Translate this page into:
Periumbilical keratotic papules
Correspondence Address:
S Veeranna
Department of Skin and STD, J.S.S. Hospital, Ramanuja Road, Mysore, Karnataka
India
| How to cite this article: Veeranna S, K, Betkerur J, S. Periumbilical keratotic papules. Indian J Dermatol Venereol Leprol 2006;72:178 |
 |
 |
 |
 |
A 60-year-old obese female presented with skin lesions over the abdomen since 4 years. They were gradual in onset, progressive in nature and were associated with mild pruritus. She had been suffering from diabetes mellitus since the past 10 years. She had undergone a laparotomy 5 years back.
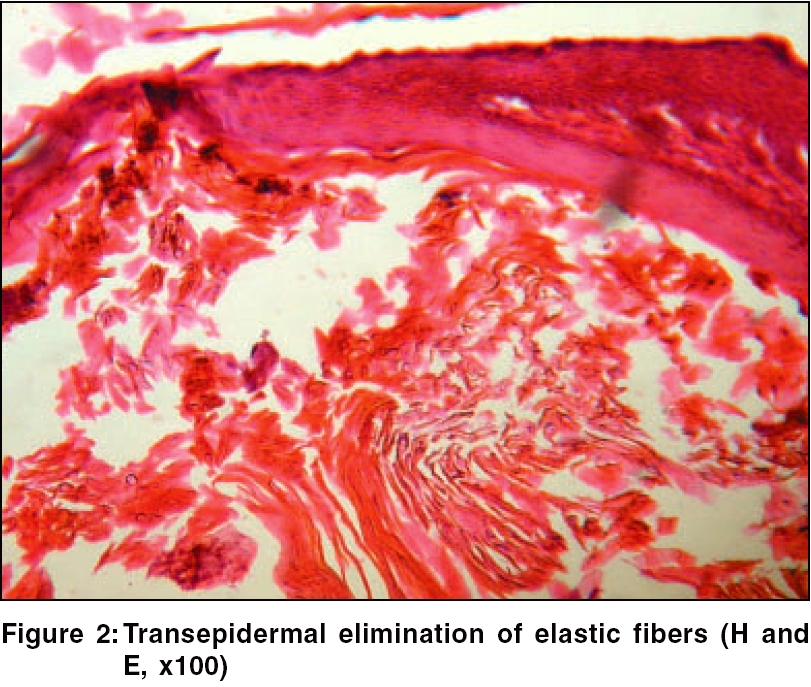
Cutaneous examination showed lax skin over the abdomen. A linear paramedian scar was present. Multiple striae were seen over the anterior abdominal wall. Multiple dome shaped papules measuring 2-5 mm in size with keratotic plugs were seen over the periumbilical area [Figure - 1].
Ophthalmological and other systemic examinations were normal. Routine hemogram and urinalysis were normal. Random blood sugar was 330 mg%. Blood urea and serum creatinine were normal.
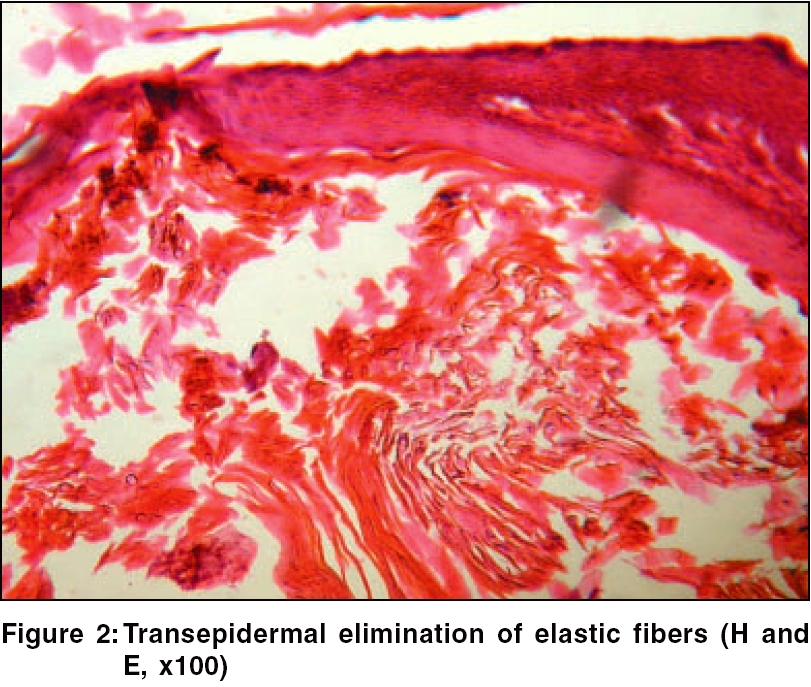
Histopathological examination of the skin biopsy material from a keratotic papule showed hyperkeratosis and perforation of epidermis with elastic fibers. There were areas of calcification. Elastic fibers were seen arranged vertically perforating the epidermis [Figure - 2]. Von Kossa stain showed calcium deposition in the dermis.
What is your diagnosis?
Diagnosis: Perforating calcific elastosis
Discussion
Perforating disorders of the skin comprises a group of unrelated pathologic abnormalities sharing the common characteristics of transepidermal elimination.[1] The classical examples are Kyrle′s disease, elastosis perforans serpiginosa, reactive perforating collaginosis and perforating folliculitis. Patients with diabetes mellitus and chronic renal failure also show similar skin changes, which are grouped separately.[1] Several other unrelated disorders like granuloma annulare, PXE and chondrodermatitis nodularis helices also show transepidermal elimination as a secondary phenomenon.[1]
Perforating calcific elastosis (PCE), also known as periumbilical pseudoxanthoma elasticum, is an acquired localized cutaneous disorder, most frequently found in obese, multiparous, middle-aged women.[2] It is a rare type of acquired perforating disorder in which altered elastic fibers are extruded through the process of transepidermal elimination. It is seen over the periumbilical area and rarely over the breast.[3]
It has been suggested that the stretching of the skin due to repeated pregnancy, obesity and abdominal surgery promote elastic fiber degeneration resulting in PCE.[4] Initial eruption may contain asymptomatic or mildly pruritic erythematous papules, plaques or nodules. Over the course of several months or years, the lesion tends to resolve, leaving a well-demarcated, hyperpigmented, reticulate, atrophic central plaque with raised, scaly border. Discrete, horny, hyperkeratotic papules may be scattered around the periphery. Lesions range in size from 2-15 cm and may be circular or oval.[4]
Histological examination reveals numerous altered elastic fibers in the reticular dermis. They are short, thick, curly and studded with calcium.[1] Channels extruding inflammatory and elastotic debris from the reticular dermis to the overlying epidermis may be seen. Eosinophilic intrapapillary elastoma may also be observed.[4]
PCE may be associated with other abnormalities like uremia, hyperphosphatemia and angioid streaks.[4]
Transepidermal elimination of altered elastic fibers can occur as a localized acquired defect in a patient who does not have other features of pseudoxanthoma elasticum.[5] It is a distinct disorder which shares some features of PXE (both acquired and inherited), without systemic involvement. The histopathological features of these two conditions are similar but in PCE, there is transepidermal elimination of altered basophilic calcified elastic fibers, which are short, fragmented and curled.[3] Other conditions that mimic PCE are elastosis perforans serpiginosa, calcinosis cutis, late onset focal dermal elastosis and amyloid elastosis.[4]
There is no specific treatment. Topical steroids and hemodialysis have been tried. Spontaneous resolution has also been reported.[4]
| 1. |
Heilman ER, Freidman RJ. Degenerative disease and perforating diseases. In: Elder D, Elenitsas R, Jaworsky C, Johnson Jr. B, editors. Lever's Histopathology of skin. 8th ed. Lippincott-Raven: Philadelphia; 1997. p. 341-51.
[Google Scholar]
|
| 2. |
Odom RB, James WD, Berger TG. Abnormalities of dermal connective tissue. In: Odom RB, James WD, Berger TG, editors. Andrew's Diseases of the skin: Clinical Dermatology. 9th ed. WB Saunders Co: Philadelphia; 2000. p. 640-1.
[Google Scholar]
|
| 3. |
Burton JL, Lovell CR. Disorder of connective tissue. In: Champion RH, Burton JL, Burns DA. Breathnach SM, editors. Rook/ Wilkinson/ Ebling Textbook of dermatology. 6th ed. Oxford: Blackwell Science; 1998. p. 2003-72.
[Google Scholar]
|
| 4. |
Lewis KG, Bercovith L, Dill SW, Robinson-Bostom L. Acquired disorders of elastic tissue: Increased elastic tissue and solar elastotic syndromes. J Am Acad Dermatol 2004;51:1-18.
[Google Scholar]
|
| 5. |
Premalatha S, Yesudian P, Thambia AS. Periumbilical PXE with transepidermal elimination. Int J Dermatol 1982;10:604-5.
[Google Scholar]
|
Fulltext Views
3,711
PDF downloads
2,766





