Translate this page into:
Pemphigus vulgaris associated with surgery: A rare association
Correspondence Address:
Ping Fu
Department of Dermatology, The Second Affiliated Hospital of Kunming Medical University, No. 374, Burma road, Kunming 650101, Yunnan province
China
| How to cite this article: Rashid A, Wang J, Fu P, Wang W, Xie H. Pemphigus vulgaris associated with surgery: A rare association. Indian J Dermatol Venereol Leprol 2015;81:299-301 |
Sir,
A 63-year-old Chinese woman was admitted with blisters and erosions with scabbing, involving the trunk, limbs and the scalp for 1 year. A few blisters initially appeared around a surgical incision, 2 weeks following an appendectomy. It was associated with pain and pruritus. The blisters were flaccid, and ruptured easily to form erosions and scabs. The lesions then began to appear all over the body over the next six months involving the trunk, limbs and scalp. She was diagnosed to have a skin infection and treated with debridement of the surgical wound along with systemic and topical antibiotics at a local hospital. The lesions did not resolve, after which she consulted at our hospital.
Cutaneous examination revealed flaccid vesicles and bullae containing clear liquid, along with crusts. They were distributed over the trunk, extremities, and around the appendectomy scar in the right iliac fossa. The face, mucous membranes, and perineum were not involved. Nikolsky sign was positive [Figure - 1]a and b. Systemic examination was within normal limits. There was no history of oral ulcers, drug allergy, or a family history of skin diseases.
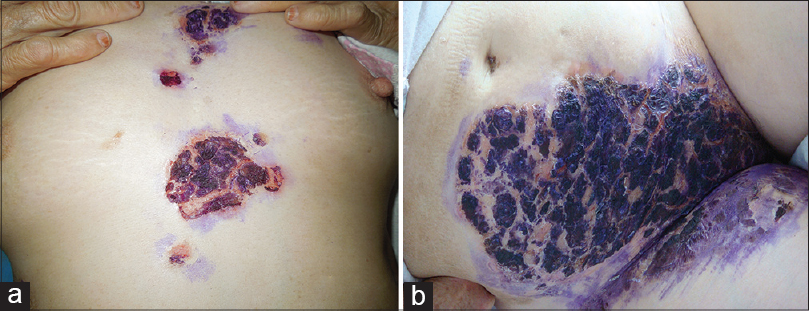 |
| Figure 1: (a) Erosions with crusts over the chest at the time of admission. (b) Erosions with crusts distributed around the appendectomy scar over the right iliac fossa after one week |
Laboratory investigations were within normal limits and the culture of blister fluid was negative. Desmoglein 1 levels were 102.83 U/ml (normal value <14 U/ml) and desmoglein 3 was 183.27 U/ml (normal value <7 U/ml). Histopathological examination revealed acantholysis localized to the suprabasal layer along with Tzanck cells [Figure - 2]. Direct immunofluorescence revealed intercellular deposits of IgG and C3 in the epidermis [Figure - 3]a and b.
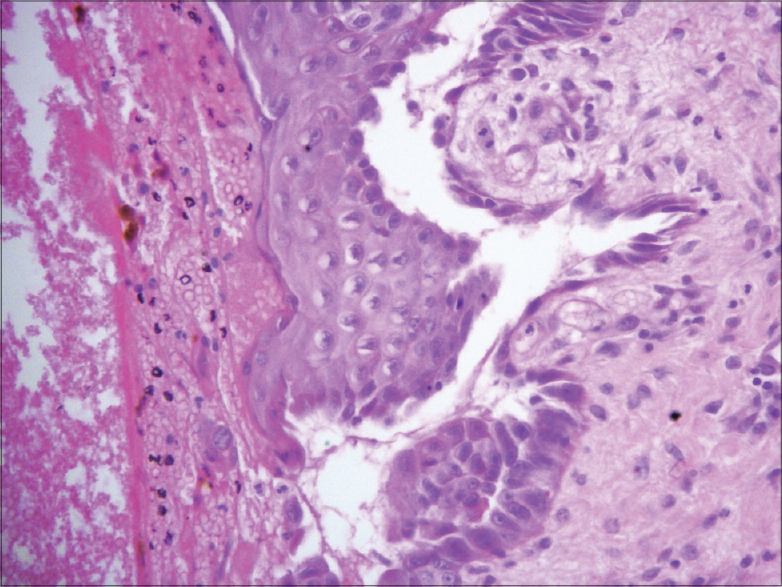 |
| Figure 2: Intraepithelial cleavage with acantholysis primarily localized to the suprabasal region with bulla formation; perivascular inflammatory infiltrate in the dermis (H and E stain, x100) |
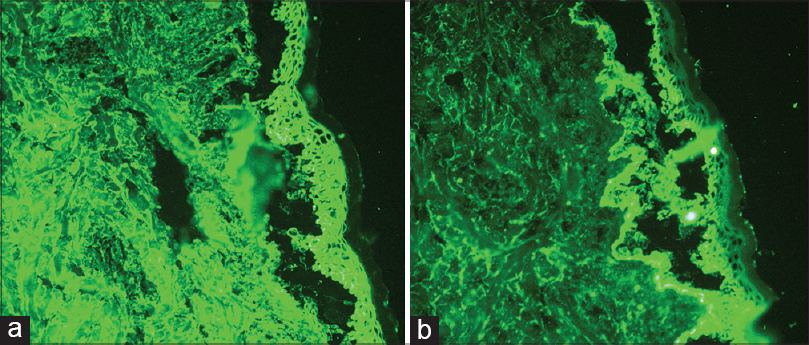 |
| Figure 3: (a and b) The direct immunofluorescence test showed IgG and C3 deposits intercellularly in the epidermis |
The patient was diagnosed to have pemphigus vulgaris and was treated with methylprednisolone (40 mg/day) and azathioprine (50mg/day). The skin lesions gradually healed with no new lesions. However, she developed a low-grade fever on the thirteenth day of treatment. There was significant swelling over the right inguinal region and thigh. There were no respiratory or urinary symptoms and no oral pseudomembrane. The abdominal and pelvic magnetic resonance imaging (MRI) and lower limb digital subtraction angiography (DSA) were negative for intraabdominal or abdominal wall abscesses. Culture of the pus discharge from the skin lesions yielded Staphylococcus aureus (methicillin sensitive) and she was treated with vancomycin.
After 17 days of therapy, methylprednisolone was changed to oral prednisone at a dose of 40mg/day. Azathioprine was discontinued in view of declining white blood cell counts. The patient was discharged after 10 days of therapy with complete resolution of the skin lesions and thigh swelling. She remains asymptomatic at 2 months follow up, and oral prednisone therapy was tapered from then on [Figure - 4].
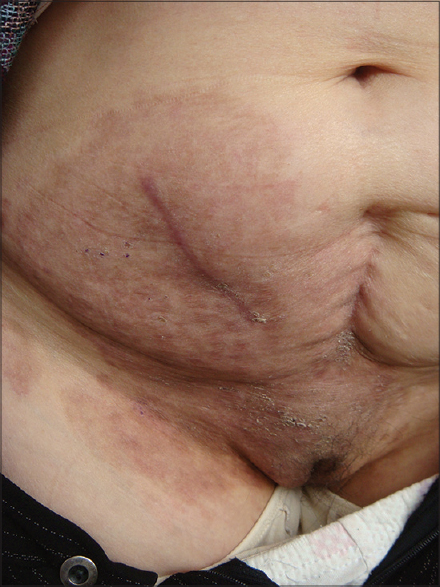 |
| Figure 4: Post inflammatory hyperpigmentation and scaling around the appendectomy scar at one month follow up |
The triggering factors of pemphigus remain unclear. It is multifactorial and involves interaction between genetic predisposition and environmental factors. [1] It also includes medications, physical agents (thermal burns, ultraviolet light, ionizing radiation, and surgery), viral infection, contactants, and even emotional stress.
There have been case reports of pemphigus occurring after contact with certain substances. [2] Iodophor as a possible inciting agent was considered, as it is commonly used as a preoperative antiseptic. However, she did not develop further lesions when iodophor was applied again prior to venipuncture. There was no allergic reaction or blistering when the patient used amoxicillin and cephalosporin, which is reported to be associated with drug-induced pemphigus. Drug-induced pemphigus usually presents with clinical features of pemphigus foliaceus or pemphigus erythematosus. The antibody titers are lower compared to idiopathic pemphigus and negative immunofluorescence results are more frequent.
There have been reports of pemphigus occurring over surgical scars in patients who have a previous history of pemphigus in remission. [3] Reichert-Penetrat reported a case of pemphigus vulgaris over a 40 year old surgical scar in an elderly male with oral ulceration. [4] Our patient had no previous history of oral ulceration, malignancy, or autoimmune disorder. Mehregan et al. also reported a case of pemphigus arising in areas of surgical manipulation after rhinoplasty and hair transplantation between 3 months and 1 year after surgery respectively. [5] Our patient developed skin lesions in and around the appendectomy wound 2 weeks after surgery, suggesting a temporal association between surgery and pemphigus. Although the etiopathology remains unclear, surgery could play a role in triggering the onset of pemphigus vulgaris.
| 1. |
Tron F, Gilbert D, Mouquet H, Joly P, Drouot L, Makni S, et al. Genetic factors in pemphigus. J Autoimmun 2005;24:319-28.
[Google Scholar]
|
| 2. |
Fisher KR, Higginbotham R, Frey J, Granese J, Pillow J, Skinner RB. Pesticide-associated pemphigus vulgaris. Cutis 2008;82:51-4.
[Google Scholar]
|
| 3. |
Duick MG, Zaks B, Moy RL, Kaplan RP. Mohs micrographic surgery-induced pemphigus.Dermatol Surg 2001;27:895-7.
[Google Scholar]
|
| 4. |
Reichert-Penetrat S, Barbaud A, Martin S, Omhover L, Weber M, Schmutz JL. Pemphigus vulgaris on an old surgical scar: Koebner's phenomenon? Eur J Dermatol 1998;8:60-2.
[Google Scholar]
|
| 5. |
Mehregan DR, Roenigk RK, Gibson LE. Postsurgical pemphigus. Arch Dermatol 1992;128:414-5.
[Google Scholar]
|
Fulltext Views
3,380
PDF downloads
1,778





