Translate this page into:
Periungual deep-seated granulomatous pyoderma gangrenosum
2 Department of Anatomopathology, Fattouma Bourguiba Hospital, Monastir, Tunisia
Correspondence Address:
Kamar Belhareth
35 Rue Habib Thameur, Eljem
Tunisia
| How to cite this article: Soua Y, Belhareth K, Lahouel M, Hadhri R, Akkari H, Belhadjali H, Youssef M, Zili J. Periungual deep-seated granulomatous pyoderma gangrenosum. Indian J Dermatol Venereol Leprol 2020;86:540-542 |
Sir,
Pyoderma gangrenosum is an uncommon neutrophilic dermatosis, classically presenting as inflammatory and painful cutaneous ulcerations of the lower extremities. The periungual location is rare. A 50-year-old woman presented with an erythematous pustular plaque on the left leg and paronychia of the left index finger with nail dystrophy for 1 year. Cutaneous examination revealed a 4-cm erythematous plaque with several pustules on the left lower leg. She also had paronychia of the left index finger with the presence of pustules; nail dystrophy and limitation of the flexion of the distal interphalangeal joint [Figure - 1] and [Figure - 2]. The patient denied any previous local trauma. She had been treated previously with systemic and topical antifungals without improvement. The mycological and bacteriological samples from the pustules from both lesions were negative. An ultrasound of the finger was suggestive of arthritis and synovitis of the distal interphalangeal joint. A grayscale ultrasound showed intra-articular tissue that was abnormally thickened, hypoechoic and poorly compressible. Skin biopsy of skin from the leg lesion showed an intense neutrophilic infiltrate with neutrophilic pustules in the superficial dermis, accompanied by edema, interspersed lymphocytes, and other inflammatory cells. Another biopsy performed from the pustules on the index finger showed deep granulomatous inflammation consisting of epithelioid cells, giant cells and peripheral lymphoid cells with central microabscess [Figure - 3]. Special stains for bacteria, fungi and mycobacteria failed to reveal any pathogenic organisms and there was no suggestion of foreign body granuloma. The diagnosis of pyoderma gangrenosum in its pustular form on the leg and in its “granulomatous” form on the finger was made. The following laboratory examinations revealed negative or normal findings: complete blood cell count, serum chemistry, cryoglobulin, rheumatoid factor, antinuclear antibodies, chest X-ray and tuberculin skin test. The patient was treated with prednisolone at a dose of 1 mg/kg/day for 3 months with a good clinical outcome and both lesions of leg and index finger responded rapidly [Figure - 4].
 |
| Figure 1: Paronychia of the left index finger; with the presence of pustules and nail dystrophy |
 |
| Figure 2: Erythematous plaque with several pustules on the left lower leg |
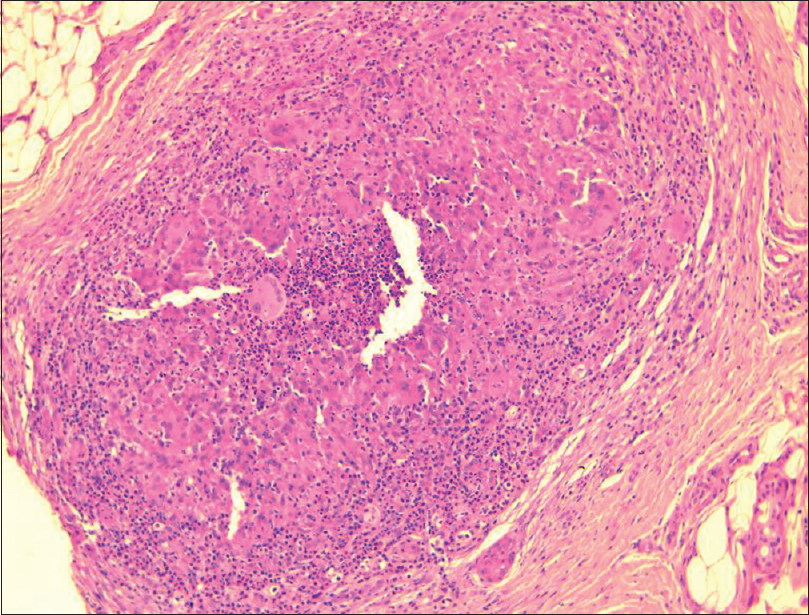 |
| Figure 3: Deep granuloma with central microabscess (H and E,×40) |
 |
| Figure 4: Favorable outcome of both lesions of leg and index finger after treatment |
Periungual pustular pyoderma gangrenosum with deep granulomas in the dermis is a rare presentation. Pustular psoriasis was suspected, especially due to the presence of synovitis and arthritis of the distal interphalangeal joint, but this diagnosis was excluded on skin biopsy. In addition, the good outcome achieved with oral corticosteroids supported the diagnosis of pyoderma gangrenosum. Only five cases of periungual pyoderma gangrenosum have been reported: three cases in its ulcerative form, one case in its bullous form and one case in its pustular variant.[1],[2],[3] Nail dystrophy was absent in all reported cases.
Granulomas were reported in a very rare pyoderma gangrenosum variant: superficial granulomatous pyoderma, which corresponds to the vegetative form. Classically, it presents as a localized form of chronic pyoderma gangrenosum with granulomatous histology. It is characterized by a benign but chronic course, superficial ulceration, truncal involvement and good outcome to less aggressive therapy. Granulomas are classically localized superficially in the upper dermis with a characteristic finding of three-layered granulomas: a superficial zone of abscess formation, a midzone of histiocytes and giant cells and an outer layer of mixed infiltrate of lymphocytes, plasma cells neutrophils and eosinophils. Only four cases of pyoderma gangrenosum with deep granulomatous infiltrate have been reported.[4],[5] Moreover, no three-layered granuloma was found in our case.
In conclusion, our case has drawn attention because of its unusual clinical and histological appearance. It demonstrated the clinical features of the pustular variant of Powell with deep granulomatous inflammation. Therefore, it may represent a distinct subset of pyoderma gangrenosum. However, we believe that other similar case reports are needed to clarify whether it is a distinct entity or not. Meanwhile, we recommend that recognizing this situation seems important to establish appropriate diagnosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hasmoni MH, Hilmi I, Goh KL. Education and imaging: Gastrointestinal: An unusual cause of gastric outlet obstruction. J Gastroenterol Hepatol 2013;28:585.
[Google Scholar]
|
| 2. |
Shinagawa M, Ishige T, Igarashi Y, Takizawa T, Arakawa H. Pyoderma gangrenosum of the finger associated with pediatric ulcerative colitis. J Pediatr Gastroenterol Nutr 2019;69:e88.
[Google Scholar]
|
| 3. |
Reich A, Maj J, Cisło M, Szepietowski JC. Periungual lesions in pyoderma gangrenosum. Clin Exp Dermatol 2009;34:e81-4.
[Google Scholar]
|
| 4. |
Baline K, Khadir K, Chiheb S, Marnissi F, Benchikhi H. Deep-seated granulomatous pyoderma gangrenosum: A novel variant?. Ann Dermatol Venereol 2015;142:340-5.
[Google Scholar]
|
| 5. |
Park HJ, Kim YC, Cinn YW, Yoon TY. Granulomatous pyoderma gangrenosum: two unusual cases showing necrotizing granulomatous inflammation. Clin Exp Dermatol 2000;25:617-20.
[Google Scholar]
|
Fulltext Views
4,108
PDF downloads
1,919





