Translate this page into:
Persistent perioral papules in a young man
2 Department of Dermatology , KPC Medical College, Kolkata, West Bengal, India
Correspondence Address:
Piyush Kumar
Katihar Medical College, Katihar, Bihar
India
| How to cite this article: Kumar P, Das A, Barkat R. Persistent perioral papules in a young man. Indian J Dermatol Venereol Leprol 2019;85:407-409 |
Case History
A 22-year-old otherwise healthy male presented with asymptomatic persistent 2-4mm sized papules distributed over the perioral region for the preceding 2 years. The lesions were asymptomatic but the patient reported a tendency to pick at the lesions. His medical as well as surgical history was non-contributory. On examination, multiple, soft-to-firm, flesh-colored to hyperpigmented papules were noted in the perioral area [Figure - 1]. Rest of the mucocutaneous and systemic examination was unremarkable. The lesions had not responded to anti-acne therapy, including benzoyl peroxide, tretinoin and adapalene.
 |
| Figure 1: Multiple flesh-colored to hyperpigmented papules in the perioral location |
Routine blood investigations including complete blood count, biochemical profile and serum angiotensin converting enzyme estimation were normal. Serology for human immunodeficiency virus and Venereal Disease Research Laboratory test were negative. A 3-mm punch biopsy was taken from a representative papule.
Histopathological findings showed moderately dense superficial and deep perivascular and periappendageal infiltrate of lymphocytes and eosinophils. Hair follicles showed enlargement of infundibulum with deposition of abundant mucin within the infundibular keratinocytes. The infundibulum also showed mild spongiosis and lymphocytic infiltration. Overlying epidermis was unaffected. Alcian blue stain showed blue staining areas confirming mucinous degeneration [Figure - 2]a, [Figure - 2]b and [Figure - 3]. Of note, infiltrating lymphocytes did not show any features of atypia. Immunohistochemistry could not be done for lack of facilities at our institute.
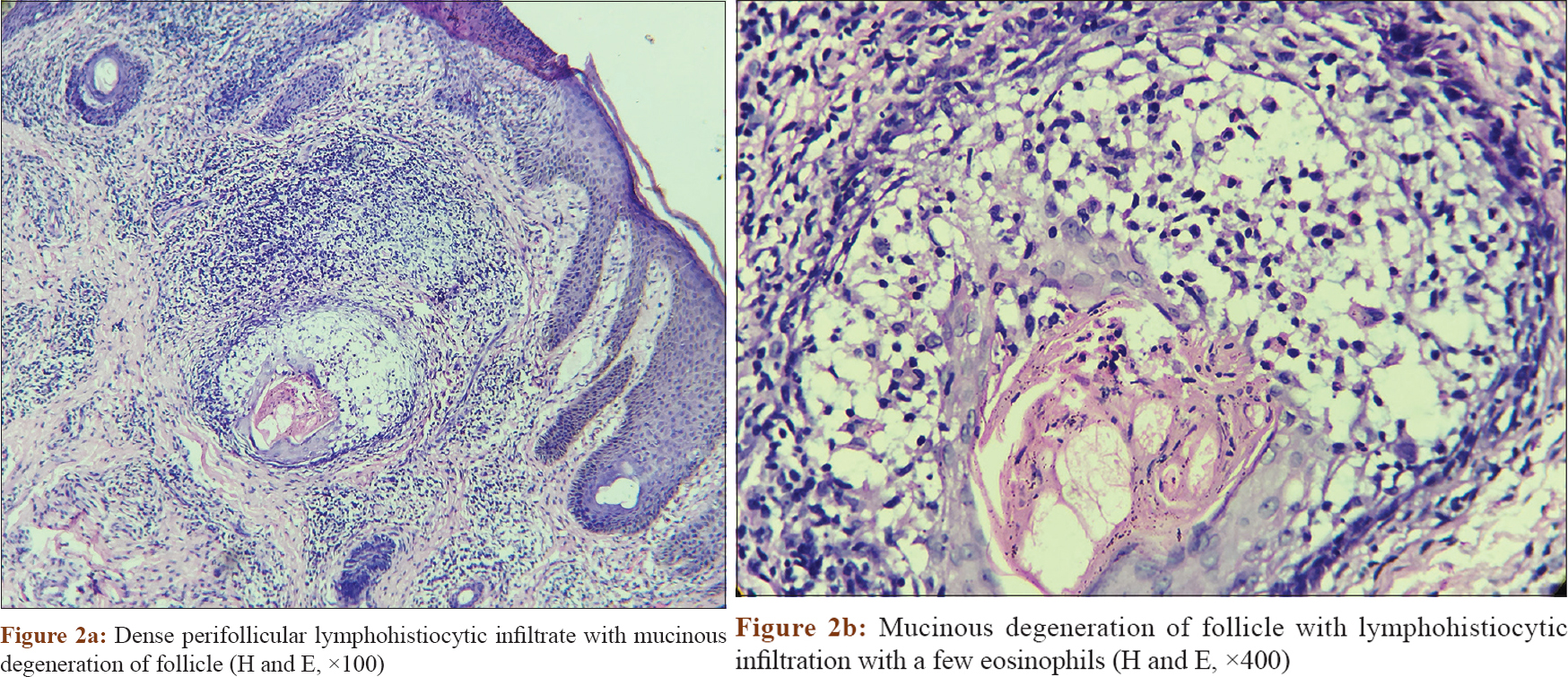 |
| Figure 2: |
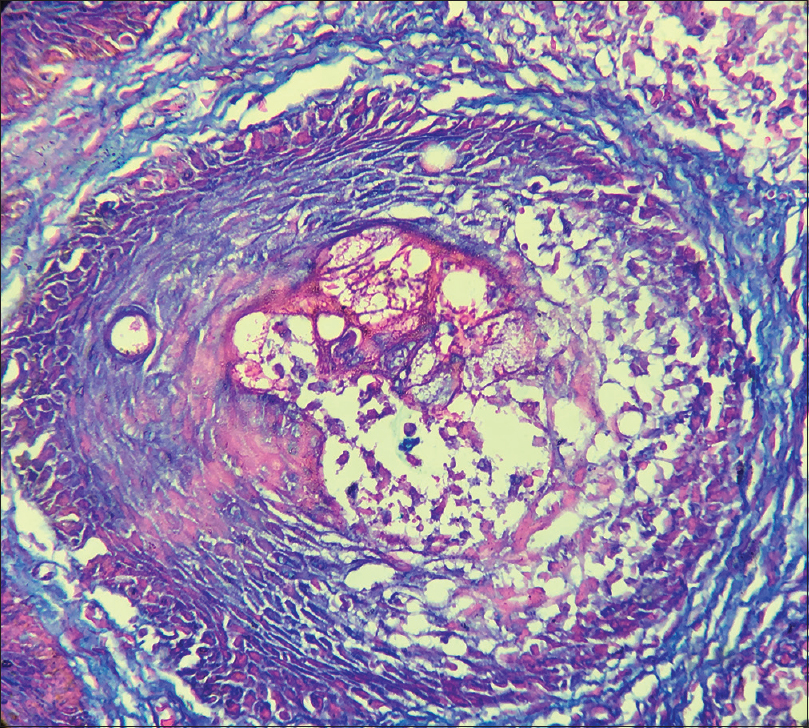 |
| Figure 3: Mucinous degeneration of follicle (Alcian blue, ×400) |
What Is Your Diagnosis?
Diagnosis
Histopathologic findings were consistent with follicular mucinosis. Considering clinical findings, a diagnosis of acneiform follicular mucinosis was made.
Discussion
Follicular mucinosis is a disorder characterized by mucinous degeneration of follicle on histopathology and clinically presents as follicular prominences, alopecia and/or comedone-like plaques.[1] The condition was first described as “alopecia mucinosa” by Pinkus in 1957, and since then, both terms have been used interchangeably.[2]
Follicular mucinosis has been documented in all races and ages and affects both sexes equally.[3] It has been described mainly in two clinical settings – an idiopathic or primary form which usually presents in children and young adults and may show spontaneous remission, and the other lymphoma-associated form which presents in older population and runs a chronic course. Most lymphoma-associated cases are seen in association with mycosis fungoides.[3]
Primary and lymphoma-associated forms have some distinguishing clinical and histopathological features. The lesion in primary follicular mucinosis is solitary in a majority of cases (65%) and is usually restricted to the head and neck region. It is commoner in younger population and often resolves spontaneously. On the other hand, lesions in lymphoma-associated forms are often multiple and widespread on the trunk and extremities. It is seen in older population and does not show spontaneous regression.[3] However, these clinical findings are not absolute.
Deposition of mucin, beginning in the outer root sheath and sebaceous apparatus of hair follicles and perifollicular infiltrate, are the histopathological hallmarks of follicular mucinosis. The inflammatory cell infiltrate in the primary form is predominantly perifollicular and perivascular, whereas infiltrate in lymphoma-associated form is more dispersed, nodular and consists of more plasma cells and fewer eosinophils. Moreover, atypical lymphocytes (enlarged hyperchromatic nuclei with irregular contours) with epidermotropism are frequently seen in lymphoma-associated forms. Of note, mucin deposition is abundant in primary follicular mucinosis in comparison to lymphoma-associated mucinosis. However, overlap of histological features has been described in the literature.[3],[4]
Acneiform follicular mucinosis has also been described as a rare variant of primary follicular mucinosis which presents with erythematous-to-skin-colored papules on the face. The disease runs a chronic course and the lesions may persist for months to years. The differential diagnoses include perioral dermatitis (reddish papules, vesicles and pustules on an erythematous base with a tendency to coalesce), facial demodicosis (facial itching, erythema, seborrheic dermatitis-like eruption mimicking perioral dermatitis), granulomatous periorificial dermatitis (yellow-to-brown papular lesions over perioral, perinasal and periocular regions, common in children), sarcoidosis (histology shows noncaseating granulomas), etc., Various treatment options have been tried effectively including tetracycline, minocycline, isotretinoin, topical tacrolimus and pimecrolimus.[5] Our patient did not report much improvement after a 1 month course of oral minocycline 100mg once daily and was later lost to follow up. The prognosis of such cases is uncertain, and hence, long-term follow-up and monitoring is essential.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Yaman B, Gerçeker Türk B, Öztürk G, Ertam I, Kandıloǧlu G, Akalin T, et al. Follicular mucinosis and follicular mycosis fungoides: Clinicopathological evaluation of seven cases. Turk Patoloji Derg 2013;29:108-16.
[Google Scholar]
|
| 2. |
Böer A, Ackerman AB. Alopecia mucinosa or follicular mucinosis – The problem is terminology! J Cutan Pathol 2004;31:210-1.
[Google Scholar]
|
| 3. |
Rongioletti F, De Lucchi S, Meyes D, Mora M, Rebora A, Zupo S, et al. Follicular mucinosis: A clinicopathologic, histochemical, immunohistochemical and molecular study comparing the primary benign form and the mycosis fungoides-associated follicular mucinosis. J Cutan Pathol 2010;37:15-9.
[Google Scholar]
|
| 4. |
Mehregan DA, Gibson LE, Muller SA. Follicular mucinosis: Histopathologic review of 33 cases. Mayo Clin Proc 1991;66:387-90.
[Google Scholar]
|
| 5. |
Brau-Javier CN, Santos-Arroyo AE, De Sanctis-González IM, Sánchez JL. Follicular mucinosis presenting as an acneiform eruption: A follow-up study. Am J Dermatopathol 2013;35:792-6.
[Google Scholar]
|
Fulltext Views
4,109
PDF downloads
2,203





