Translate this page into:
Phacomatosis pigmentokeratotica: A very rare twin spotting phenomenon
Correspondence Address:
Bela J Shah
Department of Skin and VD, Room No. 139, 1st Floor, Wing No. 3, OPD Building, Civil Hospital, Asarwa, Ahmedabad, Gujarat
India
| How to cite this article: Karia DR, Solanki AN, Jagati AG, Shah BJ. Phacomatosis pigmentokeratotica: A very rare twin spotting phenomenon. Indian J Dermatol Venereol Leprol 2018;84:120 |
Sir,
Phacomatosis pigmentokeratotica is a rare and distinct form of epidermal nevus syndrome characterized by epidermal nevus (usually nevus sebaceus), papular nevus spilus and extracutaneous anomalies.[1] This type of twin spot phenomenon (didymosis) is due to postzygotic crossing-over resulting in two homozygous daughter cells, representing the stem cells of the two distinct types of nevi and of the additional extracutaneous defects.[2] This syndrome is an example of cutaneous mosaicism. We report this syndrome, previously known as didymosis spilosebacea, in an 18-year-old man.
An 18-year-old man presented to the dermatology outpatients' department, with the complaints of brownish skin lesions since birth. He also complained of excessive sweating of the underarms, palms and soles and sweat-soaked clothing. He was born to healthy non-consanguineous parents through a normal vaginal delivery with an insignificant antenatal and birth history. Family history was unremarkable.
On examination, we found multiple, yellowish-brown hyperkeratotic velvety plaques following Blaschko's lines over the right side of the face, extending to scalp leading to localized alopecia on the right temporal area, postauricular region and neck. There was a large light brown patch extending unilaterally from the right side of chin, to the neck, chest, axilla, upper back and right upper limb, overlying which were multiple small brownish-black macules and papules [Figure - 1], [Figure - 2], [Figure - 3]. Overall clinical examination suggested the existence of two different types of nevi, i.e., nevus sebaceus along the Blaschko's lines and speckled lentiginous nevus in a segmental distribution. There was also bilateral low-grade volar and mild axillary hyperhidrosis. (sweat stains on clothing: <5 cm is considered normal; 5–10 cm, mild; 10–20 cm, moderate; and >20 cm, severe).
 |
| Figure 1: Nevus sebaceus on the right side of the face and neck, speckled lentiginous nevus involving the right side of chin, neck and right upper limb |
 |
| Figure 2: Nevus sebaceus extending to scalp and postauricular region |
 |
| Figure 3: Nevus spilus on the right side of the back |
Orthopedic evaluation showed mild scoliosis with kyphotic angle 15° which was clinically inapparent. Skin biopsy from lesions on cheek showed papillomatous epidermal hyperplasia, enlarged sebaceus lobules and buds of follicular germinative cells along the dermoepidermal junction, suggestive of nevus sebaceus [Figure - 4]. Biopsy from the lesion on the back showed nests of melanocytes in dermis corresponding to the speckles, and increased number of melanocytes in the superficial epidermis with hyperpigmentation of the basal epidermis corresponding to the patch [Figure - 5].
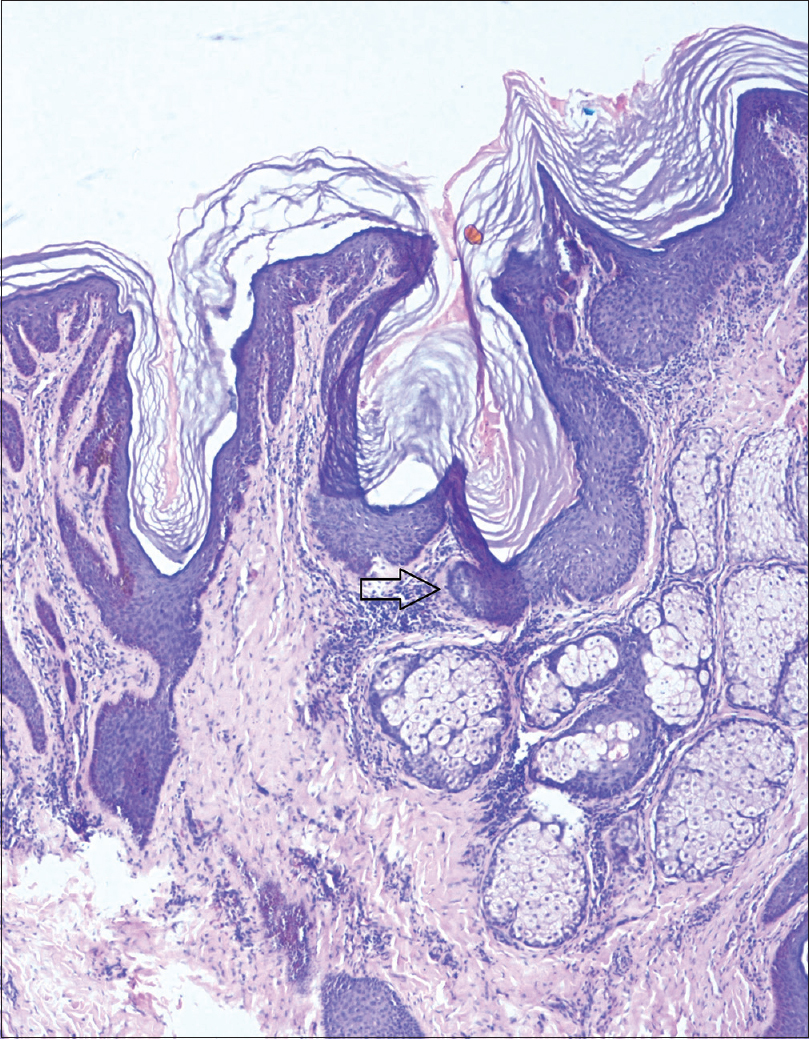 |
| Figure 4: Nevus sebaceous showing buds of follicular germinative cells along the dermoepidermal junction (H and E, ×100) |
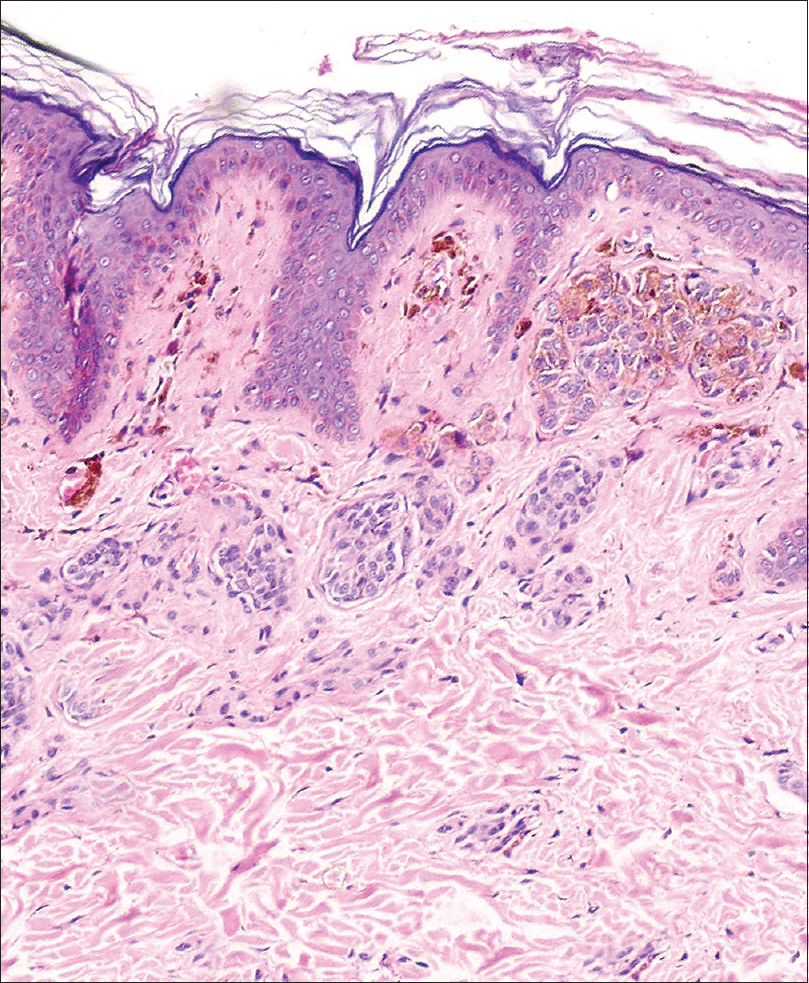 |
| Figure 5: Nevus spilus showing nests of melanocytes in dermis corresponding to the speckles (H and E, ×100) |
All the routine investigations, ophthalmic, otologic and neurological evaluation showed no abnormality. Serum levels of vitamin D3, ionized calcium and phosphate were within normal limits.
We commenced treatment with cryotherapy (for nevus sebaceus on scalp - planned for six sessions two weeks apart) and radiofrequency ablation (for nevus sebaceus on postauricular region - planned for three sessions two weeks apart), and the patient is on regular follow-up. We also referred the patient to plastic surgery department for serial surgical excision of nevus sebaceus on the face, but patient denied surgery. No intervention was done for the nevus spilus.
Phacomatosis pigmentokeratotica has the epidermal component of Schimmelpenning syndrome, but the associated extracutaneous manifestations do not comprise major central nervous system or ophthalmic anomalies. Phacomatosis pigmentokeratotica was first described by Happle based on a series of some patients previously reported in the literature.[2] It was defined as multiple organoid nevi with sebaceus differentiation, arranged along the Blaschko's lines, along with speckled lentiginous nevus in a checkerboard pattern.[3] Till date, 34 cases of this syndrome have been documented which have contributed to the improved characterization of the syndrome.
Phacomatosis pigmentokeratotica has a male:female ratio of 2.4:1.[4] The most frequently associated extracutaneous alterations are neurologic (hemiatrophy with muscular weakness, hyperhidrosis and dysesthesia in the region of the speckled lentiginous nevus), ophthalmologic (strabismus and ptosis) and skeletal disorders (postural deviation with the appearance of kyphosis/scoliosis). Many other alterations have also been described e.g., ichthyosis-like diffuse hyperkeratosis, laxity of the hands, pelvic hypoplasia, glaucoma, deafness, psychomotor retardation and hypophosphatemic rickets. The patient must also be followed up for the rare occurrence of trichoblastoma in the nevus sebaceus.[3]
Twin spot phenomenon (didymosis) is due to postzygotic crossing-over resulting in two homozygous daughter cells, representing the stem cells of the two distinct types of nevi and of the additional extracutaneous defects. Latest research has shown that the paired nevi originate from one single multipotent progenitor cell being heterozygous for an HRAS mutation. Thus, the theory of didymosis (twin spotting phenomenon) can no longer be upheld and the disorder should be regarded as “pseudodidymosis.” This discovery has important implications for future research on binary mosaic genodermatoses. This is especially true for some of the other proposed examples of nonallelic twin spotting, such as phacomatosis cesioflammea and phacomatosis spilorosea. Moreover, it seems still likely that the concept of allelic didymosis as proposed for the paired occurrence of nevus flammeus and nevus anemicus, mixed vascular nevus syndrome, and cutis tricolor will be corroborated by molecular studies.[5] There is no definitive therapy of this syndrome. Multi modality or multipronged approach can be used in the form of surgical excision, dermabrasion, Er:YAG laser and other ablative lasers to obtain optimum cosmetic outcome.
Our patient had nevus sebaceus and papular nevus spilus, both along the Blaschko's lines, mild scoliosis and palmoplantar/axillary hyperhidrosis. This presentation is atypical as speckled lentigines were in a segmental pattern instead of the characteristic checkerboard pattern and there was absence of muscle weakness, dysesthesia and neurological abnormalities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Happle R, Hoffmann R, Restano L, Caputo R, Tadini G. Phacomatosis pigmentokeratotica: A melanocytic-epidermal twin nevus syndrome. Am J Med Genet 1996;65:363-5.
[Google Scholar]
|
| 2. |
Tadini G, Ermacora E, Carminati G, Gelmetti C, Cambiaghi S, Brusasco A, et al. Unilateral speckled lentiginous nevus, contralateral verrucous epidermal naevus and diffuse ichthyosis-like hyperkeratosis: An unusual example of twin spotting? Eur J Dermatol 1995;5:659-63.
[Google Scholar]
|
| 3. |
Wollenberg A, Butnaru C, Oppel T. Phacomatosis pigmentokeratotica (Happle) in a 23-year-old man. Acta Derm Venereol 2002;82:55-7.
[Google Scholar]
|
| 4. |
Martínez-Menchón T, Mahiques Santos L, Vilata Corell JJ, Febrer Bosch I, Fortea Baixauli JM. Phacomatosis pigmentokeratotica: A 20-year follow-up with malignant degeneration of both nevus components. Pediatr Dermatol 2005;22:44-7.
[Google Scholar]
|
| 5. |
Happle R. Phacomatosis pigmentokeratotica is a “pseudodidymosis”. J Invest Dermatol 2013;133:1923-5.
[Google Scholar]
|
Fulltext Views
5,160
PDF downloads
3,116





