Translate this page into:
Paraffinoma of the penis and scrotum (sclerosing granuloma of the male genitalia)
2 Department of Pathology, Biotechnology Unit, Torrecardenas Hospital, Almeria, Spain
3 Department of Dermatology and Venereology, La Mancha General Hospital, Ciudad Real, Spain
4 Department of Pathology, Biotechnology Unit, High-resolution Hospital, Public Health Agency Business Bajo Guadalquivir, Utrera, Seville, Spain
Correspondence Address:
Francisco Javier Velasco-Albendea
Department of Pathology, Biotechnology Unit, Torrecardenas Hospital, Hermandad de Donantes de Sangre s/n, 04009 Almeria
Spain
| How to cite this article: Alcalde-Alonso M, Velasco-Albendea FJ, Soto-Díaz A, Gómez-Avivar P, Torres-Gómez FJ. Paraffinoma of the penis and scrotum (sclerosing granuloma of the male genitalia). Indian J Dermatol Venereol Leprol 2017;83:75-77 |
Sir,
Liquid fatty materials have been injected into the penis and scrotum since the 19th century, usually by non-professionals, in a bid to increase the size of the genitalia and enhance sexual performance.[1] Paraffinoma of the penis and scrotum (sclerosing granuloma of genitalia) that can result from this practice is easily diagnosed by histopathology. Though it is uncommon, there have been several case reports of this condition. Since most patients deny previous injections, a skin biopsy showing oily material, foreign-body granulomas and fibrosis is essential to the diagnosis.[2]
A 28-year-old male immigrant from Russia, where he had been a soldier, presented with progressive thickening of the scrotum and prepuce that he ascribed to a tank-related injury sustained 8 years earlier. He denied significant medical history or drug intake. On examination, the external genitalia were markedly swollen [Figure - 1]. The prepuce was thickened, fixed and could not be retracted but the glans penis was not involved. The scrotum was fibrotic with loss of hair. The pubis was also affected with elongated subcutaneous nodules. Small inguinal lymph nodes were palpable bilaterally. Laboratory tests (full blood counts, basic biochemistry and antinuclear antibodies) and a chest X-ray were normal. Although he denied local injections of any foreign substance, exogenous lipid administration was clinically suspected. A probable diagnosis of sclerosing lipogranuloma was made and a skin biopsy was taken from the prepuce.
 |
| Figure 1: Fibrotic, deformed and swollen external genitalia |
Histopathologic examination revealed severe full-thickness involvement of the dermis with marked collagenization, and a chronic infiltrate comprising lymphocytes, plasma cells and eosinophils [Figure - 2]. In the deep dermis [Figure - 3], lipid vacuoles were visible, surrounded by prominent foreign body granulomas with some foamy macrophages, epithelioid histiocytes and isolated multinucleated giant cells. A definitive diagnosis of penile and scrotal paraffinoma (secondary sclerosing lipogranuloma) was made.
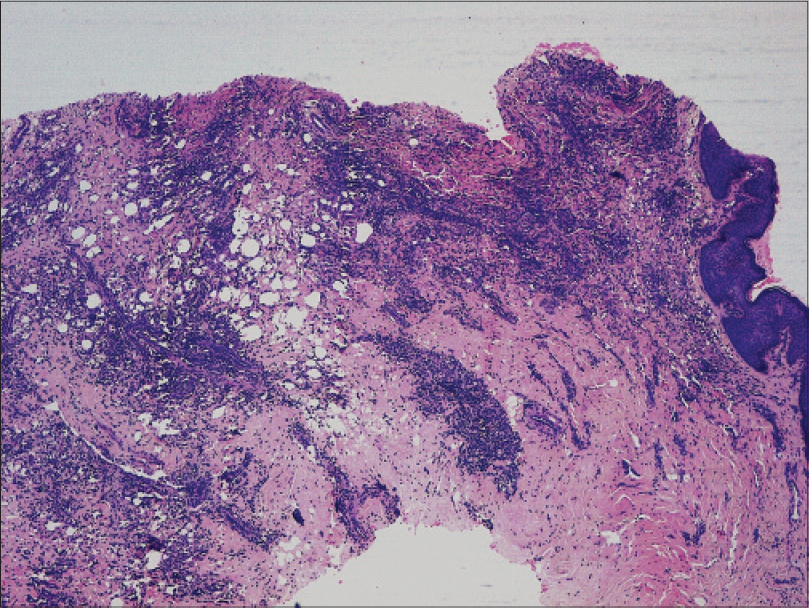 |
| Figure 2: Dermal fibrosis in association with multiple scattered lipid vacuoles and a prominent chronic inflammatory infiltrate (H and E, ×100) |
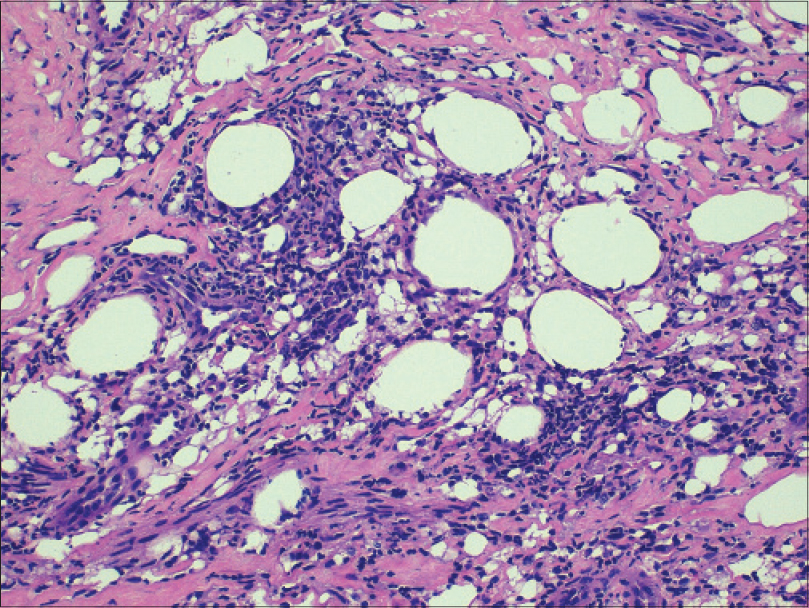 |
| Figure 3: Lipid vacuoles with a chronic granulomatous inflammatory reaction in the deep dermis (H and E, ×200) |
On enquiring again, the patient admitted that he had received several paraffin injections 8 years ago for penis augmentation. He refused any further treatment and was lost to follow-up.
Penile self-injection of various oils has given rise to a number of acute and chronic complications including necrosis, ulceration, infection, fistulization, deformity, erectile dysfunction, phimosis and even acute urinary retention. Nevertheless, this procedure is still practiced, particularly in jails and military facilities in Eastern Europe, Thailand and Korea.[1],[2],[3]
Sclerosing lipogranuloma has been reported as either a primary idiopathic entity or as a consequence of injury, inflammation or injection of oily substances (paraffin, vaseline, mineral oil, cod liver oil and petroleum jelly) into soft tissues. In the latter case, the term paraffinoma is regarded as more appropriate.[1],[2],[3] Paraffinoma development has also been reported during treatment with interferon alfa-2a.[4]
Clinical features include irregular, indurated nodules displaying varying degrees of sclerosis. The prepuce, penile shaft, scrotum and pubis are the sites most commonly involved; however, oily substances can migrate to subcutaneous tissues, muscles and lymph nodes.[1],[2],[3] Treatment involves complete surgical excision of the foreign material and fibrotic tissue followed by closure with direct suture, skin grafts or flaps. Incomplete excision frequently leads to recurrence. Extensive and invasive cases can be very difficult to treat and early detection of patients with penile augmentation by oily liquids is essential since the best results tend to be achieved when the granuloma is not highly developed and does not involve deep structures.[1],[2],[3],[4],[5] Some authors have obtained good results in patients with paraffinoma-induced full necrosis of penile skin using a Y-V incision to prevent penile shortening, together with a bipedicular scrotal flap.[6] Oral and intralesional corticosteroids may be of some value during acute flare-ups, but the duration and frequency of administration are not well established.[1],[2]
In the clinical differential diagnosis, depending on the stage, other causes of subcutaneous nodules of the male genitalia, scleroderma, infiltrative lesions such as those in storage diseases or malignancies (squamous cell carcinoma) should be considered, as also infectious diseases, both sexually transmitted and others. Magnetic resonance imaging, fine-needle aspiration cytology and sonography may provide valuable clues in the differential diagnosis; histological examination usually confirms the diagnosis.
In conclusion, clinicians need to be aware of this entity, especially given the frequent difficulty in obtaining a reliable history from patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Foxton G, Vinciullo C, Tait CP, Sinniah R. Sclerosing lipogranuloma of the penis. Australas J Dermatol 2011;52:e12-4.
[Google Scholar]
|
| 2. |
Lee T, Choi HR, Lee YT, Lee YH. Paraffinoma of the penis. Yonsei Med J 1994;35:344-8.AQ
[Google Scholar]
|
| 3. |
De Siati M, Selvaggio O, Di Fino G, Liuzzi G, Massenio P, Sanguedolce F, et al. An unusual delayed complication of paraffin self-injection for penile girth augmentation. BMC Urol 2013;13:66.
[Google Scholar]
|
| 4. |
Bachmeyer C, Moguelet P, Gombeaud T, Sbidian E, Aractingi S. Penile paraffinoma developing during treatment with pegylated interferon alfa-2a for chronic hepatitis C virus infection. Arch Dermatol 2011;147:1232-3.
[Google Scholar]
|
| 5. |
Nyirády P, Kelemen Z, Kiss A, BánfiG, Borka K, Romics I. Treatment and outcome of vaseline-induced sclerosing lipogranuloma of the penis. Urology 2008;71:1132-7.
[Google Scholar]
|
| 6. |
Kim SW, Yoon BI, Ha US, Kim SW, Cho YH, Sohn DW. Treatment of paraffin-induced lipogranuloma of the penis by bipedicled scrotal flap with Y-V incision. Ann Plast Surg 2014;73:692-5.
[Google Scholar]
|
Fulltext Views
6,492
PDF downloads
3,630





