Translate this page into:
Patient-physician relationship in patients with psoriasis
Correspondence Address:
Matteo Megna
Department of Dermatology, University of Naples Federico II, Via Pansini, 5, 80131 Napoli
Italy
| How to cite this article: Patruno C, Ayala F, Megna M, Napolitano M, Balato N. Patient-physician relationship in patients with psoriasis. Indian J Dermatol Venereol Leprol 2012;78:228 |
Sir,
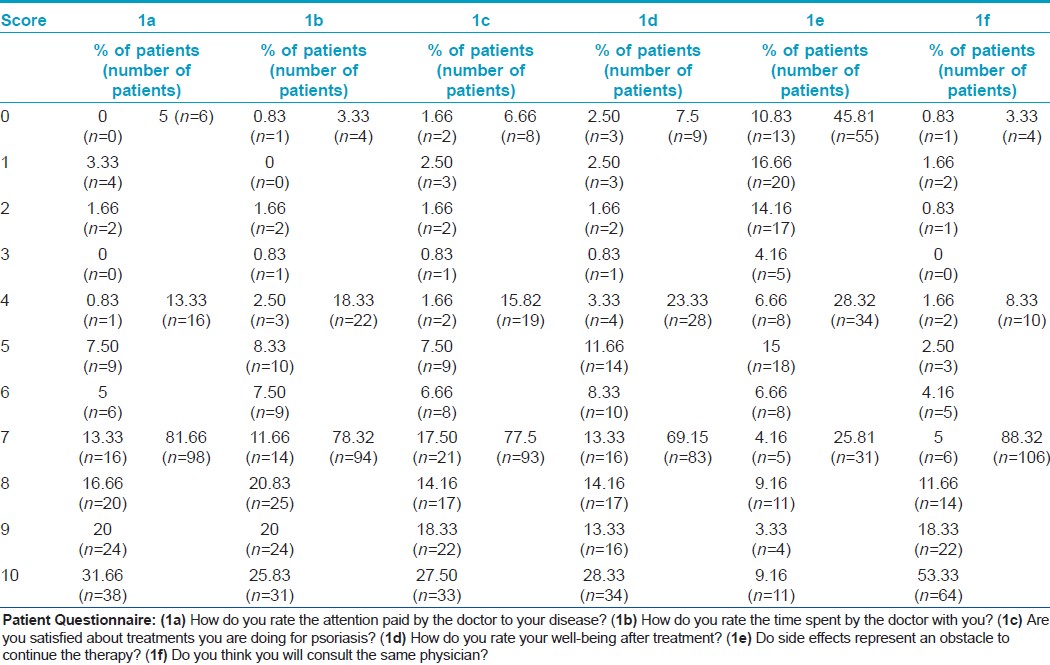
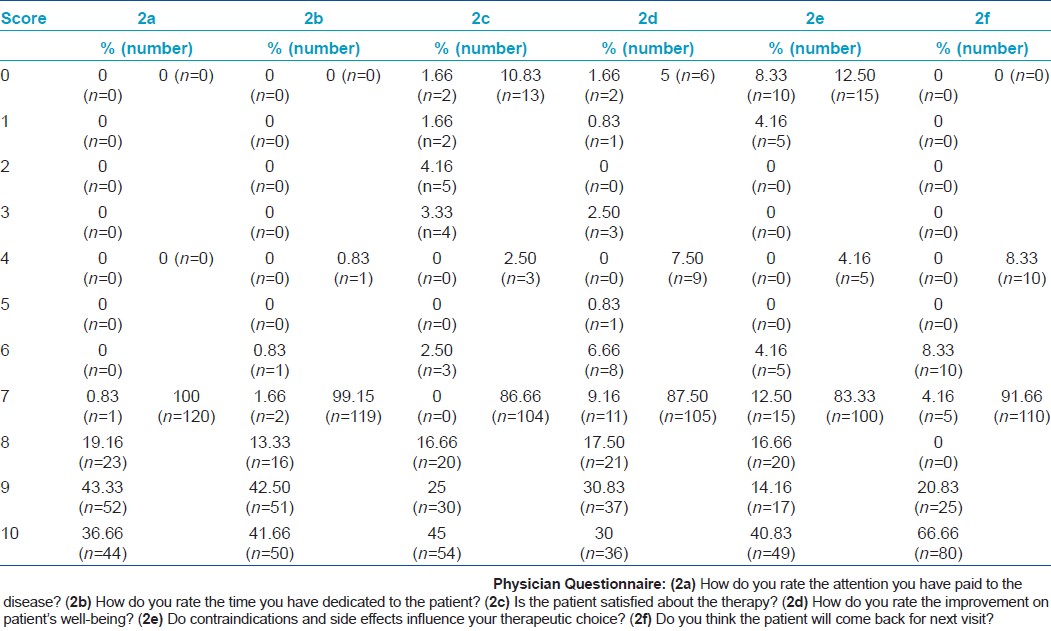
Psoriasis is a chronic skin disease that affects the quality of life for its esthetic, psychological and systemic implications. [1],[2] Only few studies have investigated how the disease and the patient-physician relationship are perceived by the patient or the dermatologist. [3],[4] We conducted a study to assess how psoriasis and its treatment are subjectively experienced by the patient and the dermatologist as well as to identify how to improve the doctor-patient relationship and to satisfy the patient′s expectations. In the present survey, a 10- item questionnaire using a 0-10 scale (score 0-3: negative; 4-6: not bad not good; 7-10: positive) was administered to 120 (56 males and 64 females; aged 18-70 years; mean 44.2 years) consecutive outpatients referred to our department of Dermatology from October 2009 to September 2010. All patients were receiving systemic treatments for psoriasis. Informed consent was obtained prior to interview. For each patient, a 10-item complementary questionnaire using a 0-10 scale was filled always by the same dermatologist. Patients completed their questionnaire anonymously after the medical examination such that their answers could not be influenced by the physicians in any way. Data were compared statistically by Student′s t and Pearson correlation tests. Ninety-eight patients (81.66%) rated the attention paid by the dermatologist regarding their disease as favorable (score=7-10) [Figure - 1]a; [Table - 1]a. Almost the same outcomes were reported for the evaluation of the time spent by the dermatologist for the medical examination [Figure - 1]b; [Table - 1]b. Interestingly, 77.50% (n=93) of the patients were satisfied with the treatment they received (score=7-10) [Figure - 1]c; [Table - 1]c, while 69.16% (n=83; score = 7-10) reported high well-being after treatments [Figure - 1]d; [Table - 1]d. 45.81% of the patients (n=55; score=0-3) reported that side-effects did not represent a significant obstacle to continue the systemic therapies [Figure - 1]e; [Table - 1]e; 106 patients (88.33%) related they will continue to consult the same dermatologists (score=7-10) [Figure - 1]f; [Table - 1]f. We found a statistically significant negative correlation between Psoriasis Area Severity Index (PASI) and the score of items regarding treatments (Are you satisfied about treatments you are doing for psoriasis?) (P=0.0003; [Figure - 2]a) and evaluation of well-being after treatments (How do you rate your well-being after treatment?) (P=0.0001; [Figure - 2]b), indicating that the persistence of psoriatic skin manifestations instead of treatments could deeply influence the patient attitude toward the disease. As regards the 10-item questionnaire filled by the physician, in all the cases (100%; n=120), the dermatologist considered more than sufficient the attention paid to the disease (score = 7-10) [Table - 2]a, and in 99.15% (n=119) of the cases more than sufficient the time dedicated to the patient (score = 7-10) [Table - 2]b. Following the dermatologist′s answers, 10.83% (n=13) of the patients were absolutely not satisfied about the therapy they were undergoing (score = 0-3) [Table - 2]c, while in 5% (n=6) of the cases the physician rated very insufficient the improvement on patient′s well-being (score=0-3) [Table - 2]d. Moreover, the dermatologist reported that the therapeutic choice was influenced by side-effects in 100 cases (83.33%; score=7-10) [Table - 2]e and that 110 patients (91.66%; score=7-10) will continue the follow-up [Table - 2]f. Attractive outcomes were produced by comparing physicians and patients answers among the same themes: attention paid to the disease/patient (mean patients=8,494 ± 0,1654, n=120; mean physician=9,158 ± 0,06900, n=120), time spent for the medical examination (mean patients=7,892 ± 0,1863, n=120; mean physician=9,217 ± 0,07313, n=120) and improvement on well-being after treatment (mean patients=7,400 ± 0,2353, n=120; mean physician=8,350 ± 0,1722, n=120) were overestimated by physicians in a statistically significant way (P=0.0001, P=0.0001 and P=0.0007, respectively). Difference in perception regarding satisfaction about the therapy (mean patients = 8,219 ± 0,1821, n=120; mean physician = 8,433 ± 0,2279, n=120) was not significant. This comparation seems to underline the most common factors altering the doctor-patient relationship, forming the basis of patient′s dissatisfaction and "doctor-shopping." Patient′s perspective is important not only in terms of symptoms but also on the well-being impact. In fact, it is known that the importance of patient expectations as it is expressed by "patient-centered medicine" sets a strong focus on patient participation in clinical decision making. [5] Consequently, clinician′s role also includes finding out patient expectations in order to help them to get the right information and supporting them in the decision-making process. The current study might therefore provide an indication on how to direct future qualitative research in order to improve psychological and relational aspects in the management of psoriasis.
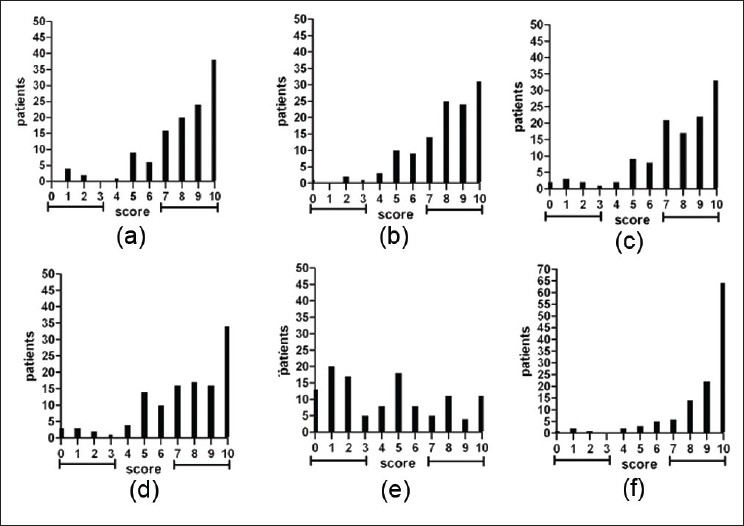 |
| Figure 1: Patient questionnaire: (a) How do you rate the attention paid by the doctor to your disease? (b) How do you rate the time spent by the doctor with you? (c) Are you satisfied about treatments you are doing for psoriasis? (d) How do you rate your well-being after treatment? (e) Do side effects represent an obstacle to continue the therapy? (f) Do you think you will consult the same physician? |
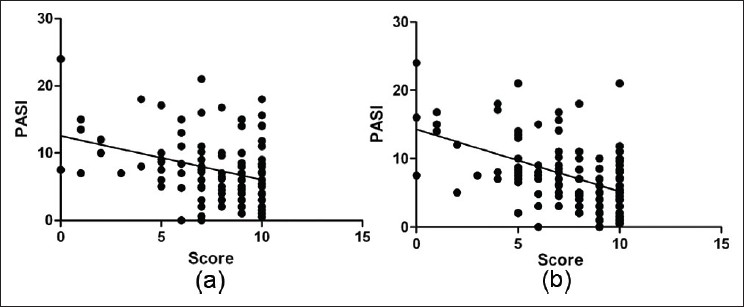 |
| Figure 2: Correlation between Psoriasis Area Severity Index (PASI) and patient's answers: (a) Correlation between PASI and patient's answers to question no. 3 (Do you consider treatments you are doing are good enough for the severity of your disease?) (P=0.0003) (b) Correlation between PASI and patient's answers to question no. 7 (How do you rate your well-being after treatment?) (P=0.0001) |
| 1. |
Hong J, Koo B, Koo J. The psychosocial and occupational impact of chronic skin disease. Dermatol Ther 2008;21:54-9.
[Google Scholar]
|
| 2. |
Sampogna F, Tabolli S, Mastroeni S, Di Pietro C, Fortes C, Abeni D. Quality of life impairment and psychological distress in elderly patients with psoriasis. Dermatology 2007;215:341-7.
[Google Scholar]
|
| 3. |
Linder D, Dall'olio E, Gisondi P, Berardesca E, De Gennaro E, Pennella AR, et al. Perception of disease and doctor-patient relationship experienced by patients with psoriasis. Am J Clin Dermatol 2009;10:325-30.
et al. Perception of disease and doctor-patient relationship experienced by patients with psoriasis. Am J Clin Dermatol 2009;10:325-30.'>[Google Scholar]
|
| 4. |
Tan J, Stacey D, Barankin B, Bissonnette R, Gulliver W, Lui H, et al. Support needed to involve psoriasis patients in treatment decisions: survey of dermatologists. J Cutan Med Surg 2011;15:192-200.
[Google Scholar]
|
| 5. |
Krahn M, Naglie G. The next step in guideline development: incorporating patient preferences. JAMA 2008;300:436-8.
[Google Scholar]
|
Fulltext Views
2,668
PDF downloads
3,351





