Translate this page into:
Patch tests with commercial hair dye products in patients with allergic contact dermatitis to para-phenylenediamine
2 Department of Dermatology, Busan St. Mary's Hospital, Busan, South Korea
3 Department of Dermatology, Severance Hospital, Yonsei University College of Medicine, Seoul, South Korea
4 Department of Dermatology, School of Medicine, Pusan National University; Biomedical Research Institute, Pusan National University Hospital, Busan, South Korea
5 Department of Dermatology, School of Medicine, Pusan National University; Research Institute for Convergence of Biomedical Science and Technology, Pusan National University, Yangsan Hospital, Busan, South Korea
Correspondence Address:
Hyun-Chang Ko
Department of Dermatology, Pusan National University Yangsan Hospital, Geumo-ro 20, Mulgeum-eup, Yangsan-si, Gyeongsangnam-do 626-770
South Korea
| How to cite this article: Lee HJ, Kim WJ, Kim JY, Kim HS, Kim BS, Kim MB, Ko HC. Patch tests with commercial hair dye products in patients with allergic contact dermatitis to para-phenylenediamine. Indian J Dermatol Venereol Leprol 2016;82:645-650 |
Abstract
Background: Hair dye is one of the most common causes of allergic contact dermatitis. The main allergen has been identified as para-phenylenediamine. To prevent the recurrence of contact dermatitis to para-phenylenediamine, patients should discontinue the use of para-phenylenediamine-containing hair dye products. However, many patients are unable to discontinue their use for cosmetic or social reasons. Sometimes, they continue to have symptoms even after switching to so-called “less allergenic” hair dyes. Objectives: To evaluate the safety of 15 commercially available hair dye products in patients with allergic contact dermatitis due to para-phenylenediamine. Methods: We performed patch tests using 15 hair dyes that were advertised as “hypoallergenic,” “no para-phenylenediamine” and “non-allergenic” products in the market. Results: Twenty three patients completed the study and 20 (87.0%) patients had a positive patch test reaction to at least one product. While four (26.7%) hair dye products contained para-phenylenediamine, 10 (66.7%) out of 15 contained m- aminophenol and 7 (46.7%) contained toluene-2,5-diamine sulfate. Only one product did not elicit a positive reaction in any patient. Limitations: Small sample size and possibility of false-positive reactions. Conclusions: Dermatologists should educate patients with allergic contact dermatitis to para-phenylenediamine about the importance of performing sensitivity testing prior to the actual use of any hair dye product, irrespective of how it is advertised or labelled.Introduction
Most patients with contact dermatitis due to hair dye have positive patch test results to para-phenylenediamine and contact with para-phenylenediamine must be strictly avoided to prevent a recurrence. For social and personal reasons, however, continued use of hair dye is important to some people. Some recently introduced hair dyes are advertised as “hypoallergenic,” “para-phenylenediamine free,” or “non-allergenic.” However, some of these products do not clearly state the contents of the hair dye and sensitive consumers have difficulty finding a hair dye that is safe for them. Moreover, sometimes even so-called “safe” hair dyes can trigger contact dermatitis. There is a paucity of reports or clinical studies on the prevention of recurrent contact dermatitis due to hair dye and about which hair dye may be safe for para-phenylenediamine-sensitive patients.
In this study, we patch tested 27 patients with hair dye allergic contact dermatitis and para-phenylenediamine sensitivity with 15 hair dye products marketed as “hypoallergenic,” “para-phenylenediamine-free,” or “non-allergenic”, in order to identify safe hair dye products for consumers with sensitivity to hair dye.
Methods
The study included 27 patients with allergic contact dermatitis to hair dye who visited Pusan National University Hospital from May 2010 to June 2011 and who had para-phenylenediamine sensitivity identified by the Korean standard antigen patch test series (Chemotechnique ®, Vellinge, Sweden). Subjects volunteered to be part of the study after they were explained the purpose, process and possible problems arising from patch testing. The study was approved by the Institutional Review Board of Pusan National University Hospital (clinical trial number: F2010004).
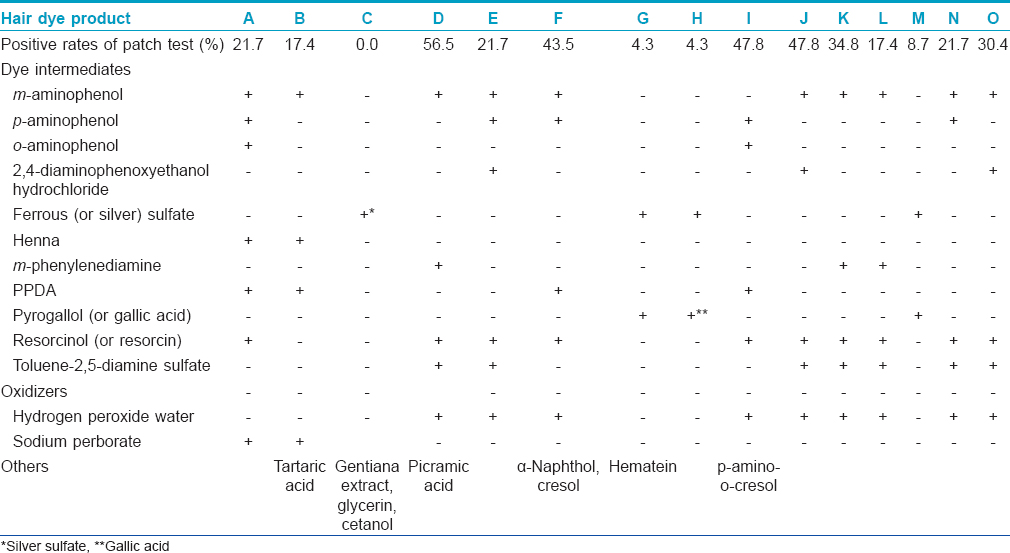
All patients were re-tested for para-phenylenediamine sensitivity with the Korean standard antigen patch test series following which they were patch tested with 15 hair dyes advertised as “hypoallergenic,” “para-phenylenediamine-free,” or “non-allergenic.” Although the research staff tried to contact the producers of the hair dyes for accurate content information, the product information used for the study was obtained from the commercial packing of the hair dyes or their package inserts. Common ingredients present in the 15 hair dye products studied were tabulated and categorized by their roles, such as dye intermediate, oxidizer and others [Table - 1].
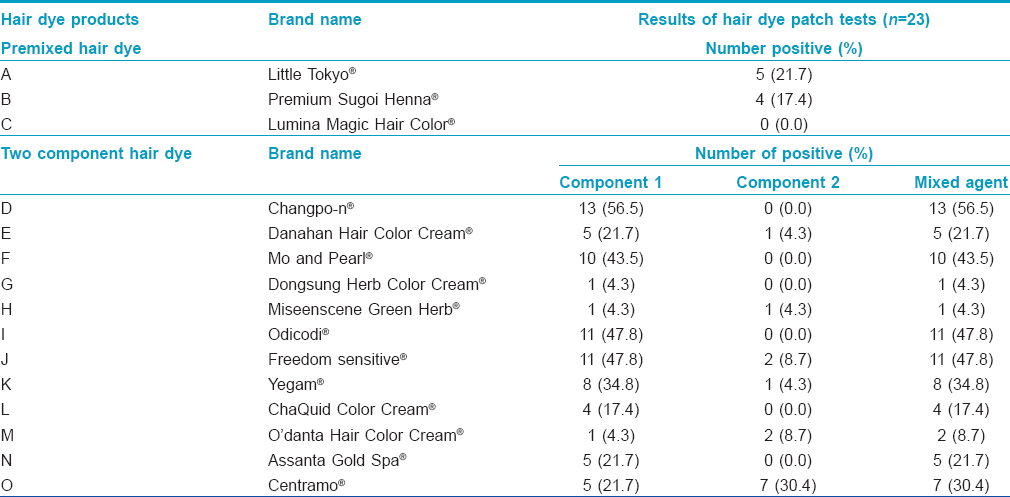
The hair dyes used for patch testing were designated as “A-C” for 3 premixed products and “D-O” for 12 products that had two separate components, number 1 and number 2, to be mixed before use. The premixed hair dyes (A–C) were patch tested “as is” while the two components of 12 hair dye products (D–O) and their mixtures were patch tested separately. The patch test was performed using 15 µL of each hair dye product (1% in pet) by the Finn chamber method (Finn chambers on Scanpor; Epitest®, Tuusula, Finland).[1],[2] The patch test units were applied on the upper back and subjects returned after 48 hours (day 2) for the primary reading that was made 30 minutes after the removal of patches. The final reading was made on day 4 and results were graded according to International Contact Dermatitis Research Group standards.[3] Readings of 1+ or higher, persisting on day 4, were considered significant for final analysis.
Results
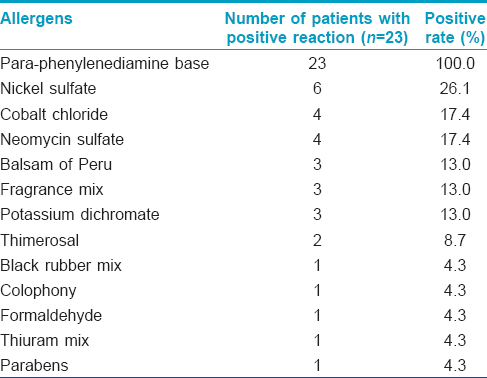
The data of only 23 patients was available for final analysis as four patients did not complete the study either due to severe skin rashes or by choice. These 23 patients included 10 (43.5%) men and 13 (56.5%) women of average age 58.7 ± 9.6 years. All of them had positive patch tests to para-phenylenediamine on previous testing with the Korean standard antigen series with 1+ reactions in 14 (60.9%) patients, 2+ reactions in 5 (21.7%) and 3+ reactions in 4 (17.4%). Antigens, other than para-phenylenediamine that yielded positive reactions included nickel sulfate (26.1%), cobalt chloride (17.4%), neomycin sulfate (17.4%), Balsam of Peru (13.0%), fragrance mix (13.0%) and potassium dichromate (13.0%) [Table - 2].
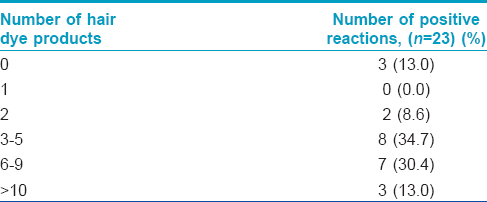
Of the 23 patients, 20 (87.0%) patients tested positive with more than one hair dye; 2 (8.6%) patients had positive patch tests to two hair dyes, 8 (34.7%) patients to 3–5 types of hair dyes, and 7 (30.4%) patients to 6–9 hair dyes. Three (13.0%) patients had positive patch tests to more than 10 types of hair dyes [Table - 3] and [Figure - 1]. Three patients did not react positively to any of the tested dyes. Patients who showed positive patch test reactions to hair dye component numbers 1 or 2 also had positive reactions to their respective mixtures.
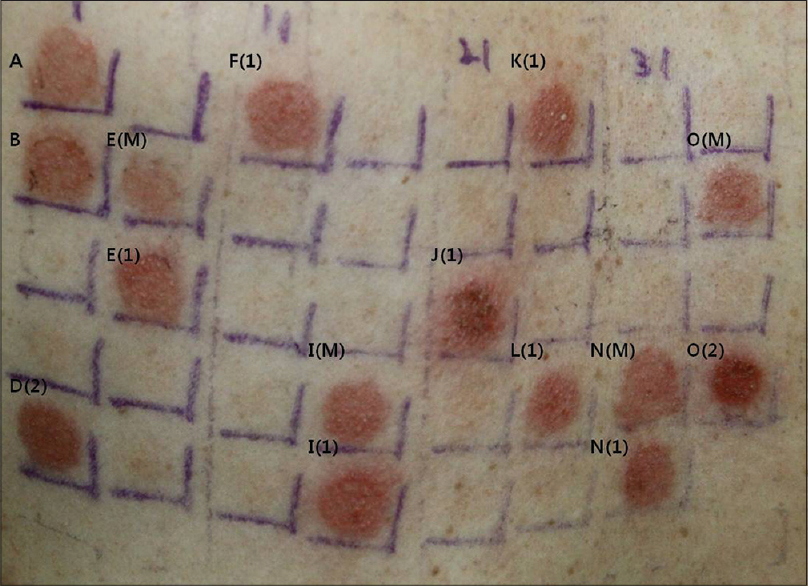 |
| Figure 1: The patient with positive patch test reactions to 13 types of hair dye products (1): Component 1 (2): Component 2 (M): Mixed agent |
Thirteen (56.5%) patients had positive reactions to “D” hair dye, 11 (47.8%) patients had positive reactions to “I” and “J” hair dyes, while 10 (43.5%) patients and 8 (34.8%) patients had positive reactions to “F” and “K” hair dyes, respectively. On the other hand, only one patient each had positive reactions to the “G” and “H” hair dye products, while “C” hair dye product did not elicit a positive reaction in any of the patients. For the premixed (A–C) hair dye products, 21.7%, 17.4% and 0% of patients had positive reactions, respectively. As for the 12 hair dyes with two components (numbers 1 and 2), all the components number 1 elicited positive reactions, while only half the components number 2 did the same. In six hair dye products (D, F, G, I, L and N), components number 2 elicited no reaction in any patient [Table - 4].
[Table - 1] lists all dye intermediates and oxidizers present in each of the tested hair dyes. We found that 11 (73.3%) hair dyes contained aminophenol(s) (which cross reacts with para-phenylenediamine). Ten (66.7%) hair dyes (A, D, E, F, I, J, K, L, N and O) had resorcinol, an ingredient in phenol dyes, 7 (46.7%) hair dyes had toluene-2,5-diamine sulfate (which also cross reacts with para-phenylenediamine) and 4 (26.7%) hair dyes (C, G, H and M) had ferrous sulfate or silver sulfate which yield black or brown colors on oxidization. Four (26.7%) hair dyes (A, B, F and I) contained para-phenylenediamine and 3 (20.0%) contained m- phenylenediamine; 3 (20.0%) contained 2,4-diaminophenoxyethanol hydrochloride, a synthetic coloring and 3 (20.0%) contained pyrogallol or gallic acid which are position isomers of para-phenylenediamine. Pyrogallol and gallic acid are phenol substances in the leaves and roots of plants, with strong reducibility in aqueous states and are used to dye hair brown. Henna (Lawsonia inermis), known as a natural dye, was present in two hair dye products (A, B). With regard to oxidizers, 9 (60.0%) hair dyes had hydrogen peroxide and 2 (13.3%) hair dyes had sodium perborate. Tartaric acid, gentian extract, glycerin, cetanol, picramic acid, α - naphthol, cresol, hematein and p- amino-o- cresol were also found in some hair dyes (6.7%).
Discussion
Para-phenylenediamine is an effective dye ingredient that, when mixed with other ingredients, enables black or other color dyes to dye hair permanently. It is also one of the most important antigens responsible for allergic contact dermatitis to hair dye.[4] In cases of allergic contact dermatitis, avoiding exposure to the causative allergen is the most important measure leading to improvement of symptoms and prevention of recurrence but hair dyeing is often deemed necessary for social and personal reasons. Several hair dyes are now advertised to be “hypoallergenic,” “para-phenylenediamine-free,” or “non-allergenic”, and many consumers choose their hair dyes based on these advertisements. However, a significant number of patients visit hospitals for allergic contact dermatitis after using such products necessitating accurate identification of the allergen to prevent recurrences. Although open patch testing has been successfully used to determine sensitivity due to any particular hair dye,[5],[6] we preferred the closed Finn chamber method because we wanted to test multiple dye products. During our preliminary study of five patients whom we subjected to open patch tests and 48 h contact time with 15 hair dyes, the results were ambiguous in all but one patient This happened because of wiping, smearing and mixing of different hair dyes due to body movements and contact with clothes during the procedure and also caused discomfort to some patients.
Of the 23 patients, 20 (87%) patients had positive patch test reactions to more than one hair dye product. Contrary to the initial expectation, para-phenylenediamine was responsible for positivity in only four hair dyes (A, B, F, I). However, the positivity rates of these four hair dyes ranged from 17.4% to 56.5%, in our study sample, unlike the 100% positivity observed with the Korean standard antigen series. As has been suggested previously, low exposure concentration of para-phenylenediamine in these four hair dyes could be one of the explanations for this dissociation of results.[4],[7] The para-phenylenediamine concentration used in the Korean standard antigen series is 1.0% while it is perhaps <1.0% in these four hair dyes. However, this explanation remains unsubstantiated as these four hair dyes, despite listing para-phenylenediamine as their main ingredient, did not specify its concentration. Similarly, the six hair dyes (E, J, K, L, N, O), having toluene-2,5-diamine sulfate instead of para-phenylenediamine yielded high rates of positive patch test results (17.4–47.8%). The three hair dye products (A, B, F) with m- aminophenol, but without para-phenylenediamine or toluene-2,5-diamine sulfate, also yielded high rates of positive patch tests between 17.4% and 47.8% [Table - 3] and [Table - 4]. These high positivity rates can be attributed to cross-reaction between toluene-2,5-diamine sulfate or m- aminophenol and para-phenylenediamine, that is well known to cross-react with “para-amino” complexes, such as benzocaine, procaine and para-aminobenzoic acid, azo/aniline category hair dye and amine substances.[8],[9] The low positive patch test reaction rates (0–8.7%) of the other four hair dyes (C, G, H, M) [Table - 4] that do not contain substances capable of cross-reacting with para-phenylenediamine also lend support to this hypothesis. Of the various dye intermediates, only henna has been reported to cause allergic contact dermatitis in henna-tattoos and that is attributed by most to para-phenylenediamine added to enhance its outcome color.[10],[11],[12],[13],[14] However, henna, though present in two hair dyes tested, did not elicit positive reactions in this study.
The two premix hair dye products (A, B) which contained the oxidizer sodium perborate each showed positive rates of 21.7% and 17.4%, respectively [Table - 3] and [Table - 4]. However, these products also contained para-phenylaminediamine. The oxidizers, i.e. components number 2, of nine hair dye products (D, E, F, I, J, K, L, N, O) showed positive reactions ranging from 0% to 30.4%. Conventionally, the component number 1 is a dye intermediate and component number 2 is an oxidizer. However, it is not always possible to identify them as number 1 or number 2 in the absence of clear marking by the manufacturer, and that was also noted by us. Similarly, substances advertised as the unique characteristics of the products, such as charcoal, squid ink, mulberry extract, herb, mugwort and ginseng, swertia, green mud and pearl were not labeled. It appears that the high positive rates from premixed hair dyes “A” and “B” were probably due to the oxidizer para-phenylenediamine and/or aminophenol while the wide range of positive rates (0–30.4%) from component number 2 in nine products (D, E, F, I, J, K, L, N, O) could be due to contents that are not labeled by the manufacturer.
Small sample size, the possibility of false positive reactions due to closed patch testing and the difficulties in delineating the putative allergen in the hair dyes for lack of information on the product contents are some of the limitations of this study.
Conclusions
Although many hair dye products available in the market are advertised as “hypoallergenic,” “no para-phenylenediamine,” “non-allergenic” and so on, they may contain either small amounts of para-phenylenediamine or other substances that cross-react with para-phenylenediamine causing allergic contact sensitivity in a significant number of patients despite claimed safety. Patients with hair dye contact dermatitis must always choose their hair dye by checking the contents and not going by high-pitched advertisements that may often be misleading and use a particular hair dye only after skin tests are negative. Dermatologists must educate patients with allergic contact dermatitis to para-phenylenediamine about the significance of performing sensitivity testing every time prior to actual use of any hair dye product.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Reitschel R, Fowler J, Alexander A. Preservatives and vehicles in cosmetics and toiletries. In: Fisher's Contact Dermatitis. 6th ed. Ontario: BC Decker Inc.; 2008. p. 266-318.
[Google Scholar]
|
| 2. |
Fischer T, Maibach H. Finn chamber patch test technique. Contact Dermatitis 1984;11:137-40.
[Google Scholar]
|
| 3. |
Lee EK, Lee JY, Kim HO. A study of as is patch test in cosmetic contact dermatitis. Ann Dermatol 1999;11:207-13.
[Google Scholar]
|
| 4. |
Hextall JM, Alagaratnam NJ, Glendinning AK, Holloway DB, Blaikie L, Basketter DA, et al. Dose-time relationships for elicitation of contact allergy to para-phenylenediamine. Contact Dermatitis 2002;47:96-9.
[Google Scholar]
|
| 5. |
Krasteva M, Cristaudo A, Hall B, Orton D, Rudzki E, Santucci B, et al. Contact sensitivity to hair dyes can be detected by the consumer open test. Eur J Dermatol 2002;12:322-6.
[Google Scholar]
|
| 6. |
Krasteva M, Cottin M, Cristaudo A, Laine detected by the consumeet al. Sensitivity and specificity of the consumer open skin allergy test as a method of prediction of contact dermatitis to hair dyes. Eur J Dermatol 2005;15:18-25.
[Google Scholar]
|
| 7. |
Goebel C, Coenraads PJ, Rothe H, Kunze G, Kock M, Schlatter H, et al. Elicitation of the immune response to p-phenylenediamine in allergic patients: The role of dose and exposure time. Br J Dermatol 2010;163:1205-11.
[Google Scholar]
|
| 8. |
Basketter DA, English J. Cross-reactions among hair dye allergens. Cutan Ocul Toxicol 2009;28:104-6.
[Google Scholar]
|
| 9. |
Reitschel R, Fowler J, Alexander A. Specific instructions for patients with common contact allergens. In: Fisher's Contact Dermatitis. 6th ed. Ontario: BC Decker Inc.; 2008. p. 731-41.
[Google Scholar]
|
| 10. |
Kazandjieva J, Balabanova M, Kircheva K, Tsankov N. Contact dermatitis due to temporary henna tattoos. Skinmed 2010;8:191-2.
[Google Scholar]
|
| 11. |
Lazandjieva J, Balahlager S. Contact dermatitis after temporary henna tattoos osan increasing phenomenon. Swiss Med Wkly 2001;131:199-202.
[Google Scholar]
|
| 12. |
Calogiuri G, Foti C, Bonamonte D, Nettis E, Muratore L, Angelini G. Allergic reactions to henna-based temporary tattoos and their components. Immunopharmacol Immunotoxicol 2010;32:700-4.
[Google Scholar]
|
| 13. |
Kazandjieva J, Grozdev I, Tsankov N. Temporary henna tattoos. Clin Dermatol 2007;25:383-7.
[Google Scholar]
|
| 14. |
Kang IJ, Park HH, Lee MH. A case of contact dermatitis from henna tattooing. Korean J Dermatol 2005:43:413-5.
[Google Scholar]
|
Fulltext Views
9,348
PDF downloads
2,237





