Translate this page into:
Patients with psoriasis have a higher risk of dementia: A systematic review and meta-analysis
Corresponding author: Dr. Nipith Charoenngam, 2 Prannok Road, Bangkoknoi, Bangkok 10700, Thailand. nipith.charoenngam@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Charoenngam N, Rittiphairoj T, Ponvilawan B, Ungprasert P. Patients with psoriasis have a higher risk of dementia: A systematic review and meta-analysis. Indian J Dermatol Venereol Leprol 2021;87:364-70.
Abstract
Background:
Patients with psoriasis may have a higher risk of dementia because of the higher inflammatory burden, although results from previous epidemiological studies have been inconsistent.
Aims:
To determine the association between psoriasis and risk of dementia by pooling the evidence from previous studies.
Methods:
Potentially eligible studies were identified from Medline and EMBASE databases from inception to July 2019 using a search that comprised terms for “psoriasis” and “dementia.” Studies were eligible for the meta-analysis if they were cohort studies that included psoriatic patients and individuals without psoriasis and followed them for incident dementia. Studies were also required to report standardized incidence ratio, hazard risk ratio or relative risk with related 95% confidence intervals (CI) comparing the incidence of dementia between the two cohorts. The retrieved point estimates with standard errors from each study were pooled into the final result by the random-effect model, generic inverse variance method.
Results:
A total of 8,861 articles were identified. After two rounds of independent review by three investigators, we included six cohort studies that met the eligibility criteria in the meta-analysis. The risk of dementia was significantly higher among psoriatic patients than in those without psoriasis with a pooled risk ratio of 1.16 (95% CI, 1.04–1.30; I2 95%). A funnel plot was relatively symmetric and was not suggestive of the presence of publication bias.
Limitations:
Limited accuracy of diagnosis of psoriasis and dementia as four included studies were coding-based studies, and high statistical heterogeneity among studies.
Conclusion:
This systematic review and meta-analysis indicates that psoriatic patients have a significantly elevated risk of developing dementia.
Keywords
Dementia
meta-analysis
psoriasis
Introduction
Dementia is characterized by a combination of behavioral, psychological and cognitive abnormalities, such as the loss of short-term memory, long-term memory and reasoning, and difficulty in communication, which affect the individual’s ability to perform daily activities.1 It is estimated that more than 46 million people around the world have been diagnosed with dementia and the incidence has been increasing.2 Known risk factors for dementia include increased age, limited physical activity, diabetes mellitus, obesity, hypertension, smoking and atherosclerotic cardiovascular disease.3,4 It has been reported that immune dysregulation and chronic inflammation might play a role in the pathogenesis of dementia.5,6 Patients with chronic inflammatory disorders may therefore have a higher tendency to develop dementia than the general population.
Psoriasis is a common chronic inflammatory skin disorder affecting around 2–3% of the world population.7 The etiology of psoriasis is unknown but is thought to be a combination of genetic predisposition and lifestyle factors, such as smoking, excessive alcohol intake and obesity.7 This immune-mediated disorder not only causes keratinocyte hyperproliferation resulting in cutaneous manifestations but is also associated with an increased risk of multiple comorbidities, such as the metabolic syndrome, atherosclerotic disease and inflammatory arthritis.7,8
Previous epidemiologic studies have indicated an increased incidence of dementia in psoriatic patients, but results have been inconsistent across studies.9-14 In order to further investigate this possible relationship, we conducted a systematic review and meta-analysis of studies that compared the risk of incident dementia in patients with psoriasis versus individuals without psoriasis.
Methods
Search strategy
Published studies indexed in Medline and Embase from inception to July 2019 were independently searched by 3 investigators (N.C., T.R., B.P.). Search terms derived from terms regarding psoriasis and dementia based on MeSH terms of the Medline database and EMTREE terms of EMBASE. All 3 investigators utilized the same set of search terms. The search strategy is demonstrated in the supplement 1. We applied no language limitation.
Inclusion criteria
To be eligible, a study had to be a cohort study that consisted of one cohort of patients with psoriasis and another cohort of individuals without psoriasis. The study must have followed them for incident dementia. Relative risk (RR), hazard risk ratio (HR), standardized incidence ratio (SIR), or incidence rate ratio (IRR) with associated 95% confidence interval (CI) comparing the incidence of dementia between the two cohorts must have been reported.
Three investigators (N.C., T.R., B.P.) independently reviewed study eligibility. Discussion with the senior investigator (P.U.) was used for the resolution of differing opinions. Two investigators (P.U. and B.P.) evaluated the quality of each study after the study was deemed eligible using the Newcastle–Ottawa quality assessment scale for cohort studies.15 Investigators were not blinded to the authors/ institutions of the studies being reviewed.
Data extraction
A standardized data collection form was applied for extraction of the following details: last name of the first author, country of the study, study design, publication year, number of participants, recruitment of participants, diagnosis of psoriasis, diagnosis of dementia, follow-up duration, mean age of participants, percentage of male participants, comorbidities of participants and variables that were adjusted in multivariate analysis. Individual patient level data was not obtained from each study to be used for the analysis.
Statistical analysis
We used Review Manager 5.3 software from the Cochrane Collaboration for analysis of data. Point estimates with standard errors were retrieved from each study and were combined together using the generic inverse variance method as described by DerSimonian and Laird.16 The random-effect model, instead of a fixed-effect model, was used as the studies included had different background populations and protocols.
The Cochran’s Q test was used to determine statistical heterogeneity. This is further adjuncted with the I2 statistic, which quantifies the proportion of the total variation across studies that is from heterogeneity rather than coincidence. A value of I2 of 0%–25% represents insignificant heterogeneity, 26%–50% low heterogeneity, 51%–75% moderate heterogeneity and >75% high heterogeneity.17
A funnel plot was used for investigating the presence of publication bias.
Results
Search results
A total of 8,861 articles were retrieved from EMBASE and MEDLINE databases. Three hundred seventy six duplicated articles were withdrawn, leaving 8,485 articles for title and abstract review. After independent review of title and abstract by the three investigators, 8,432 articles were also withdrawn as they did not meet the eligibility criteria for study design and type of article. This left a total of 53 articles for the full-length article review. Forty eight articles were further withdrawn because of the absence of the outcome of interest and five studies satisfied the eligibility criteria. We then reviewed the bibliography of these included studies9-13 and selected random review articles and identified one additional eligible study.14 All investigators made the same determination regarding the eligibility of each study. Finally, we included six cohort studies that met the eligibility criteria in the meta-analysis.9-14 Figure 1 demonstrates the search methodology and selection in this study. Table 1 demonstrates the summary of the characteristics and the Newcastle–Ottawa quality score of all included cohort studies in this study. All except one study included in the meta-analysis adjusted their results for several possible confounders, including demographic variables, comorbidities and socioeconomic status [ Table 1].9,11-14
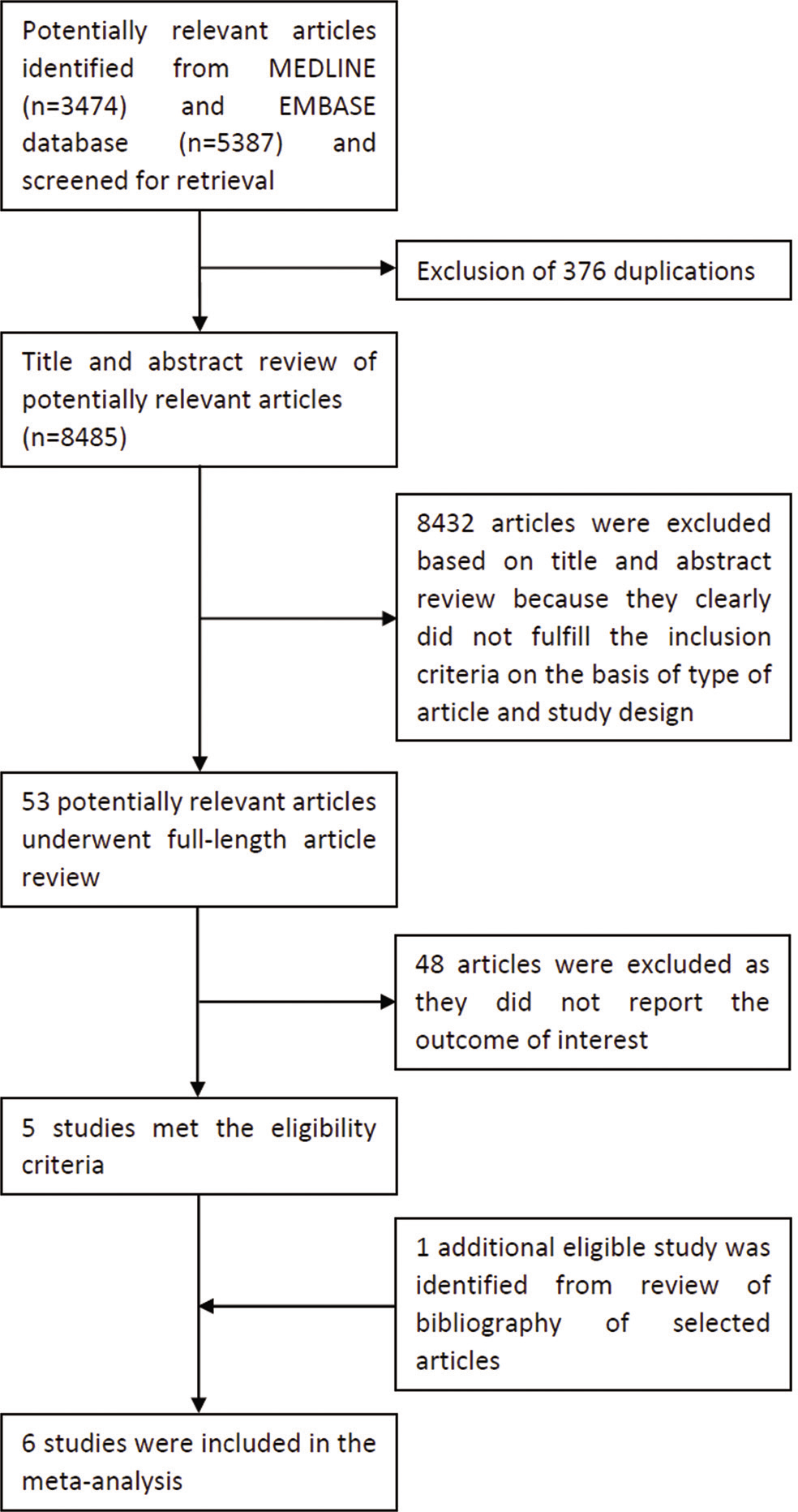
- Study identification and literature review process process
| Dregan et al. | Wotton et al. | Li et al. | |
|---|---|---|---|
| Country | United Kingdom | England | Sweden |
| Study design | Retrospective cohort | Retrospective cohort | Retrospective cohort |
| Year of publication | 2015 | 2017 | 2018 |
| Total number of participants | Patients with psoriasis: 91,789 Comparators: 308,843 |
Patients with psoriasis: N/A Comparators: around 7 million |
Patients with psoriasis: 108,607 Comparators: N/A |
| Recruitment of participants | Patients with psoriasis were identified from the database of CPRD between January 1st, 2002 and January 31st, 2013. CPRD included data of 14 million patients from 660 primary care practices across the United Kingdom. Comparators without psoriasis were randomly selected from the same database. Individuals with prior diagnosis of dementia before index date were excluded. |
Patients with psoriasis were identified from the English national HES database from April 1st, 1998 to March 31st, 2012. HES included data of all admission occurred in the National Health Service hospitals. Comparators without psoriasis were selected from the same database by identifying the first admission for each individual with various other medical and surgical conditions and injuries as the primary discharge diagnoses. |
Patients with psoriasis were identified from the database of SNPR between January 1st, 1964 and December 31st, 2010 without prior diagnosis of dementia. SNPR included data of both inpatient and outpatient care of virtually all Swedish citizens. General population was used as comparator to estimate expected number of dementia to calculate age, sex, region and socioeconomic status-specific standard incidence rates. |
| Diagnosis of psoriasis | Presence of diagnostic codes of psoriasis in the database (M16, excluding pityriasis rosea and related disorders) | Presence of diagnostic codes of psoriasis in the database (L40) | Presence of diagnostic codes of psoriasis in the database (ICD-7: 706; ICD-8:696; ICD-9: 696; ICD-10: L40) |
| Diagnosis of dementia | Presence of diagnostic codes of Alzheimer’s disease, vascular dementia, Lewy body dementia, frontotemporal dementia, dementia in other conditions and unspecified dementia in the database | Presence of diagnostic codes of dementia in the database (ICD-9: 290.4, 331.0; ICD-10: F00-F01, F03, G30) | Presence of diagnostic codes of dementia in the database (ICD-7: 304-306; ICD-8: 290, 293; ICD-9: 290,331; ICD-10: F00, F01, F03, G30) |
| Follow-up period | Until the development of dementia, death, end of CPRD record or January 31st, 2013 | Until development of dementia or death | Until the development of dementia, death, emigration out of the system or December 31st, 2010 |
| Follow-up duration (years) | Patients with psoriasis: 4.0 Comparators: N/A |
Patients with psoriasis: 4.3 Comparators: N/A |
Patients with psoriasis: N/A Comparators: N/A |
| Age of participants (years) | Patients with psoriasis: 46.1 Comparators: 50.0 |
Patients with psoriasis: 56.5 Comparators: N/A |
Patients with psoriasis: N/A Comparators: N/A |
| Sex (male) | Patients with psoriasis: 48.0% Comparators: 44.0% |
Patients with psoriasis: 55.3% Comparators: N/A |
Patients with psoriasis: N/A Comparators: N/A |
| Comorbidities | Patients with psoriasis: Obesity 26.3% Depression 19.1% Current smoker 31.9% Current alcohol 81.9% Glucocorticoids 13.6% CHD 6.0% Stroke 1.0% Type 2 diabetes 6.1% Comparators: Obesity 23.0% Depression 14.0% Current smoker 24.0% Current alcohol 80.0% Glucocorticoids 11.0% CHD 8.0% Stroke 2.0% Type 2 diabetes 9.0% |
Patients with psoriasis: N/A Comparators: N/A |
Patients with psoriasis: N/A Comparators: N/A |
| Variables adjusted in multivariate analysis | Age, age squared, sex, BMI, depression, smoking, alcohol, serum creatinine levels, exercise, antihypertensives, statins, coronary heart disease, stroke, type 2 diabetes, baseline glucocorticoids and NSAID and follow-up therapy with glucocorticoids and/or NSAIDs. | Sex, age in 5-year bands, time period in single calendar years, region of residence and deprivation score associated with patients’ area of residence, in quintiles | Age, sex, socioeconomic status and region of residence |
| Newcastle-Ottawa score | Selection: 4 Comparability: 2 Outcome: 3 |
Selection: 3 Comparability: 2 Outcome: 3 |
Selection: 3 Comparability: 1 Outcome: 3 |
| Country | The Netherlands | Taiwan | South Korea |
| Study design | Prospective cohort | Retrospective cohort | Retrospective cohort |
| Year of publication | 2018 | 2019 | 2019 |
| Total number of participants | Patients with psoriasis: 311 Comparators: 9305 |
Patients with psoriasis: 3,820 Comparators: 15,280 |
Patients with psoriasis: 535,927 Comparators: 2,679,635 |
| Recruitment of participants | Patients with psoriasis were identified from the database of the Rotterdam Study that included all inhabitants of a suburb of Rotterdam aged > 55 years since 1990. Comparators without psoriasis were randomly selected from the same database. Individuals with prior diagnosis of dementia before index date were excluded. |
Patients with psoriasis were identified from T-NHIRD between January 1st, 1996 and December 31st, 2013. T-NHIRD included data of over 99% of all residents in Taiwan. Comparators without psoriasis were randomly selected from the same database. Comparators were sex, age, urbanization and index date-matched to cases. Individuals with prior diagnosis of dementia before index date were excluded. |
Patients with psoriasis were identified from Korean National Health Insurance System database between 2008 and 2014. Comparators without psoriasis were randomly selected from the same database. Comparators were sex and age-matched to cases. |
| Diagnosis of psoriasis | Presence of at least one of the following: 1) Diagnosis of psoriasis in medical records (at least once by dermatologists or rheumatologists or at least twice by general practitioners) 2) At least one prescription for psoriasis-specific medication (psoralens, dithranol, calcipotriol, calcitriol, coal tar, tacrolimus, pimecrolimus, fumaric acid, acitretin, methotrexate, cyclosporine or biologic agents) 3) Psoriatic rash present when the patient was seen by research physicians. |
Presence of diagnostic codes of psoriasis in the database for at least 1 time in inpatient setting or 3 times in outpatient setting (ICD-9-CM codes: 696.0, 696.1, 696.8) | N/A |
| Diagnosis of dementia | Diagnosis was made based on standard criteria for dementia and AD with neuropsychological examination by research neurologists. | Presence of diagnostic codes of dementia in the database for at least 1 time in inpatient setting or 3 times in outpatient setting (ICD-9-CM codes: 290.0-290.4, 294.1-294.2, 331.0-331.2, 331.82) | N/A |
| Follow-up period | Until the development of dementia, death, lost to follow-up or January 1st, 2015. | Until the development of dementia, resignation from the registry or December 31st, 2013. | N/A |
| Follow-up duration (years) | Patients with psoriasis: N/A Comparators: N/A |
Patients with psoriasis: 7.3 Comparators: 7.2 |
Patients with psoriasis: N/A Comparators: N/A |
| Age of participants (years) | Patients with psoriasis: 66.8 Comparators: 66.1 |
Patients with psoriasis: N/A Comparators: N/A |
Patients with psoriasis: N/A Comparators: N/A |
| Sex (male) | Patients with psoriasis: 44.4% Comparators: 41.7% |
Patients with psoriasis: 63.6% Comparators: 63.6% |
Patients with psoriasis: N/A Comparators: N/A |
| Comorbidities | Patients with psoriasis: History of smoking 72.9% Hypertension 58.2% Diabetes 16.0% Comparators: History of smoking 68.7% Hypertension 52.4% Diabetes 12.9% |
Patients with psoriasis: Hypertension 58.0% Heart disease 43.9% Diabetes 33.1% Hyperlipidemia 44.6% Stroke 22.2% Depression 12.0% Comparators: Hypertension 51.4% Heart disease 38.1% Diabetes 27.1% Hyperlipidemia 36.9% Stroke 19.5% Depression 9.5% |
Patients with psoriasis: N/A Comparators: N/A |
| Variables adjusted in multivariate analysis | Age, sex, education, BMI, waist circumference, diabetes, hypertension, total cholesterol and smoking | Age, sex, level of urbanization of residence, hypertension, heart disease, diabetes, hyperlipidemia, stroke and depression | N/A |
| Newcastle-Ottawa score | Selection: 4 Comparability: 2 Outcome: 3 |
Selection: 4 Comparability: 2 Outcome: 3 |
Selection: 3 Comparability: 1 Outcome: 1 |
Abbreviation: AD: Alzheimer’s disease; BMI: body mass index; CHD: coronary heart disease; COPD: chronic obstructive pulmonary disease; CPRD: Clinical Practice Research Datalink; HES: Hospital Episode Statistics; ICD-7: International Classification of Disease, Seventh Revision; ICD-8: International Classification of Disease, Eighth Revision; ICD-9: International Classification of Disease, Ninth Revision; ICD-10: International Classification of Disease, Tenth Revision; NSAID: non-steroidal anti-inflammatory drug; SNPR: Swedish National Patient Register; T-NHIRD: Taiwan’s National Health Insurance Research database
Risk of incident dementia in psoriatic patients
The meta-analysis demonstrated an elevated risk of incident dementia in psoriatic patients compared to those without psoriasis with the pooled risk ratio of 1.16 (95% CI, 1.04–1.30). This meta-analysis had high statistical heterogeneity with I2 of 95 % [Figure 2].
Sensitivity analysis
Two studies12,13 utilized national databases from the United Kingdom during overlapping calendar years (Dregan et al.: 2002 – 2013; Wotton et al. 1998 – 2012). This might have caused duplication of participants included. In order to resolve this, we performed a sensitivity analysis by excluding one of those two aforementioned studies. The pooled results were not significantly changed after excluding either of those two studies. The new pooled RR were 1.13 (95% CI, 1.03–1.24; I2 72%) and 1.16 (95% CI, 1.04–1.30; I296%) after excluding the study by Wotton and Goldacre12 and the one by Dregan et al., respectively.13
Evaluation for publication bias
We used a funnel plot [Figure 3] to assess the publication bias of this meta-analysis. The funnel plot was fairly symmetric and did not demonstrate evidence of publication bias in favor of studies that showed a positive association.
Discussion
This is the first systematic review and meta-analysis of cohort studies that have looked at the relationship between psoriasis and risk of dementia. The pooled analysis showed that psoriatic patients have a 16% elevated risk of developing dementia compared to normal subjects after the average duration of follow-up that ranged from 4.0 to 7.3 years. This observation may have clinical implications as it may suggest that psoriasis could be another risk factor for dementia. Therefore, patients with psoriasis should be carefully monitored for their cognitive function and may need to be further assessed for dementia if they show any sign of cognitive decline.
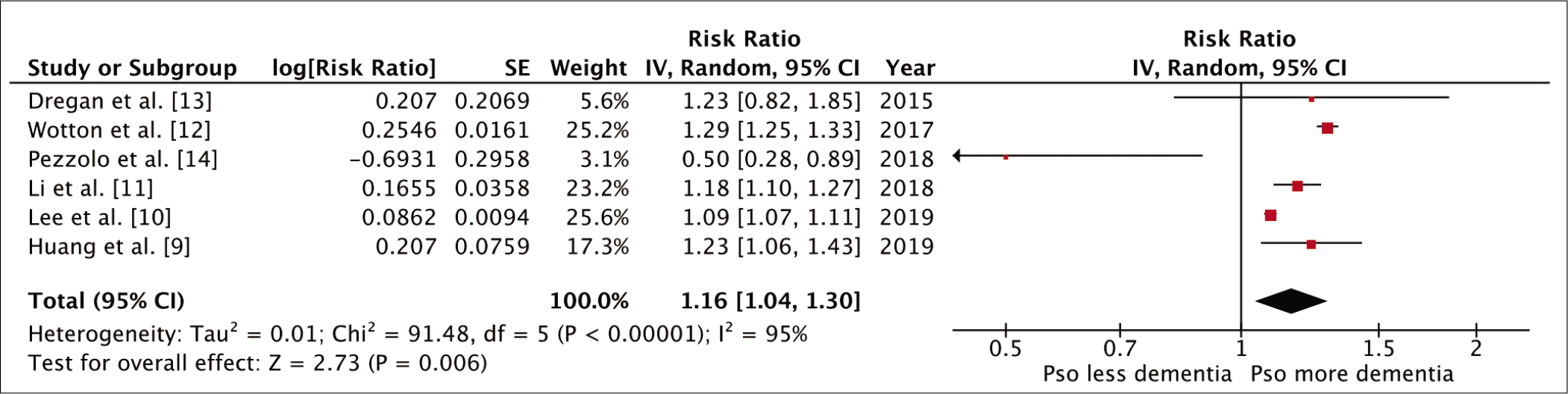
- Forest plot of the meta-analysis of risk of dementia in patients with psoriasis
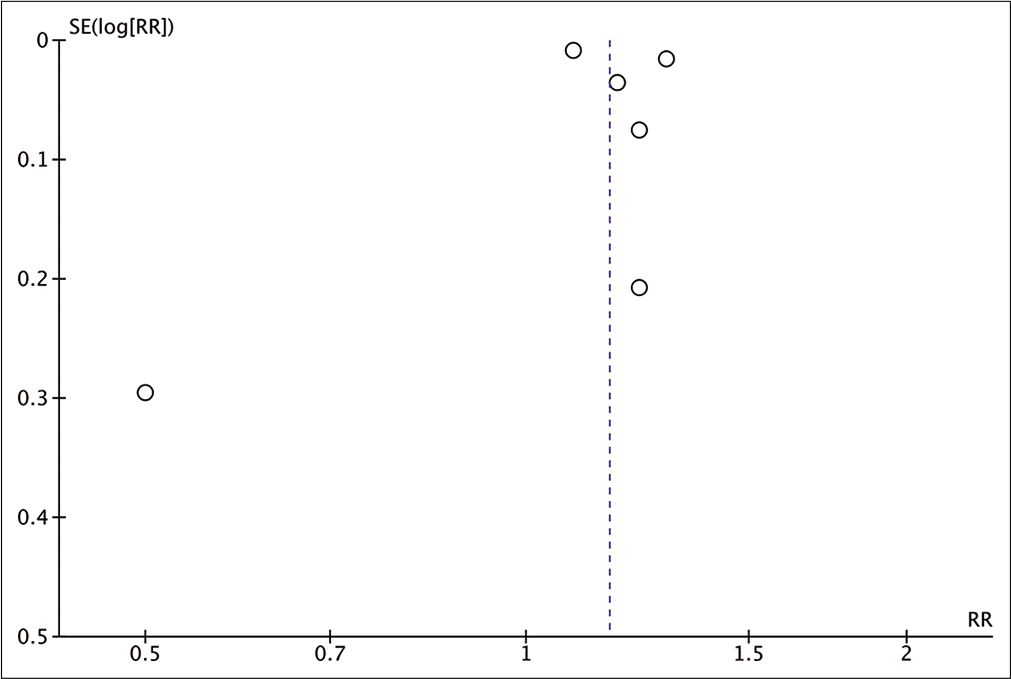
- Funnel plot of the meta-analysis of risk of dementia in patients with psoriasis
There are no known mechanisms that could conclusively explain the result of our meta-analysis. A possible mechanism for the relationship between psoriasis and dementia is that the presence of chronic inflammation can cause cognitive impairment.5,6 Population-based studies have reported that increased levels of inflammatory mediators, such as interleukin-6, TNF-α and C-reactive protein are associated with a higher risk of dementia.5,6 These cytokines are also known markers of disease activity in psoriasis. How these psoriasis-associated inflammatory cytokines might affect cognitive function and neurogenesis is also unclear, but one possible link is that they may suppress production and function of plasma brain-derived neurotrophic factor (BDNF), which has been demonstrated to play a role in preventing age-related decreased neurogenesis and cognitive dysfunction.18,19 This hypothesis could be further supported by the observations from Brunoni et al. who found lower plasma BDNF levels in patients with psoriasis than in healthy controls.20 In addition, they also found that plasma BDNF level increased after those patients were treated with psoriasis-specific therapy.20 Similarly, another study found that psoriatic patients who received more than 90 days of systemic therapy to reduce inflammatory burden (disease-modifying antirheumatic drugs and/or TNF antagonists and/or phototherapy) had about 25% lower risk of dementia than those who did not receive systemic therapy after a follow-up duration of approximately 7 years.9
Another possible explanation is that psoriasis and dementia may have some common genetic bases because hereditary components have been shown to play a strong role in both diseases21,22. There is increasing evidence showing that ApoEε4 allele is not only associated with an increased risk for Alzheimer’s disease with earlier age of disease onset,21 but also the risk of guttate psoriasis and chronic plaque psoriasis.22 It is also possible that the observed association is due to a confounding effect of several common predisposing factors that both psoriasis and dementia share, such as smoking, obesity and the metabolic syndrome.3,4,7,8
Limitations
This study has some limitations and the pooled results presented should be carefully interpreted. First, four of the six included studies relied on diagnostic codes from large administrative databases to identify psoriasis and dementia. Thus, some limitations in the accuracy of the diagnoses of both diseases might be present. In addition, none of the included studies provided information on specific subtypes of psoriasis. Further studies should be conducted to address this question. Second, there was high statistical heterogeneity in this meta-analysis, which was likely to be the result of the difference in characteristics of the studied populations and study methodologies. In fact, the prospective cohort study by Pezzolo et al.14 reported a significantl decreased risk of dementia in patients with psoriasis with the adjusted hazard ratio of 0.50 (95% CI: 0.28-0.91), whereas all other included studies reported the opposite.9-13 The inverse relationship between psoriasis and dementia reported by Pezzolo et al. is likely due to the higher use of antihypertensive therapy (e.g. approximately 70% in Pezzelo et al.’s study compared with 55 % in Huang et al.’s study) and disease-modifying antirheumatic drugs, which have been suggested to be protective against dementia.23,24 Further studies should be conducted to find the explanation of the discrepancy in the results. Finally, although publication bias was not suggested by the funnel plot, the small number of included studies might make the plot unreliable. Therefore, unpublished data may have been present and have been missed by our systematic review.
Conclusion
The current systematic review and meta-analysis found a significantly increased risk of developing dementia among patients with psoriasis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Supplementary material available online:
References
- Dementia: Assessment, management and support: Summary of updated NICE guidance. BMJ. 2018;361:k2438.
- [CrossRef] [PubMed] [Google Scholar]
- A clinicopathological approach to the diagnosis of dementia. Nat Rev Neurol. 2017;13:457-76.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and risk factors of dementia. J Neurol Neurosurg Psychiatr. 2005;76(Suppl 5):v2.
- [CrossRef] [PubMed] [Google Scholar]
- The role of peripheral inflammatory markers in dementia and Alzheimer's disease: A meta-analysis. J Gerontol A Biol Sci Med Sci. 2013;68:433-40.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory markers and the risk of Alzheimer disease: The Framingham Study. Neurology. 2007;68:1902-8.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis: Epidemiology, clinical features, comorbidities, and clinical scoring. Indian Dermatol Online J. 2016;7:471-80.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis: Classical and emerging comorbidities. An Bras Dermatol. 2015;90:9-20.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of dementia among individuals with psoriasis: A nationwide population-based cohort study in Taiwan. J Clin Psychiatry. 2019;80
- [CrossRef] [Google Scholar]
- Alzheimer's disease risk in patients with psoriasis: A nationwide population-based cohort study. J Eur Acad Dermatol Venereol. 2019;33:22.
- [CrossRef] [PubMed] [Google Scholar]
- Dementia and Alzheimer's disease risks in patients with autoimmune disorders. Geriatr Gerontol Int. 2018;18:1350-5.
- [CrossRef] [PubMed] [Google Scholar]
- Associations between specific autoimmune diseases and subsequent dementia: Retrospective record-linkage cohort study, UK. J Epidemiol Community Health. 2017;71:576-83.
- [CrossRef] [PubMed] [Google Scholar]
- Are inflammation and related therapy associated with all-cause dementia in a primary care population? J Alzheimers Dis. 2015;46:1039-47.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis is not associated with cognition, brain imaging markers and risk of dementia: The rotterdam study. J Am Acad Dermatol 2018
- [CrossRef] [PubMed] [Google Scholar]
- The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis.
- [Google Scholar]
- Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60.
- [CrossRef] [PubMed] [Google Scholar]
- Brain-derived neurotrophic factor: A bridge between inflammation and neuroplasticity. Front Cell Neurosci. 2014;8:430.
- [CrossRef] [PubMed] [Google Scholar]
- Aberrant hippocampal neurogenesis after limbic kindling: Relationship to BDNF and hippocampal-dependent memory. Epilepsy Behav. 2015;47:83-92.
- [CrossRef] [PubMed] [Google Scholar]
- Decreased brain-derived neurotrophic factor plasma levels in psoriasis patients. Braz J Med Biol Res. 2015;48:711-4.
- [CrossRef] [PubMed] [Google Scholar]
- Apolipoprotein E and Alzheimer disease: Risk, mechanisms and therapy. Nat Rev Neurol. 2013;9:106-18.
- [CrossRef] [PubMed] [Google Scholar]
- Apolipoprotein E gene polymorphisms are associated with psoriasis but do not determine disease response to acitretin. Br J Dermatol. 2006;154:345-52.
- [CrossRef] [PubMed] [Google Scholar]
- Antihypertensive drugs and incidence of dementia: The rotterdam study. Neurobiol Aging. 2001;22:407-12.
- [CrossRef] [Google Scholar]
- Protective effect of antirheumatic drugs on dementia in rheumatoid arthritis patients. Alzheimers Dement (N Y). 2017;3:612-21.
- [CrossRef] [PubMed] [Google Scholar]






