Translate this page into:
Perifollicular nodule on the face of a young man
Correspondence Address:
Sudip Kumar Ghosh
Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, 1, Khudiram Bose Sarani, Kolkata - 700 004
India
| How to cite this article: Ghosh SK, Bandyopadhyay D, Barma KD. Perifollicular nodule on the face of a young man. Indian J Dermatol Venereol Leprol 2011;77:531-533 |
A 22-year-old man presented with an asymptomatic slow-growing swelling on his face for the preceding 1 year. There was no systemic symptom and no history of similar illness in his family. He underwent electrodessication for the lesion by a dermatologist 1 year back. However, the lesion recurred within 2 months with some residual scarring. On examination, a solitary skin-colored, shiny, firm, and non-tender nodule was seen on the right mandibular area of his face. A wisp of short, wooly, immature hairs was seen emerging from a central orifice of the nodule [Figure - 1]. Perilesional scarring was also present. There was no other mucocutaneous abnormality and systemic examination was non-contributory.
 |
| Figure 1: A solitary shiny nodule with a wisp of short, immature hairs emerging from a central orifice of the nodule |
An excision biopsy was performed followed by histopathologic examination [Figure - 2].
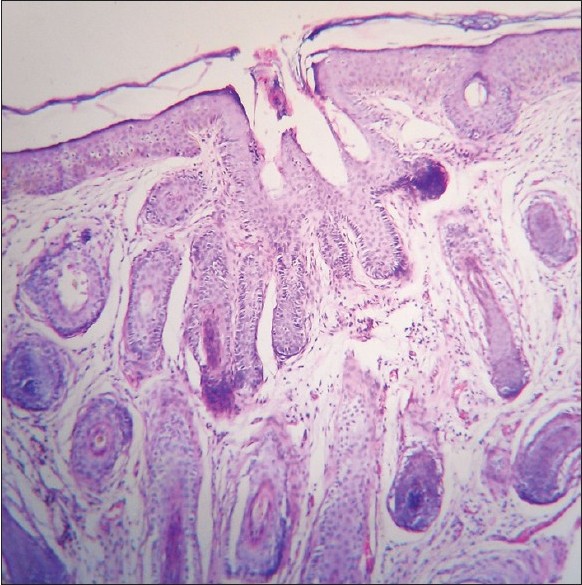 |
| Figure 2: A central cystic space opening to the skin surface with fully formed or nearly fully formed follicles radiating from it (H and E, ×100) |
What is your Diagnosis?
Answer: Trichofolliculoma
Histopathologic examination showed a central cystic space with infundibular cornification and an opening to the skin surface from which fully formed or nearly fully formed follicles radiated. This histological picture along with the distinctive morphology of the lesion confirmed the diagnosis.
Discussion
Trichofolliculoma usually presents as a papule or nodule, located on the face, scalp, upper trunk, vulva, and rarely on the eyelids. [1],[2],[3] The lesion often mimics a basal cell carcinoma, molluscum contagiosum, dermal nevus, epidermoid cyst, or trichoepithelioma. [1],[4] A tuft of white vellus hairs emanating from the nodule, when present, gives a distinctive morphological appearance to this tumor. [3] Rarely, trichofolliculoma may present as a large nodule or cyst. [1] Trichofolliculoma is common in the middle age, rare in childhood, [4] and at least one case has been reported to occur congenitally. [5] There is no definitive racial or gender predilection of this disease. [4]
The nosology of trichofolliculoma is less clear-cut. Although often regarded as a "tumor" of the hair follicle, it does not represent a true neoplasm. Rather, it should be considered as a benign follicular hamartoma. [1] Although the precise etiology of trichofolliculoma is uncertain, these tumors are not associated with any systemic disease or other skin disorders and they are believed to represent abortive differentiation of pluripotent skin cells toward hair follicles. [4] Usually, these tumors develop spontaneously, but a prior history of trauma at the tumor site may rarely be present.
Histological feature of trichofolliculoma comprises of an abnormally dilated pilosebaceous canal containing multiple poorly formed hairs with multiple pilosebaceous-like structures opening into it. [3] Fine needle aspiration cytology of trichofolliculoma may reveal cohesive, branching, keratinized squamous cell clusters admixed with sebaceous cells. [6] Trichofolliculoma is characterized by proliferation of abnormal CK15-positive hair follicle stem cells, which basically differentiate toward the outer root sheath and attempt to make hair but lose the proper differentiation. [7] Trichofolliculoma is essentially a benign condition, but malignant transformation with perineural invasion has been reported in a single case report. [8] Folliculosebaceous cystic hamartoma is believed to be a larger cystic variant of trichofolliculoma in a late stage of development by some authors. [9] According to another view, these two disorders are distinctive entities. They may develop under a similar pathogenesis, differing from each other only in the direction of differentiation. [10] Another variant of trichofolliculoma with prominent sebaceous lobules and referred to as "sebaceous trichofolliculoma" is not of any additional clinical significance. [1] Treatment of trichofolliculoma is usually not required. [1] At times, trichofolliculoma may be disfiguring, and the pulling away of hairs and other injuries may cause inflammatory reactions requiring treatment. [2] Surgical excision is usually the treatment of choice. [2],[3] The prognosis is excellent, although recurrence can occur at the primary site rarely. [4]
| 1. |
McCalmont TH. Adnexal neoplasms. In: Bolognia JL, Jorrijo JL, Rapini RP, editors. Dermatology. 2nd ed. Philadelphia: Mosby Elsevier; 2008. p. 1693-1712.
[Google Scholar]
|
| 2. |
Carreras B Jr, Lopez-Marin I Jr, Mellado VG, Gutierrez MT. Trichofolliculoma of the eyelid. Br J Ophthalmol 1981;65:214-5.
[Google Scholar]
|
| 3. |
Mackie RM, Calonje E. Tumors of the skin appendages. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook′s Textbook of Dermatology. 8th ed. Oxford: Wiley-Blackwell; 2010. p. 53.1-53.44.
[Google Scholar]
|
| 4. |
Howard MS, Smoller BR. Trichofolliculoma. e-Medicine Dermatology. Available from: http://emedicine.medscape.com. [Last accessed on 2010 Aug 2].
[Google Scholar]
|
| 5. |
Ishii N, Kawaguchi H, Takahashi K, Nakajima H. A case of congenital trichofolliculoma. J Dermatol 1992;19:195-6.
[Google Scholar]
|
| 6. |
Alexander MP, Makhija P, Jayaseelan E. Fine needle aspiration cytology of trichofolliculoma: A case report. Indian J Pathol Microbiol 2007;50:870-2.
[Google Scholar]
|
| 7. |
Misago N, Kimura T, Toda S, Mori T, Narisawa Y. A revaluation of trichofolliculoma: The histopathological and immunohistochemical features. Am J Dermatopathol 2010;32:35-43.
[Google Scholar]
|
| 8. |
Stern JB, Stout DA. Trichofolliculoma showing perineural invasion. Trichofolliculocarcinoma? Arch Dermatol 1979;115:1003-4.
[Google Scholar]
|
| 9. |
Schulz T, Hartschuh W. Folliculo-sebaceous cystic hamartoma is a trichofolliculoma at its very late stage. J Cutan Pathol 1998;25:354-64.
[Google Scholar]
|
| 10. |
Misago N, Kimura T, Toda S, Mori T, Narisawa Y. A revaluation of folliculosebaceous cystic hamartoma: The histopathological and immunohistochemical features. Am J Dermatopathol 2010;32:154-61.
[Google Scholar]
|
Fulltext Views
4,109
PDF downloads
2,967





