Translate this page into:
Pemphigus vegetans arising in umbilicus: Successful clearance with intralesional steroid
2 Department of Pathology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
3 Department of Microbiology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
Correspondence Address:
Aylin Türel Ermertcan
Department of Dermatology, Faculty of Medicine, Celal Bayar University, Manisa 45010
Turkey
| How to cite this article: Cetinarslan TS, Ermertcan AT, Temiz P, Kurutepe S. Pemphigus vegetans arising in umbilicus: Successful clearance with intralesional steroid. Indian J Dermatol Venereol Leprol 2018;84:522 |
Sir,
Pemphigus vegetans is a rare clinical variant of pemphigus vulgaris accounting for 1%–2% of all pemphigus.[1],[2] All subtypes of pemphigus are known to affect all clinical sites, but there is a definite predilection for the oral mucosa and intertriginous areas.[1] Though the etiopathogenesis of pemphigus vegetans is not entirely clear, vegetating lesions often localize to intertriginous areas attributed to the occlusion and maceration in these areas with secondary bacterial infection.[1],[2],[3] On literature search, we found only one case report of a patient treated with systemic immunosuppressants having pemphigus vegetans lesions located on umbilicus.[4] We report here a case of pemphigus vegetans originating on the umbilicus treated successfully with intralesional steroids.
A 74-year-old man presented to our outpatient clinic with a 2 months history of asymptomatic nodules in the right inguinal region and around the umbilicus. The lesions had first begun on the umbilicus followed by similar lesions on the right groin. These had not responded to oral and topical antibiotics. On dermatological examination, nodular vegetating lesions of size 1 to 4 cm were seen over umbilicus and right inguinal region [Figure - 1]. There were no mucosal lesions. A skin biopsy was performed with differential diagnoses of dermatofibrosarcoma protuberans, pemphigus vegetans and cutaneous metastasis from gastrointestinal adenocarcinoma. On histopathological examination, there was marked acanthosis with pseudoepitheliomatous hyperplasia of the epidermis with underlying dermis showing mixed inflammatory cell infiltrate with predominance of eosinophils, edema and proliferation of capillaries. Acantholytic keratinocytes were detected in the basal epidermis. [Figure - 2] Intercellular immunoglobulin G and C3 deposits were observed on direct immunofluorescent examination [Figure - 3]. Based on clinical, histopathological and immunofluorescence findings, a diagnosis of pemphigus vegetans was established.
 |
| Figure 1 |
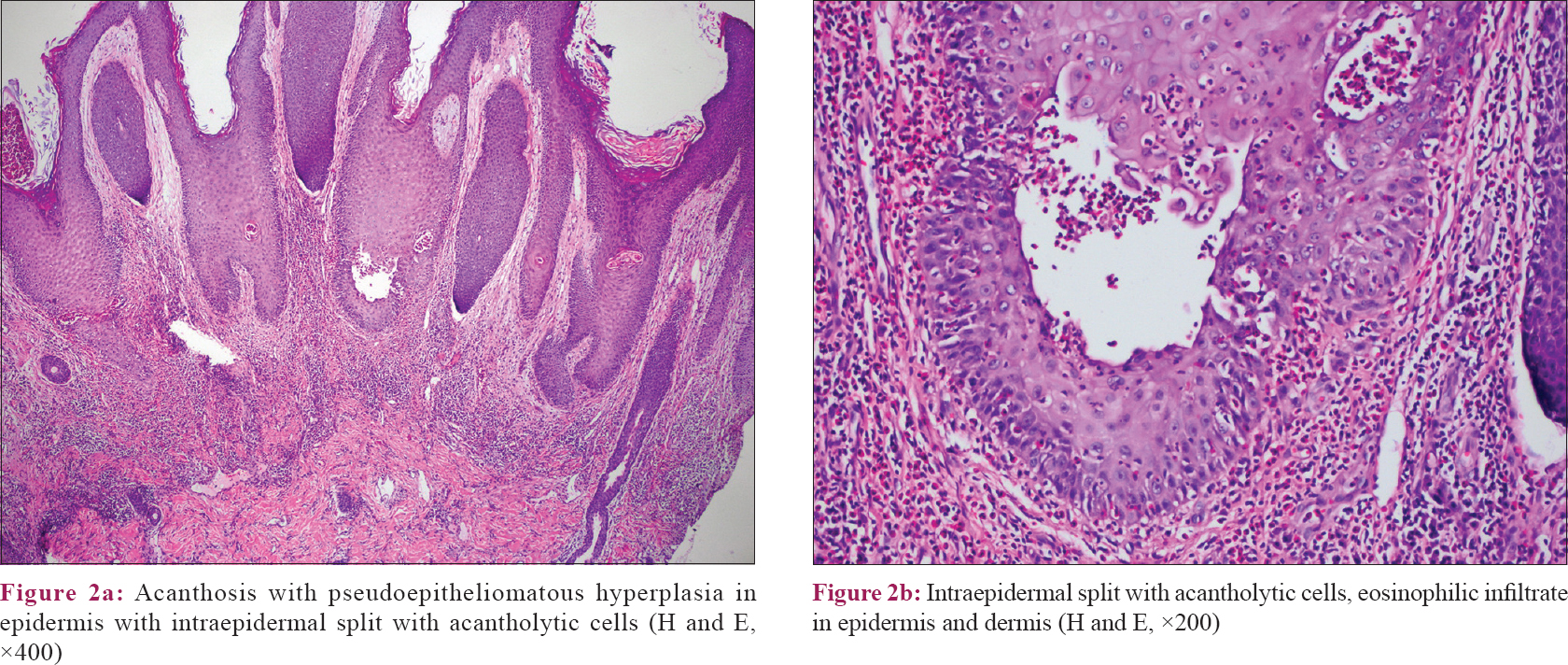 |
| Figure 2 |
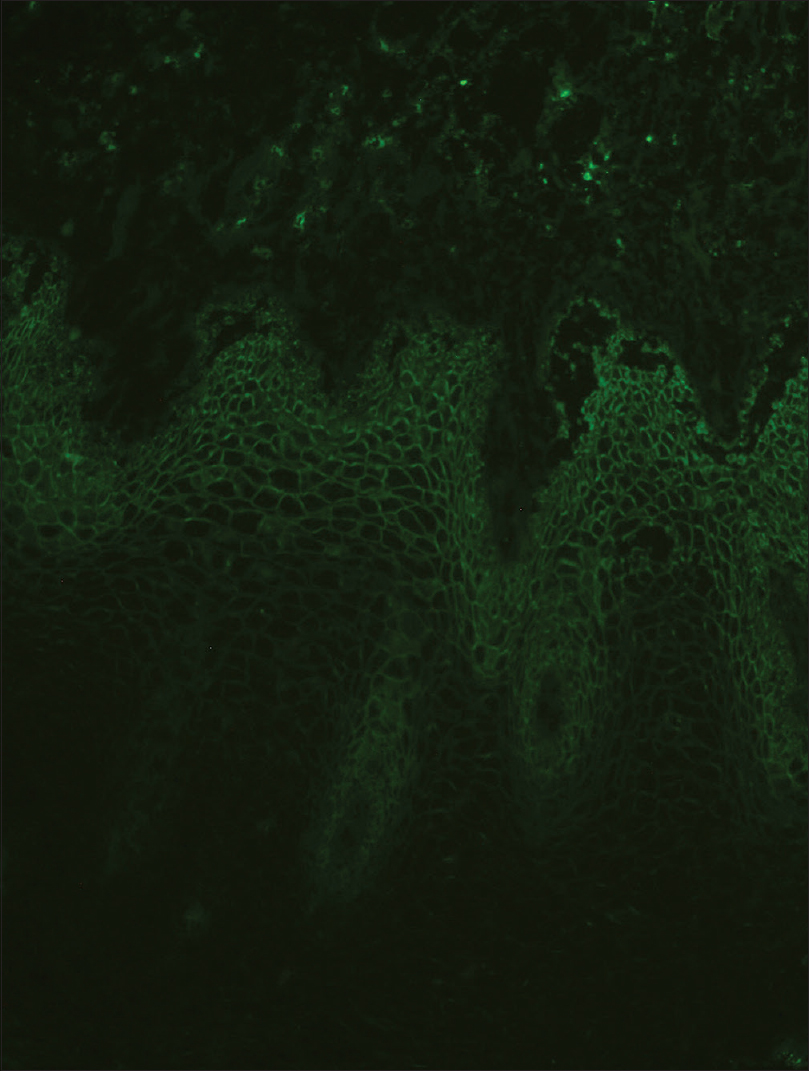 |
| Figure 3: Intercellular immunoglobulin G deposition in epidermis, direct immunofluorescence examination (×100) |
On laboratory investigations, he had mild anemia and high erythrocyte sedimentation rate. Tumor markers were negative. Mycological direct examination and cultures were negative. On bacteriological culture performed from umbilicus, Streptococcus agalactiae growth was observed.
Daily dressings with rivanol 0.1% solution and systemic amoxicillin-clavulanic acid (1000 mg orally twice daily) were started for the patient. After completing a 10-day antibiotic course, the patient was started on intralesional steroid injections. We applied intralesional 40 mg triamcinolone acetonide, diluted with 3 ml of saline (10 mg/ml), once in 2 weeks for 4 sessions. Lesions healed completely with postinflammatory hyperpigmentation in 2 months and there was no recurrence on 9 month follow up [Figure - 4].
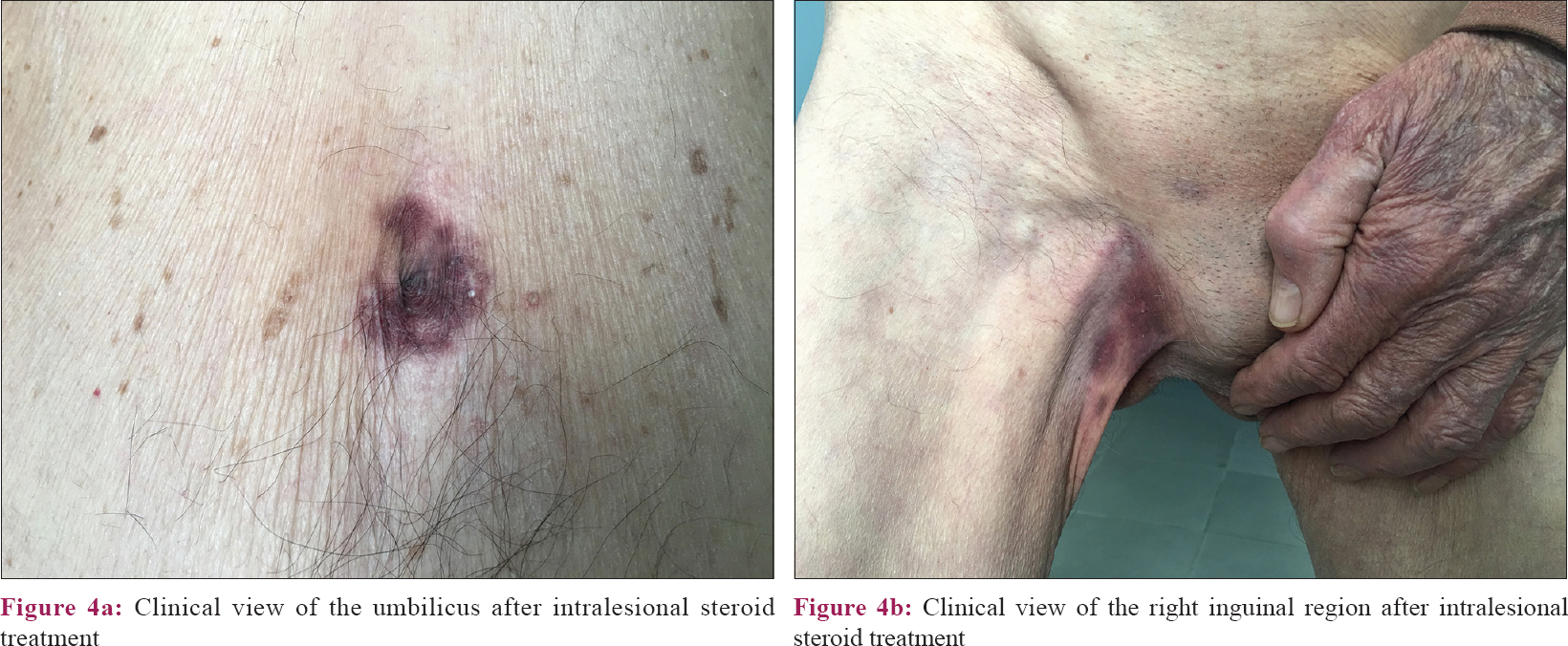 |
| Figure 4 |
Treatment of pemphigus vegetans is quite similar to that for pemphigus vulgaris and often requires systemic steroids and/or other immunosuppressants like azathioprine, mycophenolate mofetil, or cyclosporine. However, for the treatment of localized disease, intralesional steroids may be preferred.[5],[6] In our case, we achieved successful response using just intralesional steroid therapy.
In patients with limited lesions of pemphigus vegetans without mucosal involvement, intralesional steroid may be used as the first-line therapy to avoid the adverse effects of systemic steroids. These patients, however, need to be followed closely for recurrence as intralesional steroids are unlikely to cure the disease. In case recurrence is observed, systemic treatment may be administered at a later date.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Zaraa I, Sellami A, Bouguerra C, Sellami MK, Chelly I, Zitouna M, et al. Pemphigus vegetans: A clinical, histological, immunopathological and prognostic study. J Eur Acad Dermatol Venereol 2011;25:1160-7.
[Google Scholar]
|
| 2. |
Ruocco V, Ruocco E, Caccavale S, Gambardella A, Lo Schiavo A. Pemphigus vegetans of the folds (intertriginous areas). Clin Dermatol 2015;33:471-6.
[Google Scholar]
|
| 3. |
Ma DL, Fang K. Hallopeau type of pemphigus vegetans confined to the right foot: Case report. Chin Med J (Engl) 2009;122:588-90.
[Google Scholar]
|
| 4. |
Meziane M, Mernissi FZ. Pemphigus vegetans: A rare dermatosis of the folds. Pan Afr Med J 2013;15:134.
[Google Scholar]
|
| 5. |
Ichimiya M, Yamamoto K, Muto M. Successful treatment of pemphigus vegetans by addition of etretinate to systemic steroids. Clin Exp Dermatol 1998;23:178-80.
[Google Scholar]
|
| 6. |
Son YM, Kang HK, Yun JH, Roh JY, Lee JR. The neumann type of pemphigus vegetans treated with combination of dapsone and steroid. Ann Dermatol 2011;23 Suppl 3:S310-3.
[Google Scholar]
|
Fulltext Views
2,810
PDF downloads
2,180





