Translate this page into:
Phototherapy and photochemotherapy in childhood dermatoses
Correspondence Address:
Sunil Dogra
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160012
India
| How to cite this article: Dogra S, De D. Phototherapy and photochemotherapy in childhood dermatoses. Indian J Dermatol Venereol Leprol 2010;76:521-526 |
Abstract
The concept of phototherapy and photochemotherapy is not new, and sophisticated ultraviolet (UV) treatment modalities are available for almost three decades. However, phototherapy has not been used in children as extensively as in adults, probably due to long-term safety concerns. Photochemotherapy (psoralen plus UVA) is not considered to be safe in the younger age group. UV therapies can be useful treatment options for children with selected dermatological conditions provided they are used under carefully controlled conditions. Presently there is insufficient data available to provide recommendations regarding the safe maximum dose and duration of phototherapy in children. Developments of new UV delivery systems and devices are aimed at improving the safety and efficacy of phototherapy. In this review, we discuss the published literature on phototherapy and photochemotherapy in children, drawbacks of their use in pediatric population and future prospects.Introduction
Phototherapy refers to the use of ultraviolet (UV) radiation (ultraviolet A or B) without any exogenously used photosensitizer for the treatment of various dermatoses while photochemotherapy refers to the use of a sensitizer (psoralens) in addition.
Although psoralen + UVA (PUVA) has been used for vitiligo for centuries by ancient Egyptians and Indians, in modern medicine, the first clinical studies were performed by El Mofty in 1948. [1] In 1974, Parrish reported the useful role of artificial high-intensity UVA lamps and, thus, began the journey of modern PUVA therapy. [2] Fluorescent lamps (Philips TL 01) containing phosphor with peak narrow-band emission at 311 ± 2 nm (narrow-band UVB, NBUVB) was first clinically used by van Weelden et al.[3] and Green et al.[4] for the management of psoriasis in 1988.
The concept of phototherapy is not new and sophisticated UV treatment modalities are available for almost three decades. It is interesting to note that phototherapy in children has not been used as extensively as in adults for the dermatoses that are UV responsive. In this review, we discuss the published literature on phototherapy and photochemotherapy in children (excluding UVA1), drawbacks of its use and future prospects. The mechanism of action and treatment protocol of different phototherapy modalities do not form a content of this review.
Deterrents of Use of Phototherapy/Photochemotherapy in Children
The widespread use of phototherapy and photochemotherapy in children has been inhibited by safety concerns, particularly the risk of carcinogenicity and premature ageing on long-term UV therapy. An increased risk of melanoma and non-melanoma skin cancer (NMSC) is reported in adult patients receiving long-term UV therapy. [5],[6] As there are no such data in children, the information gathered in adults has been extrapolated to children. It has been observed that recurrent or prolonged erythemogenic UV exposure in early childhood increases the likelihood of development of melanoma and NMSC. [7],[8] Halder et al. did not encounter any malignancy in follow-up of 326 patients treated with PUVA for vitiligo. [9] They speculated that the risk of carcinogenicity may be disease specific, as patients with psoriasis requiring higher doses of psoralen and total cumulative dose of UVA for clearance of lesions are likely to be more predisposed. The risk of NMSC is related to patient race and type of phototherapy as well. Caucasians are more susceptible to develop malignancy, particularly squamous cell carcinoma (SCC), following PUVA treatment than Asians and Arabian-Africans. [10],[11]
The carcinogenic potential of PUVA therapy in psoriatic patients have most extensively been studied by Stern et al. in nearly 30,000 person-years. [12] A 100-fold increase in the incidence of SCC was observed in patients who received at least 337 PUVA exposures as compared to the normal control population drawn from the same locality. The risk of malignant melanoma is also increased, which is directly proportional to the degree of exposure. Persons receiving more than 250 exposures and at least 15 years after the first exposure were at an increased risk of developing melanoma. [13] The risk of developing various skin malignancies gets increased if immunosuppressive therapy is prescribed in addition to the PUVA therapy.
Overall, the risk of melanoma/NMSC is higher with all modes of photo/photochemotherapy. The risk is relatively well assessed in PUVA with long-term studies while the exact risk with NBUVB is yet to be determined with long-term data.
The risk of photodamage and carcinogenicity with UVA1 (high dose: 130 J/cm 2 , medium dose: 50-60 J/cm 2 , low dose: 10-20 J/cm 2 ) is not known. Therefore, a majority of the phototherapy experts do not recommend UVA1 therapy in subjects younger than 18 years of age. If used, it should not be more than two cycles yearly, with no more than 15 irradiation exposures per cycle. Patients should be monitored at least once a year for early detection of photodamage or skin cancer. [14]
Another problem is ensuring compliance with eye protection. The British Photodermatology Group recommends post-PUVA treatment eye protection for persons who are undergoing topical PUVA therapy for a dermatosis involving more than 30% body surface area, for systemic PUVA and for those who are being treated for atopic dermatitis (AD) as inherently they have an increased risk for cataract. [15] Therefore, they do not recommend PUVA below 10 years of age. [15]
Last but not the least is the practical difficulties. Healthcare facilities are always a daunting place for the youngsters. It is difficult to convince a small child to enter inside the phototherapy chamber. This problem in treating very young children was circumvented by allowing an attendant to accompany the child inside the phototherapy chamber with long sleeves/pants, protective eyewear on, and sunscreen application on photoexposed areas. [16] As phototherapy are largely hospital based, time consuming and requires regular travel to the healthcare facility, there is significant loss in terms of absenteeism from school for the patients as well as loss of working days for their attendants.
Phototherapy/Photochemotherapy in Children:Published Literature
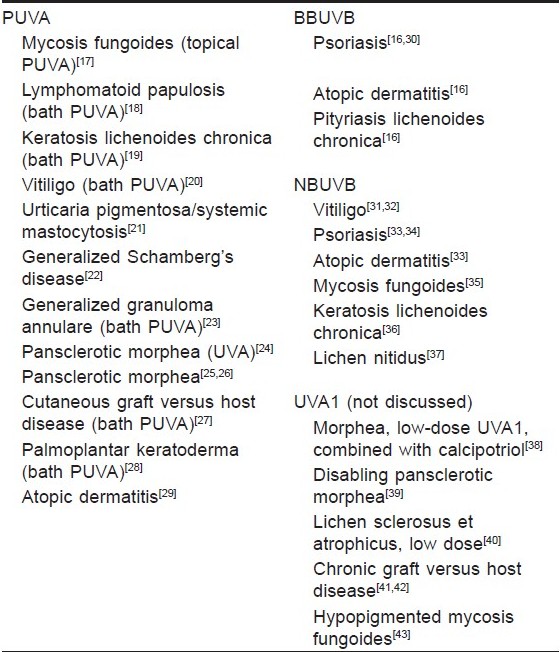
Systemic PUVA has not been used much in children. Most of the literature in this aspect appeared as case reports. Although NBUVB is considered to be safer in children, the experience with its use is limited, probably due to relatively recent introduction into the clinical practice. Literature on phototherapy in children from India is also not robust (vide infra). Different indications in which phototherapy/photochemotherapy has been used in children is listed in [Table - 1]. [16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43] We review here large case series (with ≥20 patients included) on the use of phototherapy in children in the chronological order of their publication.
Al-Fouzan et al.[30] treated 20 children with psoriasis, aged 5-12 years (mean, 9.6 years), with UVB. Eighty-eight percent of the patients responded while 12% failed the treatment (response aimed at 80% clearance). The mean cumulative dose of 3,315 mJ/cm 2 (range, 320-12,400 mJ/cm 2 ) and, on an average, 25 exposures (range, 9-50) over a period of 7.6 weeks (range, 2-20) were required for disease clearance. No serious side-effect was noted in any patient. One child had significant relapse within 6-months follow-up period, while none had serious side-effects.
Tay et al.[16] treated 20 children with psoriasis, AD and pityriasis lichenoides (PL), both acute and chronic, with BBUVB. Psoriasis patients (guttate, chronic plaque) had 30-60% body surface area involvement (mean 40%). The cumulative dose for disease clearance was 7.8 J/cm 2 (range, 1.9-16 J/cm 2 ) while the mean highest dose per exposure was 0.2 J/cm 2 (0.13-0.35 J/cm 2 ). The mean number of treatments required for disease clearance was 36 (range, 20-50), treatment sessions required being more in plaque than in guttate-type psoriasis. None developed serious side-effects. Five children with AD refractory to conventional treatment were treated thrice a week. None of the patients had complete clearance of disease, though all improved moderately, with reduction in the extent of eczema and severity of pruritus. The number of treatments received ranged from 20 to 61 (mean, 41) over 7-20 weeks (mean, 15 weeks). The mean cumulative dose of UVB ranged from 2.39 to 7.78 J/cm 2 (mean, 5.6 J/cm 2 ). Five patients of PL received thrice-weekly UVB and all had remission with an average of 26 treatments (range, 22-33) over 8-16 weeks (mean, 11 weeks). The total cumulative dose of UVB ranged from 2.96 to 4.98 J/cm 2 (mean, 4.2 J/cm 2 ), with mean highest dose per exposure being 0.23 J/cm 2 (range, 0.21-0.25 J/cm 2 ).
Njoo et al. treated 51 patients of generalized vitiligo with NBUVB twice weekly over a period of 1 year. [31] More than 75% repigmentation was observed in 53% of the patients while the disease activity was stabilized in 80%. Complete repigmentation was observed in only 6% of the patients. Patients who did not respond to other therapeutic modalities previously showed excellent repigmentation with NBUVB. No relationship was observed between the degree of repigmentation and the variables like age, sex, skin type, positive family history, duration of disease, vitiligo disease activity score (VIDA) and extent of depigmentation. Itching and xerosis were the only side-effects observed in 8% and 4% patients, respectively. However, study design was not appropriate to assess the long-term safety of NBUVB.
Kanwar and Dogra from India treated 26 children with vitiligo using NBUVB, 20 of whom completed the study period of 1 year. [32] Seventy-five percent of the patients had marked to complete response, 20% had moderate response and 5% had mild repigmentation. Fifty percent repigmentation was achieved after 34 treatment sessions on an average. Perifollicular pigmentation was the prominent pattern observed in 65% of the patients. Most of them had concomitant marginal and/or diffuse pigmentation. Adverse effects were minimal and did not warrant discontinuation of treatment. Twenty percent developed lesional burning or pruritus while 15% complained of xerosis.
Jury et al. reviewed the use of NBUVB in the pediatric population. [33] Of the 77 children (4-16 years) enrolled, 45% had psoriasis and 32% had AD. Other dermatoses treated were alopecia areata, acne, hydroa vacciniforme and polymorphic light eruption. Sixty three-percent of the psoriasis patients had marked improvement while 9% had no improvement. Sixty-eight percent and 16% of the atopics had marked and no improvement, respectively. Of the photodermatoses, response was disappointing in hydroa vacciniforme. Poor response was observed in alopecia areata as well. Median number of treatment sessions was higher for AD compared to psoriasis (24 vs. 17.5). The side-effect profile was similar to that commonly observed in adults: erythema in 30%, blistering in 5%, reactivation of herpes simplex in 2%, and varicella zoster in 1%. They noted that while comparing response to treatment in a particular disease group, adults had a much better response compared to children. The authors hypothesized that the concern for long-term safety might have prevented administration of NBUVB in children with mild or moderate disease. Thus, selection of children with severe disease only for phototherapy skewed the response rate in favor of adults.
The efficacy of NBUVB in psoriasis in adults has been proven and, in comparison to BBUVB, it elicits faster clearance of lesions, fewer episodes of erythema and longer remission. However, large studies on phototherapy in childhood psoriasis are rare. This is particularly true in the Indian context. Jain et al.[34] treated 20 patients with psoriasis (plaque psoriasis 18, guttate psoriasis 2) aged between 6 and 14 years with NBUVB. In a twice-weekly treatment regimen, the mean cumulative dose required for clearance was 4286 mJ/cm 2 (1,687-7,509 mJ/cm 2 ) over a mean number of treatment sessions of 24 (17-30). The highest dose per treatment was 329 mJ/cm 2 (165-462 mJ/cm 2 ). The age of the patients as well as the duration and extent of disease did not influence the cumulative UV dose, highest dose per treatment and number of treatments required for clearance. Over a treatment period of 12 weeks, 60% patients had excellent response, 15% had good response, 5% had moderate response and 10% had no response. Two patients withdrew from the study due to practical difficulties and two developed erythroderma. Mild erythema was observed in 10% of the patients. Within 6 months post-treatment follow-up, only one patient relapsed and required a second course of phototherapy. They concluded that NBUVB phototherapy may be a safe and effective treatment choice for childhood psoriasis ahead of more toxic systemic therapies.
Ersoy-Evans et al. treated 113 patients (aged 13-17 years, median 13 years) with different phototherapy modalities including UVB, NBUVB, PUVA and topical PUVA. [44] The dermatoses that were treated included psoriasis, PLC, vitiligo, alopecia areata and others. In psoriasis, desired response was achieved in 93% of the patients treated with NBUVB, 83.3% with PUVA and 93.3% with UVB, requiring a mean number of 16, 28 and 18.5 treatments, respectively. Of the 18 patients with PLC, 66.7% were treated with BBUVB, 27.8% with NBUVB and 5.6% with PUVA. Response was achieved in 83.3% of the patients treated with BBUVB after a mean of 18 treatment sessions. The corresponding figures in the NBUVB group were 100% and 22. The patient on PUVA did not respond to treatment. Of 26 children with vitiligo, 34.6% and 30.8% patients were treated with NBUVB and PUVA, respectively, while the rest were treated with topical methoxalen and UVA. More than 50% repigmentation was observed in 57% of the patients treated with PUVA and 50% with NBUVB in a median number of 24.5 and 15 treatment sessions, respectively. Results with topical photochemotherapy were not encouraging. Response of alopecia areata to PUVA or UVA was overall disappointing. Among all the patients treated with different treatment modalities, erythema was observed in 51.6%, and it was the most common side-effect noted. Seventy-six percent, 40% and 33% patients in the NBUVB, BBUVB and PUVA groups, respectively, had erythema. Pruritus and burning occurred in 18% and 9% of all patients, respectively.
In a recently published side to side comparison study by Jain et al. from India, it was shown that pre-radiation mineral oil application improved the efficacy of NBUVB in treatment of childhood psoriasis. [45] The mean cumulative dose for clearance in the mineral oil pre-treated side was 2,956 mJ/cm 2 compared to 4,088 mJ/cm 2 in the non-pre-treated side. The mean maximum dose and number of exposures for clearance on the emollient pre-treated side were 297 mJ/cm 2 and 20.56, respectively, while the corresponding figures in the non-pre-treated side were 394 mJ/cm 2 and 23.78. This beneficial effect of mineral oil has been attributed to its refractive index, similar to that of stratum corneum, and its ability to penetrate and fill the air-corneocyte interfaces thus decreasing backscattering or reemission of the incident light. This observation was not supported by another study and thus needs further evaluation. [46] However, it is not clear from their study how the lesion-free side was protected from exposure to NBUVB when the other side was still being treated.
This review has certain limitations. The relevant literature reviewed is not robust, most of which were retrospective studies with short post-treatment follow-up. Indication of the use of phototherapy/photochemotherapy and selection criteria based on the severity of disease was not uniform. Varied criteria were used to assess response to treatment.
Recent Developments
Targeted phototherapy (concentrated/focused phototherapy, microphototherapy) is the most recent and promising method of delivery of light, in which the light energy is directly focused on the lesion. Many of the problems associated with phototherapy in children can be circumvented by the use of this modality. Uninvolved areas are not exposed and hence remain free of immediate and long-term potential side-effects of UV light. Delivery of light energy is quick and supraerythemogenic doses can be used. In this manner, duration of individual treatment sessions can be decreased and remission can be achieved faster. [47] These new methods and devices are aimed at improving the safety and efficacy of phototherapy. As the machine is hand-held, it may be less frightening to a young soul. However, there are certain disadvantages, e.g. cost of treatment, and it cannot be used in dermatoses involving extensive body surface area (>10%).
Phototherapy/Photochemotherapy in Children:Where do we Stand?
Phototherapy has a useful role, particularly in the treatment of psoriasis, vitiligo and AD. The concern of phototherapy causing premature aging or carcinogenesis in younger individuals has not been yet adequately addressed. As of today, if phototherapy is indicated for a particular dermatosis, NBUVB remains the safest bet in children due to its relatively less side-effect profile and non-requirement for post-treatment sun and eye protection. Most of the long-term side-effects of phototherapy are dose related. Therefore, it is proposed that the maximum duration of NBUVB phototherapy in children should be 12 months. If NBUVB is required for a longer period, limited areas bearing active lesions can be exposed. Indiscriminate use of any form of phototherapy without proper and pressing indications is not justified. If long-term use of phototherapy is anticipated for disease control, phototherapy should be preferably substituted by any other available safer alternative.
| 1. |
El Mofty AM. A preliminary clinical report on the treatment of leucoderma with Ammi majjus Linn. J Eygpt Med Assoc 1948;31:651-65.
[Google Scholar]
|
| 2. |
Parish JA, Fitzpatrick TB, Tanenbaum L, Pathak MA. Photochemotherapy of psoriasis with oral methoxsalen and long wave ultraviolet light. N Eng J Med 1974;291:1207-11.
[Google Scholar]
|
| 3. |
Van Weelden H, Baart de la Faille H, Young E, van der Leun JC. A new development in UVB phototherapy for psoriasis. Br J Dermatol 1988;119:11-9.
[Google Scholar]
|
| 4. |
Green C, Ferguson J, Lakshmipathi T, Johnson BE. 311 nm UVB phototherapy: an effective treatment for psoriasis. Br J Dermatol 1988;119:691-6.
[Google Scholar]
|
| 5. |
Stern RS. The risk of melanoma in association with long-term exposure to PUVA. J Am Acad Dermatol 2001;44:755-61.
[Google Scholar]
|
| 6. |
Stern RS, Lange R. Non-melanoma skin cancer occurring in patients treated with PUVA five to ten years after first treatment. J Invest Dermatol 1988;91:120-4.
[Google Scholar]
|
| 7. |
Holman CD, Armstrong BK. Cutaneous malignant melanoma and indicators of total accumulated exposure to the sun: an analysis separating histogenic types. J Natl Cancer Inst 1984;73:75-82.
[Google Scholar]
|
| 8. |
Holly EA, Aston DA, Cress RD. Cutaneous melanoma in women: I. Exposure to sunlight, ability to tan, and other risk factors related to ultraviolet light. Am J Epidemiol 1995;141:923-33.
[Google Scholar]
|
| 9. |
Halder RM, Battle EF, Smith EM. Cutaneous malignancies in patients treated with psoralen photochemotherapy (PUVA) for vitiligo. Arch Dermatol 1995;131:734-5.
[Google Scholar]
|
| 10. |
Stern RS, Laird N. Photochemotherapy follow-up study. The carcinogenic risks of treatments for severe psoriasis. Cancer 1994;73:2759-64.
[Google Scholar]
|
| 11. |
Murase JE, Lee EE, Koo J. Effect of ethnicity on the risk of developing nonmelanoma skin cancer following long-term PUVA therapy. Int J Dermatol 2005;44:1016-21.
[Google Scholar]
|
| 12. |
Stern RS, Laird N, Melski J, Parrish JA, Fitzpatrick TB, Bleich HL. Cutaneous squamous-cell carcinoma in patients treated with PUVA. N Engl J Med 1984;310:1156-61.
[Google Scholar]
|
| 13. |
Stern RS, Nichols KT, Vakeva LH. Malignant melanoma in patients treated for psoriasis with methoxsalen (psoralen) and ultraviolet A radiation (PUVA). The PUVA follow up study. N Engl J Med 1997;336:1041-5.
[Google Scholar]
|
| 14. |
Simon JC, Pfieger D, Schopf E. Recent advances in phototherapy. Eur J Dermatol 2000;10:642-5.
[Google Scholar]
|
| 15. |
British Photodermatology Group. British photodermatology group guidelines for PUVA. Br J Dermatol 1994;130:246-55.
[Google Scholar]
|
| 16. |
Tay Y, Morelli JG, Weston WL. Experience with UVB phototherapy in children. Pediatr Dermatol 1996;13:406-9.
[Google Scholar]
|
| 17. |
Pabsch H, Rόtten A, Von Stemm A, Meigel W, Sander CA, Schaller J. Treatment of childhood mycosis fungoides with topical PUVA. J Am Acad Dermatol 2002;47:557-61.
[Google Scholar]
|
| 18. |
Volkenandt M, Kerscher M, Sander C, Meurer M, Rocken M. PUVA-bath photochemotherapy resulting in rapid clearance of lymphomatoid papulosis in a child. Arch Dermatol 1995;131:1094.
[Google Scholar]
|
| 19. |
Remling R, Schnopp C, Schmidt T, Hein R, Ring J, Abeck D. Keratosis lichenoides chronica. Bath PUVA therapy. Hautarzt 2002;53:550-3.
[Google Scholar]
|
| 20. |
Mai DW, Omohundro C, Dijkstra JW, Bailin PL. Childhood vitiligo successfully treated with bath PUVA. Pediatr Dermatol 1998;15:53-5.
[Google Scholar]
|
| 21. |
Godt O, Proksch E, Streit V, Christophers E. Short- and long-term effectiveness of oral and bath PUVA therapy in urticaria pigmentosa and systemic mastocytosis. Dermatology 1997;195:35-9.
[Google Scholar]
|
| 22. |
Milea M, Dimov HA, Cribier B. Generalized Schamberg's disease treated with PUVA in a child. Ann Dermatol Venereol 2007;134:378-80.
[Google Scholar]
|
| 23. |
Batchelor R, Clark S. Clearance of generalized papular umbilicated granuloma annulare in a child with bath PUVA therapy. Pediatr Dermatol 2006;23:72-4.
[Google Scholar]
|
| 24. |
Yildirim M, Baysal V, Aridogan BC, Kesici D, Erturan I. Pansclerotic morphea treated with UVA: a case report. J Dermatol 2003;30:625-7.
[Google Scholar]
|
| 25. |
Todd DJ, Askari A, Ektaish E. PUVA therapy for disabling pansclerotic morphoea of children. Br J Dermatol 1998;138:201-2.
[Google Scholar]
|
| 26. |
Scharffetter-Kochanek K, Goldermann R, Lehmann P, Hφlzle E, Goerz G. PUVA therapy in disabling pansclerotic morphoea of children. Br J Dermatol 1995;132:830-1.
[Google Scholar]
|
| 27. |
Bonanomi S, Balduzzi A, Tagliabue A, Biagi E, Rovelli A, Corti P, et al. Bath PUVA therapy in pediatric patients with drug-resistant cutaneous graft-versus-host disease. Bone Marrow Transplant 2001;28:631-2.
[Google Scholar]
|
| 28. |
Kaskel P, Leiter U, Krahn G, Schiener R, Pillekamp H, Peter RU, et al. PUVA-bath photochemotherapy for congenital palmoplantar keratoderma in an 11-year-old girl. Br J Dermatol 2000;143:464-5.
[Google Scholar]
|
| 29. |
Sheehan MP, Atherton DJ, Norris P, Hawk J. Oral psoralen photochemotherapy in severe childhood atopic eczema: an update. Br J Dermatol 1993;129:431-6.
[Google Scholar]
|
| 30. |
Al- Fouzan AW, Nanda A. UVB phototherapy in childhood psoriasis. Pediatr Dermatol 1995;12:66.
[Google Scholar]
|
| 31. |
Njoo MD, Bos JD, Westerhof W. Treatment of generalized vitiligo in children with narrow-band (TL-01) UVB radiation therapy. J Am Acad Dermatol 2000;42:245-53.
[Google Scholar]
|
| 32. |
Kanwar AJ, Dogra S. Narrow- band UVB for the treatment of generalized vitiligo in children. Clin Exp Dermatol 2005;30:332-6.
[Google Scholar]
|
| 33. |
Jury CS, McHenry P, Burden AD, Lever R, Bilsland D. Narrowband ultraviolet B (UVB) phototherapy in children. Clin Exp Dermatol 2006;31:196-9.
[Google Scholar]
|
| 34. |
Jain VK, Aggarwal K, Jain K, Bansal A. Narrow-band UV-B phototherapy in childhood psoriasis. Int J Dermatol 2007;46:320-2.
[Google Scholar]
|
| 35. |
Kavala M, Zindanci I, Bόyόkbabani N, Tόrkoglu Z, Kocatόrk E, Can B. Treatment of childhood mycosis fungoides with narrow-band phototherapy. Int J Dermatol 2009;48:203-4.
[Google Scholar]
|
| 36. |
Tomb R, Soutou B. Keratosis lichenoides chronica in two siblings with marked response to UVB phototherapy. Ann Dermatol Venereol 2008;135:835-8.
[Google Scholar]
|
| 37. |
Do MO, Kim MJ, Kim SH, Myung KB, Choi YW. Generalized lichen nitidus successfully treated with narrow-band UVB phototherapy: two cases report. J Korean Med Sci 2007;22:163-6.
[Google Scholar]
|
| 38. |
Kreuter A, Gambichler T, Avermaete A, Jansen T, Hoffmann M, Hoffmann K, et al. Combined treatment with calcipotriol ointment and low-dose ultraviolet A1 phototherapy in childhood morphea. Pediatr Dermatol 2001;18:241-5.
[Google Scholar]
|
| 39. |
Gruss C, Stόcker M, Kobyletzki G, Schreiber D, Altmeyer P, Kerscher M. Low dose UVA1 phototherapy in disabling pansclerotic morphoea of childhood. Br J Dermatol 1997;136:293-4.
[Google Scholar]
|
| 40. |
Kreuter A, Jansen T, Stόcker M, Herde M, Hoffmann K, Altmeyer P, et al. Low-dose ultraviolet-A1 phototherapy for lichen sclerosus et atrophicus. Clin Exp Dermatol 2001;26:30-2.
[Google Scholar]
|
| 41. |
Kowalzick L, Artlett CM, Thoss K, Baum HP, Ziegler H, Mischke D, et al. Chronic graft-versus-host-disease-like dermopathy in a child with CD4+ cell microchimerism. Dermatology 2005;210:68-71.
[Google Scholar]
|
| 42. |
Ziemer M, Thiele JJ, Gruhn B, Elsner P. Chronic cutaneous graft-versus-host disease in two children responds to UVA1 therapy: improvement of skin lesions, joint mobility, and quality of life. J Am Acad Dermatol 2004;51:318-9.
[Google Scholar]
|
| 43. |
Roupe G. Hypopigmented mycosis fungoides in a child successfully treated with UVA1-light. Pediatr Dermatol 2005;22:82.
[Google Scholar]
|
| 44. |
Ersoy- Evans S, Altaykan A, Sahin S, Kolemen F. Phototherapy in childhood. Pediatr Dermatol 2008;25:599-605.
[Google Scholar]
|
| 45. |
Jain VK, Bansal A, Aggarwal K, Jain K. Enhanced response of childhood psoriasis to narrow-band UV-B phototherapy with preradiation use of mineral oil. Pediatr Dermatol 2008;25:559-64.
[Google Scholar]
|
| 46. |
George SA, Bilsland DJ, Wainwright NJ, Ferguson J. Failure of coconut oil to accelerate psoriasis clearance in narrow-band UVB phototherapy or photochemotherapy. Br J Dermatol 1993;128:301-5.
[Google Scholar]
|
| 47. |
Morita A, Weiss M, Maeda A. Recent developments in phototherapy: Treatment methods and devices. Recent Pat Inflamm Allergy Drug Discov 2008;2:105-8.
[Google Scholar]
|
Fulltext Views
6,414
PDF downloads
2,345





