Translate this page into:
Perforating lichen planus
Correspondence Address:
Uday Khopkar
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai 400 012
India
| How to cite this article: Gutte R, Khopkar U. Perforating lichen planus. Indian J Dermatol Venereol Leprol 2011;77:515-517 |
Sir,
Lichen planus (LP) is a common chronic inflammatory papulosquamous disorder affecting skin, mucous membranes, nail, and hairs. [1]
Our patient, a 38-year-old married male presented with gradually increasing occasionally itchy multiple dark colored raised lesions on bilateral palms with pits over them and multiple raised keratotic lesions over bilateral elbows and waistline since 6 months. There was neither history of any drug intake before developing these lesions nor history of jaundice in the past.
Examination showed multiple hyperpigmented, hyperkeratotic somewhat symmetrical plaques with multiple pits over the surface on bilateral palms [Figure - 1]. In addition, multiple keratotic follicular papules, coalescing to form plaques at places, were seen over bilateral elbows and waistline. Rest of the examination including mucosa, nails and hairs was normal. Routine hemogram and biochemical investigations including glucose-6-phosphate dehydrogenase activity were within normal limits.
 |
| Figure 1: Hyperpigmented, hyperkeratotic plaques over palm with pits on the surface |
Differential diagnoses of porokeratosis, lichen nitidus and porokeratotic eccrine ostial and dermal duct nevus were thought.
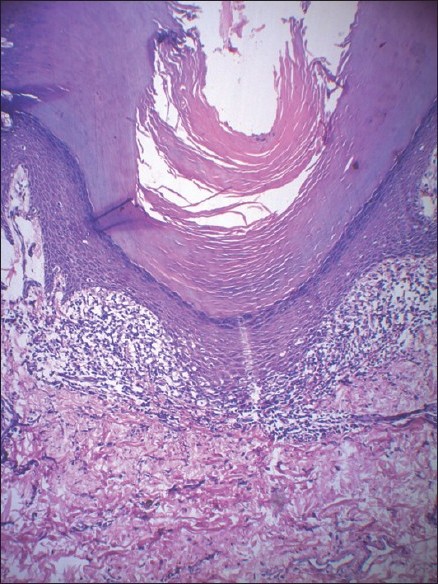
Biopsy taken from a lesion on the palm showed histologic features of lichen planus, viz., thick and compact hyperkeratosis, acanthosis, wedge-shaped hypergranulosis, lymphocytic band-like infiltrate in upper dermis with acrosyringeal accentuation [Figure - 2] and basal layer vacuolization with abundant colloid bodies and melanophages [Figure - 3]. Further sections of the same specimen revealed perforation of epidermis by a parakeratotic plug probably corresponding to the pits seen clinically [Figure - 4]. Based on clinicopathological correlation a diagnosis of perforating LP was made. The patient was started on oral dapsone 100 mg OD and oral antihistamines along with topical clobetasol propionate 0.05% cream twice daily; however, we lost follow-up with the patient.
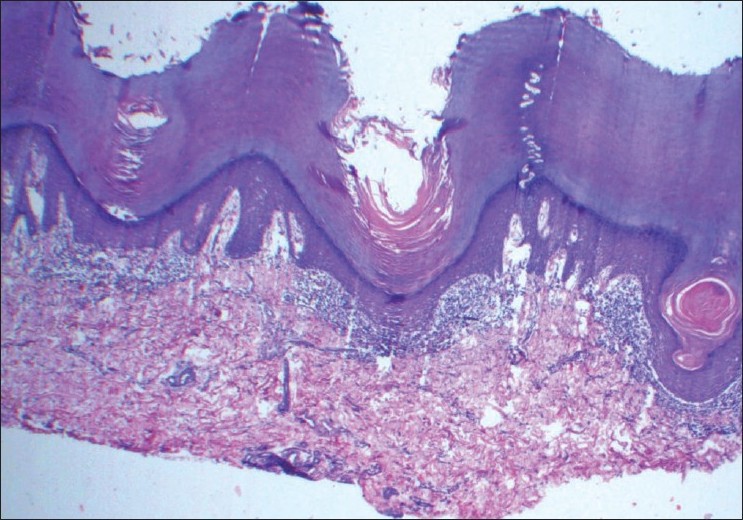 |
| Figure 2: Hyperkeratosis, parakeratosis, wedge-shaped hypergranulosis and band-like lymphocytic infiltrate (H and E, ×40) |
 |
| Figure 3: Close up view showing basal layer vacuolization with colloid bodies (H and E, ×100) |
 |
| Figure 4: High power view showing perforation of epidermis by a parakeratotic plug, acrosyringeal accentuation of infiltrate with interface change. (H and E, ×200) |
Hanau and Sengel [2] reported a case of perforating LP in 1984 in a 52-year-old woman. Histology in their case showed classic picture of LP and perforation of epidermis by a channel containing epithelial cells, hyaline bodies, inflammatory cells, melanophages and fibrilar material. [2] In our case, the perforating channel was made up of a parakeratotic plug.
Enhamre and Lagerholm [3] described six cases of lichen planus with dermal lymphocytic infiltrate in juxtaposition to acrosyringium with liquefactive degeneration of acrosyringeal basal cell layer as a prominent histological finding and coined the term acrosyringeal lichen planus Mugoni et al.[4] described five cases of lichen planus on palms and soles and found acrosyringeal lichen planus in one of them. Hypertrophic palmoplantar lichen planus treated successfully with enoxaparin has been reported recently. [5],[6]
In our case, perforation of epidermis was seen along with acrosyringeal accentuation of infiltrate. Since normal palmoplantar skin has abundant sweat glands and extrapalmar lesion was not biopsied, and because we lost follow up with patient, we called it just perforating lichen planus though there was an additional acrosyringeal accentuation of infiltrate.
Various speculations on the pathogenesis of acrosyringeal variant of LP have been made. Drugs such as β-blockers that are excreted through sweat ducts may influence its physiology by involving β-adrenergic receptors to produce predominant acrosyringeal changes. [3],[4] However, our patient did not have any history of drug intake. Mugoni et al.[4] stated that acrosyringium constitutively expresses class 2 major histocompatibility antigens (HLA-DR, HLA-DP, HLA-DQ) on surface, and this expression of antigens in association with cell mediated immune mechanisms in certain circumstances, could allow antigen presentation to T cells giving rise to immune response that predominantly involves acrosyringium. [4]
Hanau and Sengel [2] speculated that hyaline bodies present abundantly at the base of perforation could irritate the dermo epidermal (D-E) junction and, consequently, initiate the process of perforation of epidermis. [2]
In our case, the perforating channel was made up of a parakeratotic plug, and also abundant colloid bodies were seen below the invagination of epidermis by a parakeratotic plug.
In conclusion, we describe a rare variant of lichen planus with palmar involvement and with distinct clinicopathological features that may be added to well-known variants.
| 1. |
Sánchez-Pérez J, Rios Buceta L, Fraga J, García-Díez A. Lichen planus with lesions on the palms and/or soles: Prevalence and clinicopathological study of 36 patients. Br J Dermatol 2000;142:310-4.
[Google Scholar]
|
| 2. |
Hanau D, Sengel D. Perforating lichen planus. J Cutan Pathol 1984;11:176-8.
[Google Scholar]
|
| 3. |
Enhamre A, Lagerholm B. Acrosyringeal lichen planus. Acta Derm Venereol 1987;67:346-50.
[Google Scholar]
|
| 4. |
Mugoni MG, Montesu MA, Cottoni F. Lichen planus on palms and soles. J Eur Acad Dermatol Venereol 1994;3:535-40.
[Google Scholar]
|
| 5. |
Yasar S, Serdar ZA, Goktay F, Doner N, Tanzer C, Akkaya D, et al. The successful treatment of palmoplantar hyperkeratotic lichen planus with enoxaparin. Indian J Dermatol Venereol Leprol 2011;77:64-6.
[Google Scholar]
|
| 6. |
S, Kathuria SD, Gupta R, Singh MK, Sharma VK. Hyperkeratotic pitted plaques on palms and soles. Indian J Dermatol Venereol Leprol 2010;76:52-5.
[Google Scholar]
|
Fulltext Views
3,116
PDF downloads
1,969





