Translate this page into:
Pemphigus vulgaris localised exclusively to the penis
2 Department of Pathology, Bezmialem Vakif University, Medical Faculty, Istanbul, Turkey
3 Department of Pathology, Istanbul University, Cerrahpasa Medical Faculty, Istanbul, Turkey
Correspondence Address:
Ozlem Su
Sigirtmac Sokak, Park Solare Sitesi, B Blok, Daire 12 Osmaniye/Bakirk�y, Istanbul
Turkey
| How to cite this article: Su O, Dizman D, Ozkaya DB, Yildiz P, Demirkesen C, Onsun N. Pemphigus vulgaris localised exclusively to the penis. Indian J Dermatol Venereol Leprol 2015;81:298-299 |
Sir,
Pemphigus vulgaris is a chronic, autoimmune bullous disease affecting the mucosae and skin. Though disease usually starts in the oral mucosa, which is the most frequently affected site, involvement of other mucosae may be seen. [1] There are only a few reports documenting the involvement of penile skin [2] of which only a single report documents penile erosions as the first manifestation of pemphigus vulgaris in two patients. In both of these cases, pemphigus vulgaris started in the penile area, followed by oral mucosal lesions in both and skin erosions in one patient. [3] We report here a patient with chronic, painful penile erosions with maceration who was diagnosed as pemphigus vulgaris. We were unable to find previous reports of isolated penile pemphigus vulgaris.
A 49-year-old male was admitted to our hospital with painful penile erosions that were slowly progressive for 3½ months. The patient had previously responded poorly to courses of topical and systemic antiviral, antibiotic, antifungal agents, and topical corticosteroids. On dermatological examination, multiple confluent erythematous erosions were observed on the glans, corona, and shaft of the penis. The penile skin had a whitish macerated and fragile appearance [Figure - 1]a. There were no mucosal or cutaneous lesions elsewhere on the body. Treponema pallidum hemagglutination assay (TPHA) and enzyme-linked immunosorbent assay (ELISA) for herpes simplex virus (HSV) type 2 IgM and IgG were negative. A punch biopsy taken from the penile erosion revealed suprabasal blistering with acantholysis [Figure - 2]a and b. Direct immunofluorescence (DIF) studies of the perilesional penile mucosa demonstrated IgG and complement (C3) deposits in the intercellular area [Figure - 3]a and b. ELISA for Dsg3 and Dsg1 were positive in 1:1000 and 1:100 dilutions respectively (normal < 1:10). Based on the results of clinical evaluation and histopathological and immunofluorescence studies a diagnosis of pemphigus vulgaris localized to the penis was made. The patient was treated with oral prednisone (1 mg/kg) and azathioprine (2 mg/kg/day). The penile lesions cleared completely after 3 months of therapy [Figure - 1]b after which the prednisone dose was tapered gradually. Additional skin and other mucosal lesions were not observed during follow-up. The patient remains in remission after 16 months of follow up.
 |
| Figure 1: (a) Multiple erythematous erosions with whitish maceration on the penis. (b) Complete healing occurred after treatment |
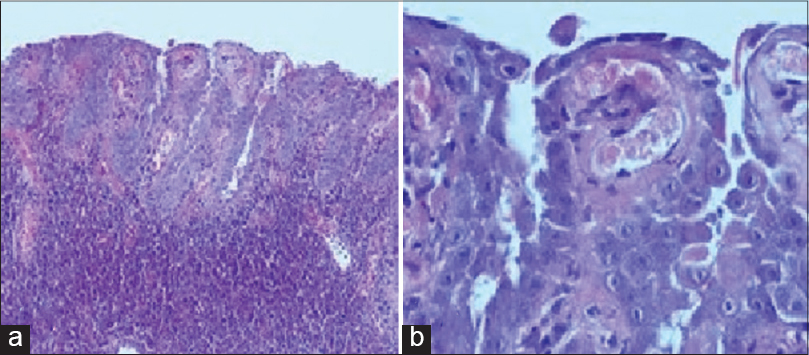 |
| Figure 2: (a) Suprabasal acantholytic blister formation. (H and E ×100) (b) The basal cells show a tombstone appearance together with acantholytic cells (H and E ×400) |
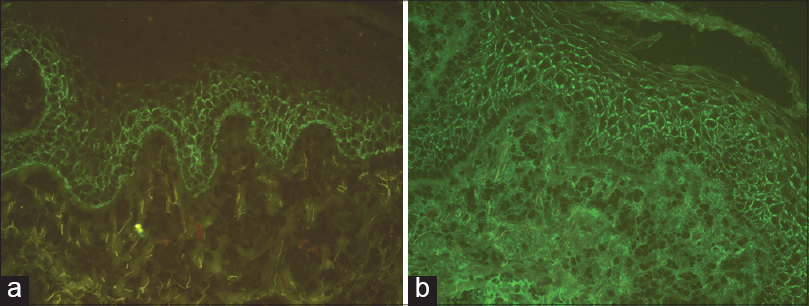 |
| Figure 3: Intercellular epidermal staining for complement C3 (a) and IgG (b) (×100) |
Mucosal involvement occurs commonly in pemphigus vulgaris. Although the oral mucosa is involved most frequently, other mucosal areas may also be affected, albeit less commonly. In a retrospective analysis of 1209 cases, Chams-Davatchi et al. [4] reported involvement of the oral cavity, conjunctiva, nasal, vaginal, laryngeal/esophageal, and perineal mucosae in 81%, 16%, 11%, 9%, 8%, and 2% of cases, respectively. Akhyani et al. have reported a much higher incidence of genital mucosal involvement in 51% of 77 cases with muco-cutaneous involvement. [5] According to this study, the genital mucosa was the second most commonly affected mucosal site in pemphigus vulgaris. In another study, the presence of genital lesions was found to be associated with treatment resistance and was recognized as a poor prognostic factor and a marker of disease severity. [1]
Genital involvement in males with pemphigus vulgaris has been reported only rarely. [2],[3] Sami and Ahmet reported involvement of the penile skin in 12 male patients with pemphigus. However, in none of these cases was the disease limited to penile skin only. [2] Recently, Stieger et al. [3] described two cases of pemphigus vulgaris presenting with erosions over the glans penis and coronal sulcus. In both these patients, though the disease started from penile area it later affected the oral mucosa also. One of the patients also developed cutaneous lesions on follow up. [3] The initial presentation with penile erosions alone led to a delay in diagnosis in both these cases. Both patients were treated with 1 mg/kg/body weight prednisone and azathioprine.
Possible differential diagnoses for long-standing penile erosions include infectious etiologies (herpes simplex virus, syphilis, candidiasis, and mycobacterial infection), fixed drug eruption, erosive lichen planus, genital aphthosis of Behçet′s disease, and premalignant and malignant conditions like plasma cell balanitis, Paget′s disease, erythroplasia of Queyrat and squamous cell carcinoma. Because isolated penile involvement as a presenting feature of pemphigus vulgaris is not commonly described, the diagnosis may be missed. We also believe that the presence of genital lesions in pemphigus vulgaris is indicative of likelihood of resistance to treatment and these patients may require high-dose systemic steroids and stronger immunosuppressive regimens.
| 1. |
Malik M, Ahmed AR. Involvement of the female genital tract in pemphigus vulgaris. Obstet Gynecol 2005;106:1005-12.
[Google Scholar]
|
| 2. |
Sami N, Ahmed AR. Penile pemphigus. Arch Dermatol 2001;137:756-8.
[Google Scholar]
|
| 3. |
Stieger M, Pelivani N, Ramelet AA, Beltraminelli H, Borradori L. Penile erosions as first manifestation of pemphigus vulgaris: A misleading presentation. Acta Derm Venereol 2013;93:248-9.
[Google Scholar]
|
| 4. |
Chams-Davatchi C, Valikhani M, Daneshpazhooh M, Esmaili N, Balighi K, Hallaji Z, et al. Pemphigus: Analysis of 1209 cases. Int J Dermatol 2005;44:470-6.
[Google Scholar]
|
| 5. |
Akhyani M, Chams-Davatchi C, Naraghi Z, Daneshpazhooh M, Toosi S, Asgari M, et al. Cervicovaginal involvement in pemphigus vulgaris: A clinical study of 77 cases. Br J Dermatol 2008;158:478-82.
[Google Scholar]
|
Fulltext Views
5,253
PDF downloads
1,375





