iran J Child Neurol 2009;3:61-6.
[Google Scholar]
|
| 18. |
Caltik A, Demircin G, Bülbül M, Erdogan O, Akyüz SG, Arda N, et al. An unusual case of ANA negative systemic lupus erythematosus presented with vasculitis, long-standing serositis and full-house nephropathy. Rheumatol Int 2013;33:219-22.
[Google Scholar]
|
| 19. |
Xie Q, Liu Y, Yang N, Yin G. Antinuclear antibody-negative systemic lupus erythematosus in a case with pregnancy. Rheumatol Int 2012;32:3273-6.
[Google Scholar]
|
| 20. |
Chaubey VK, Chhabra L. Cold agglutinin-induced haemolysis in association with antinuclear antibody-negative SLE. BMJ Case Rep 2013. doi: 10.1136/bcr-2013-009337.
[Google Scholar]
|
| 21. |
Yang HC, Hong MJ, Lim JH, Jang SA, Jeon SY, Yoo WH. A case of ANA-negative, anti-dsDNA negative, and anti-Ro/SSA positive membranous lupus nephropathy. J Rheum Dis 2013;20:127-31.
[Google Scholar]
|
| 22. |
Elcioglu OC, Ozkok A, Bakan A, Tuncan S, Ozluk Y, Kilicarslan I, et al. A case of full-house nephropathy with anti-nuclear antibody negative lupus. Turk Nephrol Dial Transplant 2014;23:161-3.
[Google Scholar]
|
| 23. |
Hoang V, Addison D, Lakkis N, Tabbaa R. ANA-negative lupus presenting with heart failure and severe valvular dysfunction: Case report and review of the literature. Methodist Debakey Cardiovasc J 2015;11:186-8.
[Google Scholar]
|
| 24. |
Chikkalingaiah KB. Seronegative lupus membranous nephropathy. Int J Case Rep Images 2016;7:624-7.
[Google Scholar]
|
| 25. |
Zhao M. ANA-negative presentation of SLE in man with severe autoimmune neutropenia. Case Rep Med 2016;2016:6853936.
[Google Scholar]
|
| 26. |
Tiwary AK, Mishra DK. ANA-negative systemic lupus erythematosus with targetoid lesions: Rowell syndrome or just a rare presentation of lupus erythematosus. J Pak Assoc Dermatol 2016;26:269-72.
[Google Scholar]
|
| 27. |
Changal KH, Sofi F, Altaf SS, Raina A, Raina AH. ANA negative systemic lupus erythematosus leading to CTEPH, TTP-like thrombocytopenia, and skin ulcers. Case Rep Rheumatol 2016;2016:4507247.
[Google Scholar]
|
| 28. |
Cerqueira SG, Castro RA, Abreu RM, Sampaio S, Pereira PR, Nunes AT, et al. Lupus nephritisin a patient without evidence of systemic lupus erythematosus. Port J Nephrol Hypert 2017;31:59-62.
[Google Scholar]
|
Fulltext Views
6,420
PDF downloads
3,295





